Rheumatic heart disease is still a problem in the developing countries including India with significant morbidity and mortality [1,2]. A large body of evidence indicates that patients with MS are at increased risk of developing LA thrombus and its associated thrombo-embolic complications [3–5]. Thromboembolic complications especially cerebral embolism, one of the major morbidities of rheumatic MS occur in about 10-20% of patients with MS. Obstruction of mitral valve caused by MS causes stagnation of blood flow, leading to thrombus formation in the left atrium, especially the left atrial appendage. This clot can dislodge from the left atrium and reach the systemic circulation leading to thrombo-embolic complications [5]. Not all patients with severe MS develop thrombus in the left atrium. The reason for the thrombi to develop in only some patients, but not in others is unknown.
Hence, we proposed to conduct a study to explore alternative aetiological factors for this condition, specially focusing on possible oxidative stress and inflammatory mechanisms. The aim of this study was to assess the alterations in the circulating levels of markers of oxidative stress and inflammation in patients of severe rheumatic MS with and without LA thrombus and to study their predictive power to detect the presence of LA thrombus in patients with rheumatic MS.
Material and Methods
This was a cross-sectional study of 80 patients with symptomatic severe rheumatic MS (mitral valve area on routine transthoracic echocardiography (TTE) <1.2 cm2), undergoing transesophageal echocardiography (TEE) evaluation for presence or absence of LA thrombus, before percutaneous mitral commisurotomy. Group 1 comprised of patients with rheumatic MS with LA thrombus (n=35) and Group 2 included patients with rheumatic MS without LA thrombus (n=45). Patients with clinical evidence of rheumatic activity, mitral regurgitation, prior anticoagulation therapy, history of known coagulation abnormalities, history of coronary artery disease, diabetes, hypertension, endocrine disorders, smoking, renal/liver impairment, infective endocarditis, neoplasia, connective tissue disease, deep vein thrombosis or pulmonary embolism were excluded from the study. Written informed consent was taken from all study subjects, prior to recruitment. Ethical approval was taken from the Institute’s Human Ethics Committee. The study protocol conformed to the ethical guidelines of the 1975 Declaration of Helsinki.
Detailed history was taken and clinical examination was performed in all study subjects. Echocardiographic parameters [mitral valve area, mean trans-mitral gradient, pulmonary artery pressure, Left atrial spontaneous echo contrast (LASEC)] were assessed in all study subjects. LASEC was graded from 0-4 based on Fatkin’s score [6].
Biochemical parameters were estimated in the 5 ml fasting blood sample drawn immediately, after the TEE in both the groups. During the same visit, anthropometric measurements (weight, height) were recorded. Body mass index (BMI) was calculated as per standard formula as the ratio of weight in kilograms and the square of the height in metres. Routine biochemical investigations like blood glucose, lipid profile and uric acid were estimated in all study subjects using standard methods using reagent kits from Agappe Diagnostics (Agappe Diagnostics Limited, Kerala, India) and Erba Diagnostics (ERBA Diagnostics Limited, Mannheim, Germany). All the above estimations were carried out in a well-calibrated automated clinical chemistry analyser, RX Imola (Randox Laboratories Limited, Crumlin, UK).
Assay of Study Parameters
MDA was estimated by the method of Agarwal and Chase, [7] using high performance liquid chromatography (SP-20A HPLC system, Shimadzu, Japan). Protein carbonyls were assayed according to the Levine’s method as modified by Chakraborthy [8]. Total oxidant status was assayed by the method of Erel [9]. Total antioxidant status was assayed using commercially available kit from Cayman Chemical Company, Ann Arbor, Michigan, USA. hs-CRP levels were estimated using commercially available ELISA kit from Diagnostics Biochem Canada Inc., Ontario, Canada. Total and protein-bound sialic acid levels were assayed by modified Aminoff’s method [10].
Statistical Analysis
All statistical analysis was done using SPSS (Statistical Package for Social Science). Both descriptive and inferential statistics were used to analyse the data. Baseline characteristics of the patients with MS were analysed by descriptive statistics. Categorical data were described using percentages and frequencies and were compared by using Chi–square test or Fischer’s exact test. The normality of continuous data was assessed by Kolmogrov-Smirnov test. Normally distributed data were described by mean ± standard deviation and median was used for non-Gaussian data. Normally distributed continuous data were compared by Independent Student’s t-test and Mann Whitney “U” test was used for non-Gaussian data. The association of clinical, biochemical and echocardiographic variables with the occurrence of LA thrombus was analysed using univariate analysis. The variables which are found significant in univariate analysis were considered for multivariate logistic regression analysis. Analysis was carried out at 5% level of significance and p<0.05 was considered as statistically significant.
Results
Out of 80 patients with rheumatic mitral stenosis, 35 had left atrial thrombus and 45 patients had no thrombus. Among the 35 patients with left atrial thrombus, 11 (31.4%) were males and 24 (68.6%) were females. Among the 45 patients without thrombus, 13 (24%) were males and 32 (76%) were females. The mean age of the patients in Group 1 was 40.83±6.99 years and that in Group 2 was 38.51±8.64 years. Mean waist-hip ratio of patients in Groups 1 and 2 was 0.86±0.05 and 0.86±0.04 respectively and the mean BMI was 20.41 ± 4.02 and 20.44 ± 4.26 kg/m2 respectively. These differences were not significant statistically.
In the present study, MDA (4.15±1.83 vs. 2.33±1.30 μmol/L, p<0.001), protein carbonyl (4.15±0.72 vs. 3.20±0.76 nmol/mg protein, p<0.001) and total oxidant status (12.85±2.16 vs. 7.81±1.39 μmol H2O2 Eq/L, p<0.001), were significantly elevated, whilst total antioxidant status (0.06±0.003 vs 0.10±0.006 nmol/Trolox status, p=0.001) showed a significant fall in rheumatic MS patients with LA thrombus (Group 1), as compared with those without LA thrombus (Group 2). Markers of inflammation such as hs-CRP (6.45±1.91 vs. 4.13±2.83 mg/L, p<0.001), TSA (192.54±64.57 vs. 152.30±58.59 mg/L, p=0.005) and PBSA (61.81±16.74 vs. 46.88±13.55 μg/mg of protein, p<0.001) showed a significant rise in Group 1, as compared with Group 2. These differences persisted after adjustment for confounding variables.
A comparison of the echocardiographic variables between the groups showed that mitral valve area was significantly lower in Group 1 (0.92±0.11 cm2), as compared with Group 2 (1.00±0.11 cm2) (p<0.0007). Mean mitral gradient, pulmonary artery pressure and LASEC grading was not significantly different among patients with LA thrombus, as compared with those without LA thrombus.
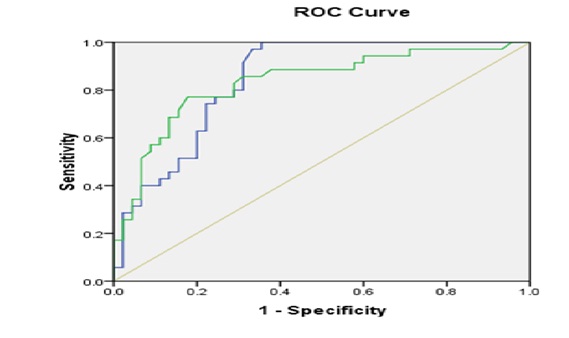
Atrial fibrillation (AF) was reported in 91.4% of patients with LA thrombus, where as it was 66.6% in without LA thrombus group, but incidence of AF was significantly higher in LA thrombus group, when compared to without LA thrombus group (p < 0.018). Receiver Operating Characteristic curve was used to evaluate the usefulness of MDA and protein carbonyls in predicting the occurrence of thrombus [Table/Fig–1]. It showed that serum MDA in predicting thrombus showed 80% sensitivity and 71% specificity at a cutoff value 2.7μmol/L with area under the curve of 0.844. Similarly, ROC to assess the diagnostic performance of protein carbonyls in predicting thrombus showed 83% sensitivity and 71% specificity at a cut off value of 3.59 nmol/mg of total protein with AUC 0.833.
Receiver operating characteristic curve of MDA and Protein Carbonyls
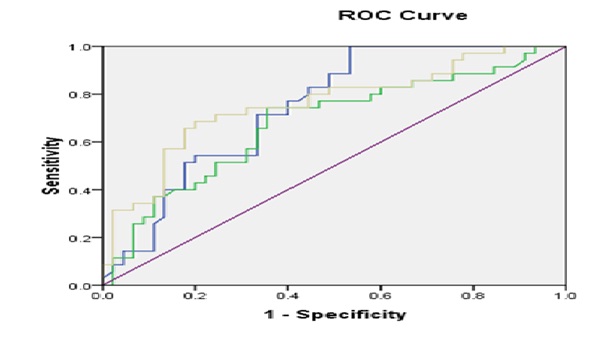
Receiver Operating Characteristic curve was used to evaluate the usefulness of hs CRP, TSA and PBSA in predicting the occurrence of thrombus [Table/Fig–2]. It showed that serum hs-CRP in predicting thrombus showed 71% sensitivity and 67% specificity at a cut off value of 5.275mg/L, with area under the curve of 0.745. Similarly, to assess the diagnostic performance of TSA in predicting thrombus showed 71.4% sensitivity and 64.4% specificity at a cut off value of 169.645 mg/dL and area under the curve was 0.679 and serum PBSA in predicting thrombus at a cut-off value of 53.66 μg/mg of total protein showed 71.4% sensitivity and 75.6% specificity with AUC 0.757.
Receiver operating characteristic curve of hs-CRP, TSA and PBSA
The biochemical parameters such as MDA, protein carbonyls, total oxidant status and total anti-oxidant status, hs-CRP, TSA and PBSA found significant in univariate analysis were considered for multivariate logistic regression analysis. MDA, protein carbonyls and protein-bound sialic acid were independent factors associated with the occurrence of thrombus in patients with rheumatic MS [Table/Fig–3].
Predictors of left atrial thrombus on multivariate analysis
| Sl. No. | Parameter | Odds Ratio | 95% C. I | p–value |
|---|
| Lower | Upper |
|---|
| 1 | Malondialdehyde | 3.079 | 1.575 | 6.022 | 0.001 |
| 2 | Protein Carbonyls | 6.359 | 2.066 | 19.569 | 0.001 |
| 3 | Total oxidant status | 2.071 | 1.970 | 2.169 | 0.147 |
| 4 | Total antioxidant status | 1.115 | 0.995 | 1.135 | 0.181 |
| 5 | hs-CRP | 1.274 | 0.901 | 1.801 | 0.171 |
| 6 | Total Sialic Acid | 1.005 | 0.994 | 1.015 | 0.393 |
| 7 | Protein Bound Sialic Acid | 1.09 | 1.022 | 1.162 | 0.009 |
Discussion
The present study investigated the circulating levels of markers of oxidative stress and inflammation in patients with rheumatic MS and compared the alterations in the above parameters in patients with and without LA thrombus.
MDA is an index of lipid peroxidation due to reactive oxygen species. Reactive Oxygen Species (ROS) can react with proteins to form protein carbonyls. This serves as a relatively early index of oxidative stress and is preferred as a oxidative marker due to its early formation and the relative stability of carbonylated proteins. Total oxidant status and total anti-oxidant status refer to the summation of pro-/oxidants and anti-oxidants present in the serum. Hence we measured the above pro-anti-oxidants in patients with rheumatic MS with and without LA thrombus.
Although the role of oxidative stress in the pathophysiology of rheumatic heart valve disease has been suggested, little is known about the underlying mechanisms and a number of questions still remain to be clarified. Chiu-Braga et al., [11] examined oxidative status of patients with rheumatic heart valve disease (HVD) using advanced oxidation protein products. In concordance with our results, they found that levels of advanced oxidation protein products were significantly elevated in rheumatic HVD patients compared to controls and that these elevated levels were not correlated with the severity of mitral disease.
The role of oxidative stress in the formation of thrombus in the LA is currently a subject for ongoing research. We found that MDA, protein carbonyls and total oxidant status were significantly elevated, whilst total anti-oxidant status lowered in patients with rheumatic MS with LA thrombus, as compared with those without LA thrombus. These differences persisted after adjustment for confounding variables. This decrease in total antioxidant status, along with increase in pro-oxidants could explain the complications caused due to elevated oxidative stress in rheumatic MS, increasing risk for thrombus formation.
CRP belongs to the pentraxin family of acute phase proteins and hs-CRP has a role in inflamed tissues promoting local pro-inflammatory effects [12]. Therefore, elevated CRP levels may influence on the natural history of the disease by inducing local activation of complement and subsequent amplification of local inflammation and cellular damage [12–13].
In the present study, hs-CRP levels were higher than the expected normal values in both the groups. The levels were significantly higher in the LA thrombus group, as compared with those without thrombus. This difference persisted after adjustment for confounding variables. Alyan et al., [14] demonstrated that high levels of high sensitivity C-reactive protein (hs-CRP) may be associated with severity of chronic rheumatic MS.
Sialic acids are acetylated derivatives of neuraminic acid. Sialic acid is a more stable inflammatory marker and therefore provides a more accurate reflection of an individual’s inflammatory status [15]. Sialic acid shows less intra-individual variability and is perhaps a more representative marker of the overall acute–phase response [15]. It may be a more appropriate acute-phase marker in rheumatic MS patients.
In the present study, TSA and PBSA levels were higher than the expected normal values in both the groups. The levels were significantly higher in the LA thrombus group, as compared with those without thrombus. This difference persisted after adjustment for confounding variables. To the best of our knowledge, there are no previous studies which have evaluated sialic acid levels in rheumatic MS.
Increased hs-CRP and sialic acid levels in LA thrombus group might increase the risk for the formation of thrombus in the left atrium in rheumatic MS patients. As seen in the present study, it has been shown that the inflammatory response still persists in patients with rheumatic MS with LA thrombus. This suggests a putative role for systemic inflammation in the pathogenesis of LA thrombus formation. A role for unrecognised sub-clinical rheumatic activity in patients with chronic rheumatic valvular disease is suggested, as neither group had patients with conventional evidence of neither rheumatic activity nor active carditis. Subclinical inflammation could play a role in the pathogenesis of LA thrombus formation in rheumatic MS patients.
We found that the circulating levels of MDA, protein carbonyls and protein-bound sialic acid were independent factors associated with occurrence of thrombus in patients with rheumatic MS. This suggests a putative role for oxidative stress and inflammatory mechanisms in the pathogenesis of LA thrombus formation. Evidences that the inflammatory response still persists in the chronic phase of the disease was shown previously by different authors [14,16]. This suggests that oxidative stress and inflammatory mechanisms could contribute to the pathophysiology of thrombosis in the LA in rheumatic MS.
As expected, in the present study, the mitral valve area was lower in LA thrombus group, than in the group without thrombus, indicating that the extent of stenosis was higher in Group 1 and hence this could be one of the contributing factors for developing thrombus in this group of rheumatic MS patients. There was no difference between the groups in the LASEC, mean mitral gradient or the pulmonary artery pressure. This is in concordance with a previous study by Karthikeyan et al., [16].
In the present study, AF between the groups (with and without LA thrombus) showed that the proportion of individuals with AF is significantly higher in thrombus group (91.4%), when compared to non-thrombus (66.6%) group. Increased AF in group 1, along with increase in oxidative stress, could cause increased thrombogenesis in the LA in this group of rheumatic MS patients. In a study by Dudley et al., [17] the authors report that AF increases reactive oxygen species (ROS) production in the left atrium. Increased NAD(P)H oxidase and xanthine oxidase activities contribute to the observed increase in ROS production in the LA. This increase in superoxide and its reactive metabolites may contribute to atrial oxidative injury and hence, the pathological consequences of AF such as thrombosis, inflammation, and tissue remodelling [17–18].
The limitations of the present research work included the small sample size involving only 80 study subjects and the high prevalence of AF in the LA thrombus group as AF itself may be a confounding variable for increased oxidative stress. Hence further studies are required involving a larger patient sample to validate our results and establish the role of oxidative stress in the pathogenesis of thrombus formation in the LA in rheumatic MS.
In conclusion, our results suggest that there is oxidative stress and inflammation in patients with rheumatic MS, but more significant in those with LA thrombus, than in those without LA thrombus. Our findings suggest that oxidative stress and inflammatory mechanisms contribute to the pathophysiology of thrombosis in the left atrium in patients with rheumatic MS. However, the exact mechanisms involved remain to be unravelled in future studies. Randomized clinical trials, using anti-oxidant supplementation and anti-inflammatory drugs, would aid in devising establish more appropriate therapy in patients with rheumatic MS and change the natural course of the disease and prevent the formation of thrombus in the LA in rheumatic MS.
Author Contributions
M Rajappa and S Satheesh conceived the idea for analysis. S Satheesh, P Vinay Kumar and M Vengatesan were involved with recruitment of study subjects. P Vinay Kumar, M Vengatesan and M Rajappa were involved with sample collection and laboratory assays. KT Harichandrakumar conducted statistical analysis. M Rajappa and S Satheesh drafted the original manuscript. All the authors were involved with revising the manuscript critically for important intellectual content and gave approval for this final version to be published.
Funding: The present study was funded by the Intramural Research Grant of the Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER), Puducherry, India.
Conflict of interest- The authors report no conflict of interest.