Anaemia in pregnancy is now considered as a major health problem. This commonest haematological problem in pregnancy, caused by iron deficiency, is seen in 90% of cases. According to WHO estimation, the prevalence of anaemia in pregnant women is 14% in developed countries, it is 51% in developing countries and it is 65-75% in India [1]. India contributes to about 80% of the maternal deaths caused by anaemia in South Asia [2]. As per the guidelines proposed by the expert group of World Health Organization, anaemia is considered to exist when haemoglobin level is below 11gm/dl in pregnant women [3]. Most of the reported anaemia mothers are in third trimester of pregnancy, since the iron demand reaches 6.6 mg/day in this period. There is an increase in plasma volume and red cell mass, especially in third trimester. But the disproportionate increase in plasma volume causes haemodilution and it lowers the haemoglobin level.
Although the antenatal mothers were attending the antenatal clinics and regularly taking iron and folic acid tablets, the prevalence of anaemia was still in higher in these groups [4]. So, the cause of anaemia should be attributed to mainly nutritional deficiency, poor intake of iron rich food stuff, worm infestations, repeated pregnancies in a short interval of time, absence of replenishing of the iron stores lost due to menstrual loss, etc, [3,5]. Maternal anaemia is often associated with increased risk of maternal and foetal morbidity and mortality [2]. So, the only way to reduce these complications is early screening for anaemia and giving proper, effective treatment and counseling about the same.
This study was undertaken among the booked antenatal mothers in last trimester who were attending the antenatal clinic in our hospital. The main aim of the study was to evaluate the number of anaemic cases and type of anaemia among them. Our study also included any complications which occurred in the antenatal period and during delivery and postnatal outcomes of these cases.
Material and Methods
This cross sectional, descriptive study was carried out in the Department of Clinical Pathology in association with Department of Pharmacology at Sri Manakula Vinayagar Medical College and Hospital, Pondicherry, India. This was a prospective study conducted over a period of two months in 2010. All the booked antenatal mothers of third trimester, attending antenatal clinic, in the age group of 19–40 years, were included in the study. Those who refused to give consent, HIV positive women, and those with symptomatic infections were excluded from the study. Written informed consents were obtained from each patient for their participation, after the nature of the study was explained to them in their language. This study was approved by the institutional ethics committee.
A structured questionnaire was administered to all the study individuals. The information on age, age at marriage, average per capita income, educational status, age at first pregnancy, parity, gestational age, interval between previous and index pregnancies, number of abortions, iron-folic acid tablets supplementation, etc was collected. After clinical examination, blood samples were collected in Ethylene Diaminete Traacetic Acid (EDTA) tubes in the clinicopathology lab. Haemoglobin estimation was done by Sahli’s Haemoglobinometer method. Typing of anaemia was done as per standard peripheral blood smear examination method [3]. The World Health Organization criteria for typing anaemia in pregnancy were adopted in this study. According to WHO criteria, the degree of anaemia was classified as mild- 8-10g%, moderate – 7-8g%, severe –below 7g%. Based on their education, occupation status and family income per month, antenatal mothers were categorized as class 1-upper class, class 2- upper middle class, class 3 - lower middle class, class 4–upper lower class, class 5–lower class according to Kuppuswamy’s socio-economic status scale, 2012 [6]. Educational status of these mothers was classified as illiterate, upto 5th, upto 10th, upto 12th and graduates.
Participants were followed up till delivery. During delivery period, babies’ birth outcomes such as weight, APGAR, length, head circumference, as well as still birth, mode of delivery, gestation age at delivery were recorded. Maternal complications were also recorded. The data were collected and analyzed by using computer software Statistical Package for Social Science (SPSS), version 11.0 and results were expressed in percentage.
Results
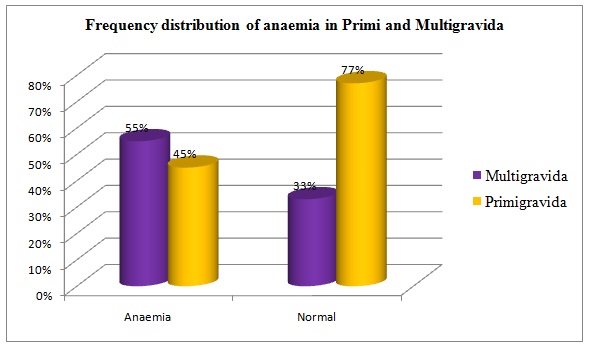
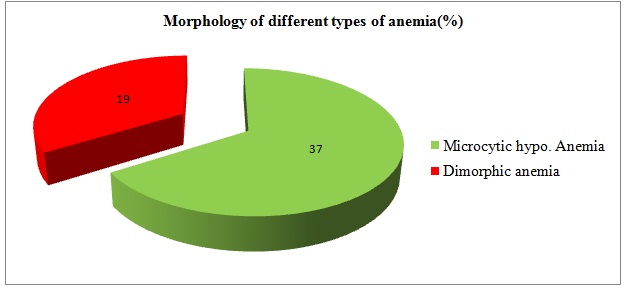
A total of seventy five pregnant women attending the Antenatal Clinic constituted the study population. All the pregnant women in third trimester in the study group were in the age of group of 19- 40 years. It was found that out of 75 mothers studied, 62 cases (83%) showed Hb level of less than 10g%. Only 17% showed Hb levels of more than 11g%. Age wise distribution of anaemia among the study population has been shown in [Table/Fig-1], which showed that majority (41 cases) of the pregnant women were 23-27 years of age. All the eight cases who were around 30 years of age were reported to have anaemia. Similarly, twenty three cases in age group of 20 years were reported to have anaemia (87%). Around 55% multi–gravid mothers reported anaemia in comparison with 45% primi–gravida who showed anaemia. This finding was further emphasized by the fact that 77% primigravida were non–anaemic in third trimester [Table/Fig-2].The Peripheral Blood Smear (PBS) identified microcytic hypochromic and dimorphic blood picture to be most common morphological variant of anaemia. Smears showed microcytic hypochromic anaemia in 37% cases and dimorphic anaemia in 19% cases [Table/Fig-3]. Remaining 27% cases showed normal blood smear report on RBC morphology.
Age wise distribution of anaemia
| Age | Total cases | Anaemia cases | % anaemia cases |
|---|
| 19-22 | 26 | 23 | 87% |
| 23-27 | 41 | 31 | 68% |
| 28-32 | 6 | 6 | 100% |
| >33 | 2 | 2 | 100% |
Frequency distribution of anaemia in Primi–gravida and Multi–gravida
FMorphology of different types of anaemia(%)
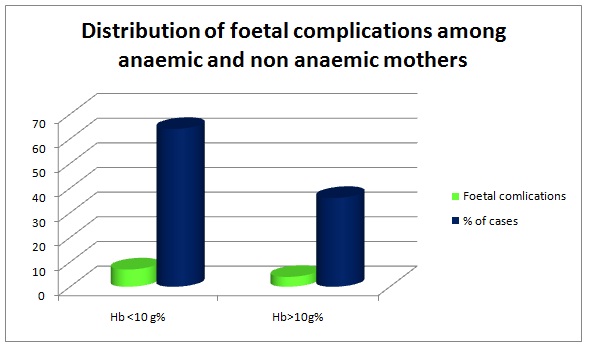
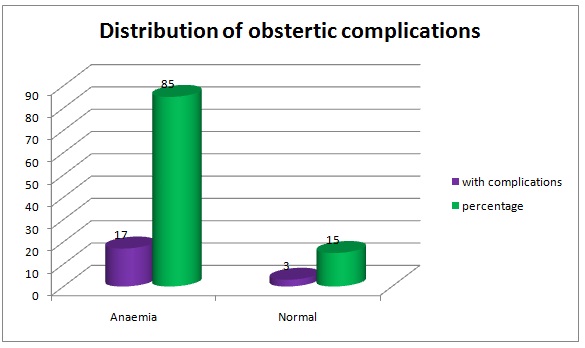
[Table/Fig-4] showed that 50 cases out of 75 cases were under Class V and Class IV, that is low socio–economic status groups. On an average, 88 % of anaemia cases were seen in Class V and Class IV. No anaemia cases were reported in class I. Two anaemia cases were reported in class II and twelve anaemia cases were reported in class III socio-economic status. Anaemia was significantly higher (100%) in illiterates and in those who had primary education only [Table/Fig-5]. Among 20 cases who presented with antenatal complications, 17 were found to be anaemic, that is, obstetric complications were seen in 85% of anaemic mothers. The other maternal complications were prolonged labour, uterine inertia and postpartum haemorrhage and one case had disseminated intravascular coagulation. Foetal distress was present in seven reported cases among anaemic cases of the study group [Table/Fig-6 and 7].
Distribution of anaemia in different Socio economic groups
| Socio–economic class | Total | Anaemia | %anaemia |
|---|
| V | 42 | 38 | 90% |
| IV | 12 | 10 | 85% |
| III | 16 | 12 | 75% |
| II | 5 | 2 | 40% |
| I | 0 | 0 | 0 |
Association of anaemia with educational status
| Education | Total | Anaemia | %Anaemia |
|---|
| Illiterate | 6 | 6 | 100 |
| Upto 5th | 2 | 2 | 100 |
| Upto10th | 46 | 42 | 90 |
| Upto12th | 14 | 12 | 86 |
| Graduate | 11 | 4 | 86 |
Distribution of foetal complications among anaemic and non anaemic mothers
Distribution of obstetric complications
Discussion
India contributes about 80% of the maternal deaths caused by anaemia in south Asia [2]. In addition, maternal anaemia is considered as a risk factor for poor pregnancy outcomes and it threatens the life of foetus also. Even more presently, it has been found that more than half of the world’s population will experience some form of anaemia in their lifetime. This study which was conducted in our hospital, included 75 antenatal cases in last trimester, who were booked and were regularly taking iron and folic acid tablets.
According to our study, it was found that 83% of cases had Hb levels of less than 10 g%. Only 17% had Hb of more than 10 g%, even with intake of iron supplements. Among them, majority were in the age group of 23-27 years, as was seen in a study conducted by Viveki et al., [7]. Moreover, there was a high rate of maternal anaemia from age of 28 years onwards and above 33 years of age. WHO recorded that anaemia was significantly high in the third trimester of pregnancy than in other two trimesters [8]. Our study also indicated the same. Studies supporting low prevalence of maternal anaemia in Southern India, West Bengal and Kerala also exist (40% and 5%) [9]. The iron requirement in pregnancy is approximately 600mg (foetal and placental deposits+basal losses) and the demand for iron which arises from expansion of red blood mass (haemodilution) is 500 mg, or total of 1070mg is needed [10]. The daily requirement of iron in early pregnancy is about 2.5 mg/day and in late pregnancy, it is about 6 mg/day. Iron deficiency may be caused by menstrual loss, inadequate diet, or a previous recent pregnancy. Among 83% of anaemic cases, microcytic hypochromic anaemia was presented in 37% cases, indicating iron deficiency anaemia. The predominant findings of microcytic hypochromic anaemia were consistent with those of Virender et al., [11]. Another 19% showed dimorphic anaemia, indicating that there was marrow response to iron treatment or impending deficiency for iron. So, around 60% cases had any one type of anaemia. High percentage of microcytic hypochromic anaemia has also been reported from Raichur [12]. Moreover, 55% multi–gravid mothers showed anaemia in comparison with 45% primi–gravida who showed anaemia [13,14]. The small interval period between successive pregnancies in multigravida may be the cause of poor iron stores for next pregnancy, since there is no time to replenish the depleted iron. But in primigravida, it may due to teenage pregnancies and poor nutrition, hyperemesis and menstrual loss, which are not replenished [12]. The aspects of birth spacing and avoidance of teenage pregnancy allow the deposition of iron and normalization of iron stores.
Literacy and socio-economic status also importantly contribute to maternal anaemia. There was a strong association of illiteracy, low socio-economic status with maternal anaemia in the above conducted study [15]. 85% cases with reported anaemia were of very low socio-economic status. Most of them did not have any permanent income in their families. In developed countries, the prevalence of anaemia was only 18% among pregnant women, as was reported by WHO (1998) [1]. The socio-economic developments, higher standard of living, better utilization of health care facilities, along with increasing literacy rate, are associated with the low prevalence of anaemia in developed countries. Moreover, in the present study, it was found that anaemia increases steadily with decrease in the level of education and this was in accordance with findings of Pushpa et al., [15].
Surveys done in different parts of India have revealed that 60-80% of women who belonged to low socio-economic status were anaemic in the last trimester of pregnancy [16]. Though anaemia is prevalent in women of low socio-economic status, it is not uncommon in well to do sections of the society.
Obstetric complications were seen in 85% of anaemic mothers. The maternal complications included prolonged labour, uterine inertia and postpartum haemorrhage and one case with disseminated intravascular coagulation was also reported. Foetal complications were seen in 64% of anaemic mothers, which included low birth weights, low APGAR scores and birth asphyxia. Immune depression caused by anaemia, prolonged recovery from infection might be responsible for low birth weight babies in anaemic women. Studies have shown that there was 2 to 3-fold increase in perinatal mortality rate when maternal haemoglobin levels fell below 8.0g/d1 and that there was an 8-10 fold increase when maternal haemoglobin levels fell below 5.0 g/dl [2]. The increased perinatal mortality can be attributed to sepsis and prematurity.
Data from surveys carried out by National Family Health Survey (NFHS) [17], Indian Council of Medical Research [18], National Nutritional Monitoring Bureau [19] and District Level Household Survey [20] showed that there has not been any decline in cases of anaemia in pregnancy. Poverty, ignorance, non–availability and/or failure in utilizing available medical facilities have been shown to be associated with maternal anaemia on one hand and with maternal and perinatal morbidity and mortality on the other, though the association is not causal. The 10th five year plan emphasized the need of universal screening for anaemia in pregnant mothers and early detection and management for the same [21]. Health education given to improve the utilization of available facilities and improvement in the health care delivery system to cater to the needy, right at their doorsteps, may thus go a long way in reducing adverse obstetric outcomes associated with maternal anaemia.
Conclusion
Our present study done in the third trimester of booked antenatal mothers showed that 83% of cases were reported to have anaemia. Inspite of regular antenatal visits, most of them showed microcytic hypochromic anaemia 37%, indicating iron deficiency anaemia. It was also noted that a majority of them belonged to low education status, along with poor socio-economic status and multi-parity, during determination of birth outcome and foetal complications. Regular patient education given by imparting proper knowledge regarding iron rich foods, food fortification, implementation of anaemia prophylaxis programmes from adolescence, regular antenatal care from first trimester, play a vital role in managing maternal anaemia effectively and for effective perinatal outcomes. All practitioners handling obstetrics cases should be motivated for prescribing iron preparations and balanced diet with good compliance.