Neonatal jaundice is the commonest abnormal physical finding in the newborn nursery and haemolytic disease of the newborn (HDN) among babies born to Rh negative mothers is the most formidable etiology [1]. The incidence of HDN depends upon the proportion of the population who are Rh negative. Before immunoprophylaxis was available, HDN affected 1% of all newborns and was responsible for the death of one baby in every 2,200 births [2]. Anti-D prophylaxis and advances in neonatal care have reduced the frequency of HDN by almost a factor of 10 to 1 in 21,000 births. Deaths attributed to RhD alloimmunisation fell from 46/100,000 births before 1969 to 1.6/100,000 in 1990 [3]. This may not be entirely attributable to immunoglobulin; changes in abortion rates and racial composition may also play a part.
This study was undertaken to study the current trends in presentation, management and outcome of hyperbilirubinemia among newborns delivered to Rh negative mothers.
Methods
This observational descriptive study with prospective data collection was conducted at neonatal services of Kempegowda Institute of Medical Sciences Hospital between November 2005 and April 2007. One hundred live born term babies born to Rh negative mothers in Kempegowda Institute of Medical Sciences Hospital were included in the study after obtaining parental informed consent. Using a predesigned proforma antenatal and natal data was recorded. Cord blood was collected during delivery for assessment of bilirubin, hematocrit and direct Coombs test. In babies with clinical jaundice, serum bilirubin levels were estimated 8 hourly till bilirubin levels reduced to normal levels. Babies were also investigated to rule out other causes of jaundice and excluded from the study if found. Babies not requiring treatment for hyperbilirubinemia were monitored clinically twice a day till discharge. Following discharge babies were followed up once a week for one month. Descriptive statistics was used to find the significant association of incidence of jaundice / hyperbilirubinemia and study characteristics. The study protocol was approved by the institute ethics committee.
Results
In the present clinical study, out of 100 babies enrolled in to the study, 57 babies were delivered per vaginally and 43 babies were delivered by caesarean section. Sixty babies were born to multiparous mothers [Table/Fig-1]. In the present study, there were 40 mothers with O-ve blood group, 32 with A-ve blood group, 26 with B -ve blood group and 2 with AB-ve blood group. Out of 100 babies, there were 59 male and 41 female babies. There were 20 babies weighing <2500 gms and 4 babies weighing >3500 gms. There were 24 babies with Rh -ve blood groups out of which there were 9 babies with O-ve blood group, 8 babies with A-ve blood group, 6 babies with B-ve blood group and 1 baby with AB-ve blood group. There were 76 babies with Rh +ve blood group of which there were 25 babies with O +ve blood group, 23 babies each with A +ve and B +ve blood groups and 5 babies with AB +ve blood group. There were 60 multiparous mothers out of which 38(63.3%) had received Anti-D and 22(36.7%) had not received Anti-D.
A Study of Neonatal Jaundice in Babies Born to Rh-ve Mothers
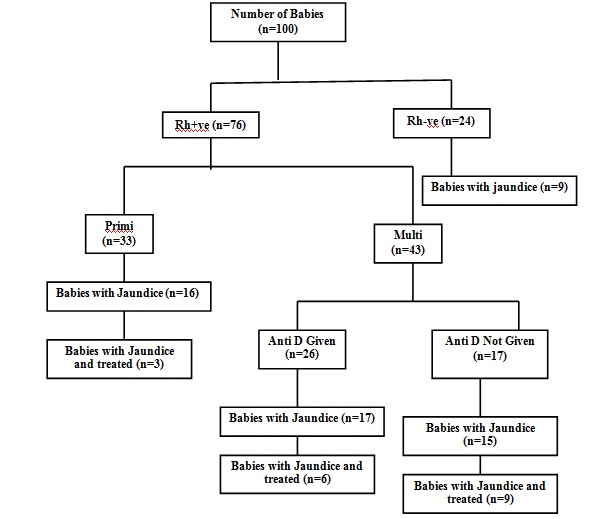
Out of 100 babies, 57 babies developed jaundice and in 43 babies there was no jaundice. Jaundice was 2.7 times more likely associated with babies born to multiparous Rh-ve mothers (p=0.017). Jaundice was 2.9 times more likely associated with Rh+ve babies born to Rh-ve mothers (p=0.027). Jaundice was 3 times more likely associated with Rh+ve babies born to multiparous mothers (p=0.020). Jaundice was 3.97 times more likely associated with Rh+ve babies born to multiparous mothers who have not received Anti-D (p=0.154). In the present study, out of the 3 babies born to multiparous mothers in whom direct coombs test was positive, 2 babies had cord blood hemoglobin level of <11gm% with cord blood bilirubin level of >4.5mg%. Exchange transfusion was done in these 2 babies with subsequent phototherapy. One more baby had cord blood bilirubin level of >4.5mg% with cord blood hemoglobin level >11gm%. In this case, the mother’s blood group was O-ve and the baby was B+ve. This baby was treated with double surface phototherapy only.
Among 57 babies with jaundice, 22 babies (38.6%) received treatment and rest 35 babies (61.4%) did not receive any treatment. Treatment for jaundice was required 3.8 times more likely in Rh+ve babies born to multiparous mothers (p=0.058). Treatment of jaundice was required 2.75 times more likely in Rh+ve babies born to multiparous mothers without history of Anti-D administration in the past than those who received Anti-D (p=0.162). Duration of phototherapy was significantly more in Rh+ve babies born to multiparous mothers (p=0.0002). Duration of phototherapy was significantly more in Rh+ve babies born to multiparous mothers who had not received Anti-D (p=0.0097).
Discussion
This study was done to evaluate the current trends in presentation, management and outcome of hyperbilirubinemia among newborns delivered to Rh negative mothers. The incidence of Rh-ve blood group in India is 5-10% [4]. A total of 2257 mothers delivered during the study period in our hospital. There were 124 babies delivered to mothers with Rh-ve blood group during this period. This accounts for 5.5% of total number of mothers who delivered during this period. Out of the 124 babies born to Rh-ve mothers 100 babies satisfying the criteria were included in the study.
In the present study, majority (76%) of the babies were Rh+ve and the rest were Rh-ve. This is similar to the finding (74%) in the study conducted by Locham KK, Sodhi M and Singh M [5]. In the present study, there were 60 multiparous mothers out of which 38 (63.3%) had received Anti-D and 22 (36.7%) had not received Anti-D. In a study conducted by Fawole AO et al., [6] in 2001 Anti-D immunoprophylaxis rate was poor (44.8%) among multiparous mothers. The majority of mothers who declined immunoprophylaxis did so for financial reasons. We can observe that the Anti-D immunoprophylaxis rate is increasing over the years.
In our study, 57% of the babies developed jaundice. A similar observation was made in a study conducted by Sharma J, Sharma P and Bahl L [7]. In a similar study done by Locham KK, Sodhi M and Singh G [5], jaundice was observed in 54% of babies. A majority (61.4%) of babies did not receive any treatment in our study. A similar observation (74%) was made in the other study compared [5]. Treatment of jaundice was 2.75 times more likely in Rh+ve babies born to multiparous mothers who have not received Anti-D than in those babies born to multiparous mothers who have received Anti-D. This proves the efficacy of Anti-D in management of Rh isoimmunization. The duration of phototherapy was significantly more in Rh+ve babies born to multiparous mothers who had not received Anti-D than in those born to multiparous mothers who had received Anti-D.
In our study (2006), 66.6% of the babies with Rh incompatibility required exchange transfusion which is similar to the study conducted by Rasul et al., [8]. Almost 90 % and 60 % of babies with Rh incompatibility required exchange transfusion in studies conducted by Narang et al., [9] and Singhal et al., [3] respectively. These wide variations in the values in different studies may be due to different protocols for treatment of Rh incompatibility and also due to small sample size, i.e., 2 out of 3 babies in the present study,15 out of 23 babies in study conducted by Rasul et al., and 13 out of 14 babies in the study conducted by Narang et al., and 21 out of 37 babies in the study conducted by Singhal et al., required exchange transfusion.
The incidence of hemolytic disease of the newborn reflects the frequency of Rh negativity in a population. Existing data suggest that the risk of Rh isoimmunization when immunoprophylaxis is not administered is 16% if Rh-positive fetuses are ABO compatible with their Rh-negative mothers, 1.5% to 2% if ABO incompatible, 4% to 5% after therapeutic abortion, and 2% after spontaneous abortion [10]. In the present study, the incidence of Rh isoimmunization was 17.6% which is comparable to the above mentioned data.
We conclude that, although the overall incidence of Rh isoimmunization has declined dramatically over the last decade, it is still an important cause of neonatal morbidity and mortality. Exchange transfusion is frequently used in cases of Rh incompatibility even today. This emphasizes the need for more vigorous preventive efforts and up-to-date management skills.