Treatment of Internal Resorption with Mineral Trioxide Aggregates: A Case Report
Pankaj Yadav1, Yogesh Rao2, Anurag Jain3, Nikhil Relhan4, Sandeep Gupta5
1 Senior Resident, Department of Conservative Dentistry and Endodontics, Maulana Azad Institute of Dental Sciences, Delhi, India.
2 Senior Lecturer, Department of Prosthodontics, Maharana Pratap College of Dentistry and Research Centre, Gwalior, India.
3 Senior Lecturer, Department of Conservative dentistry and endodontics, Maharana Pratap College of Dentistry and Research Centre, Gwalior, India.
4 Senior Lecturer, Department of Department of Conservative Dentistry and Endodontics, Pacific Dental College and Hospital, Udaipur, India.
5 Senior Lecturer, Department of conservative dentistry and endodontics, Maharana Pratap College of Dentistry and Research Centre, Gwalior, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Pankaj Yadav, Senior Resident, Department of Conservative Dentistry and Endodontics, Maulana Azad Institute of Dental Sciences, New Delhi, India.
Phone: 09313545604,
E-mail: Dr_pankaj_111@yahoo.co.in
Tooth resorption is a common sequel which follows injuries or irritation to the periodontal ligament and/or tooth pulp. The course of tooth resorption involves an elaborate interaction among inflammatory cells, resorbing cells, and hard tissue structures. The key cells which are involved in resorption are multi–nucleated giant cells. Internal root resorptions are usually non–symptomatic and they are discovered occasionally through periapical radiographs, which reveal very defined and regular outlines. Many techniques and materials have been used to fill internal resorptive defects. Among them, Mineral Trioxide Aggregates (MTAs) have satisfactory properties, which include: biocompatibility, a favourable sealing ability, mechanical strength and a capacity to promote a periradicular tissue healing. Thus, a Mineral Trioxide Aggregate (MTA) repair of a maxillary left central incisor tooth with an inflammatory resorptive defect, in the middle third of the root canal, has been reported here.
Internal resorption, Endodontic treatment, MTA
Introduction
Internal root resorption which originates from pulp inflammation is always pathological. Internal resorption is established after necrosis of odontoblasts and it is associated with chronic partial pulp inflammation and partial pulp necrosis [1]. Only the resorption of deciduous teeth is considered to be physiological, whereas the root resorption of permanent teeth is considered to be pathological [2].
Its etiology is not quite clarified, however, it can be associated with many factors such as partial removal of the pulp, caries, trauma, pulp capping with calcium hydroxide or pulpotomy, extreme heat and a cracked tooth. These factors stimulate the pulp tissue, thus initiating inflammatory processes and then some undifferentiated cells of the pulp convert themselves to osteoclasts or macrophages, which results in dentinal resorption [3].
In a majority of the cases, the internal resorption usually is asymptomatic and it is detectable by routine radiographs. Radiographically, it is described as a radiolucent area which is characterised by an oval–shaped enlargement of the root canal, which shows many times the appearance of an ampoule and which does not move with variations of radiographic angle [1]. Midroot internal resorption has sharp margins; most of the lesions are symmetrical, and uniform in density. With internal resorption, the canal cannot be traced and it will appear to balloon out into the lesion [4]. In more evolved cases, the fragility of the dental structure can cause areas of fracture or perforation [3].
Being originally developed as a surgical root end filling material, MTA has been successfully used in several clinical applications such as pulp capping [5] pulpotomy [6] perforation repair [7] treatment of traumatized teeth with immature apices [8] and for treatment of root resorptions [9].
Case Report
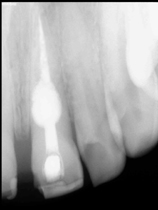
A 28–year–old male patient presented with a history of a broken filling in maxillary left and right central incisors. The periapical radiograph revealed that [Table/Fig-1] the left central incisor tooth had undergone internal resorption. The patient was in good health, with no significant past or present illnesses, and he reported no history of any dental trauma. His medical history was uneventful. Clinically, there was no colour change in left central incisor [Table/Fig-2] and the tooth was asymptomatic. The tooth did not respond to vitality tests. The tooth was isolated with a rubber dam and access to it was achieved on the lingual aspect of the crown. Necrotic pulp tissue was removed from the canal and working length was established. The coronal aspect of the canal was opened by using a Gates glidden. Then, canal was instrumented apically to K file number 60 and it was back stepped to a K file number 80 in 0.5 mm increments. The absence of a perforation in the defect was confirmed by paper points (absence of bleeding) and the use of an apex locator (Rayapex 5). Sodium hypochlorite was used copiously throughout the procedure and calcium hydroxide paste was placed in the canal for a week, to alkalinise the environment. After 7 days, calcium hydroxide dressing was removed. The canal was irrigated with EDTA, followed by sodium hypochlorite irrigation and then, it was finally irrigated with chlorhexidine and dried. After the root canal was prepared, gray MTA was manipulated and applied to the resorption cavity and to rest of the canal as a root canal filling material [Table/Fig-3]. Then, the coronal cavity was restored by using composite [Table/Fig-4].
Periapical film reveals that the tooth has undergone internal resorption

Clinical appearance of maxillary right and left central incisor

Immediate post-treatment radiograph
Post–operative clinical view

Discussion
Inflammatory root resorption is a multi–disciplinary problem which requires a variety of specialists, to understand the aetiology, pathogenesis, diagnosis and treatment of this disease [2].
The process of tooth resorption involves an elaborate interaction among inflammatory cells, resorbing cells, and hard tissue structures. However, the process of tooth resorption is believed to be very similar to that of bone resorption. Injuries to and irritation of bone, dentin, or cementum lead to chemical changes within these tissues; the result is the formation of multi–nucleated giant cells, which are referred to as clasts. The clastic cell is the key cell type which is responsible for all hard tissue resorptive processes, which are accompanied by cells such as macrophages and monocytes in resorptive activities. Collectively, these cells orchestrate a complex interplay of molecular biologic events which involve cytokines, enzymes, and hormones, which influence the progression of resorption [10].
It is a very common thought that internal and external inflammatory root resorptions are often confused and misdiagnosed. A correct diagnosis is essential, since internal and external resorptions are totally different pathological processes, with different aetiological factors and treatment protocols. Diagnosis is based mainly on radiographic features, which are supplemented by clinical findings. Accepted radiographic features that differentiate internal from external resorptions are: radiographs which are taken at different angles will result in movement of the lucency on the root in external resorption, while the lucency will stay close to the canal in internal resorption. An external resorption will have an irregular lucency and the canal can often be seen through the lucency, while an internal resorption has clearly defined borders with no radiographically visible canal in the defect [2].
The lesion in this case was diagnosed as an internal resorption, based on radiographic examination (clearly defined margins, uniform density and root canal wall appear to balloon out). According to Culbreath et al., the treatment for internal resorption can include several materials such as gutta percha, zinc oxide eugenol and amalgam alloy. However, these materials do not provide strength to the tooth structure and they may be responsible for considerable discolouration.
The outcome of treatment of teeth with internal root resorption depends primarily on the size of the lesions. Large lesions cause a reduction in the resistance of the tooth to shear forces that may lead to tooth fracture. Therefore, it is imperative to initiate an endodontic treatment as soon as possible, to arrest the progression of the resorptive process and to prevent root or cervical crown fractures [11].
In this case, MTA was selected because of its known abilities for repairing sealing and mechanically strengthening the weak lateral walls. MTA has many favourable properties, which include good sealing properties, biocompatibility, bactericidal effects, radiopacity and ability to set in the presence of blood [12].
Conclusion
It can be concluded that a mineral trioxide aggregate may be a suitable material for use in the treatment of an internal resorption in the coronal third of the root canal.
[1]. Jacobovitz M, de Lima RKP, Treatment of inflammatory internal root resorption with mineral trioxide aggregate: a case reportInternational Endodontic Journal 2008 41:905-12. [Google Scholar]
[2]. Lyroudia Kleoniki M, Dourou Vasiliki, Panteiidou Ourania CH, Labrianidis Theodoros, Pitas Loannis K, Internal root resorption studied by radiography, stereomicroscope, scanning electron microscope and computerized 3D reconstructive methodDental Traumatology 2002 18:148-52. [Google Scholar]
[3]. Araujo Lins CG, Study of prevalence of internal resorption in periapical radiography of anterior permanents toothInt. J. Morphol 2009 27:227-30. [Google Scholar]
[4]. Gartner AH, Mack T, Somerlott RG, Walsh LC, Differential diagnosis of internal and external root resorptionJ Endod 1976 2:329-34. [Google Scholar]
[5]. Pitt Ford TR, Torabinejad M, Abedi Hr, Using mineral trioxide aggregate as a pulp capping materialJ Am Dent Assoc 1996 127:1491-94. [Google Scholar]
[6]. Salako N, Josph B, Ritwik P, Salonen J, John P, Comparison of bioactive glass, mineral trioxide aggregate, ferric sulphate and formocresol as pulpotomy agents in rat molarDental traumatology 2003 19:314-20. [Google Scholar]
[7]. Main C, Mirzayan N, Shabang S, Torabinejad M, Repair of root perforations using mineral trioxide aggregate: a long term studyJournal of Endodontics 2004 30:80-83. [Google Scholar]
[8]. Bakland LK, Management of traumatically injured teeth using MTAJournal of California Dental Association 2000 28:855-58. [Google Scholar]
[9]. Simon S, Rilliard F, Berdal A, Machtou P, The use of mineral trioxide aggregate in one visit apexification treatment: a prospective studyInternational Endodontic Journal 2007 40:186-97. [Google Scholar]
[10]. Ne Rita F, Witherspoon David E, Gutmann James L, Tooth resorptionQuintessence Int 1999 30:9-25. [Google Scholar]
[11]. Keinan D, Heling I, Stabholtz A, Moshonov J, Rapidly progressive internal root resorption: a case reportDental Traumatology 2008 24:546-49. [Google Scholar]
[12]. Meire M, Moor RD, Mineral trioxide aggregate repair of a perforating internal resorption in a mandibular molarJ Endod 2008 34:220-23. [Google Scholar]