Management of Severe Gag Reflex by An Unique Approach: Palateless Dentures
Anoop Jain1, Vijayalaxmi V2, R.M. Bharathi3, Veena Patil4, Jyoti Alur5
1 Post Graduate Student, Department of Prosthodontics, HKE’S S N institute of dental sciences & Research, Karnataka-585105, India.
2 Assistant Professor, Department of Prosthodontics, G Pulla Reddy dental college, Andhra Pradesh-518002, India.
3 Professor, Department of Prosthodontics, G Pulla Reddy dental college, Andhra Pradesh-518002, India.
4 HOD & Professor, Department of Periodontics, HKE’S S N Institute of Dental Sciences & Research, Karnataka-585105, India.
5 Senior Lecturer, Department of Oral Pathology, HKE’S S N institute of dental sciences & Research, Karnataka-585105, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Anoop Jain, Post Graduate Student, Department of Prosthodontics, HKE’S S N institute of dental sciences & Research, Karnataka-585105, India.
Phone: +91-8860700181,
E-mail: dranoopjn@gmail.com
Gagging is most common protective reflex that prevents the foreign bodies from entering trachea. But some patients have abnormally active gag reflex. The purpose of this paper was to describe method of managing gagging patients , based on modified treatment approaches, starting from impression making to design of the prosthesis i.e. palateless denture, to help the patient tolerate prosthesis in his/her mouth.
Gag reflex, Gagging, Overdenture, Palateless, Retching
Case Report
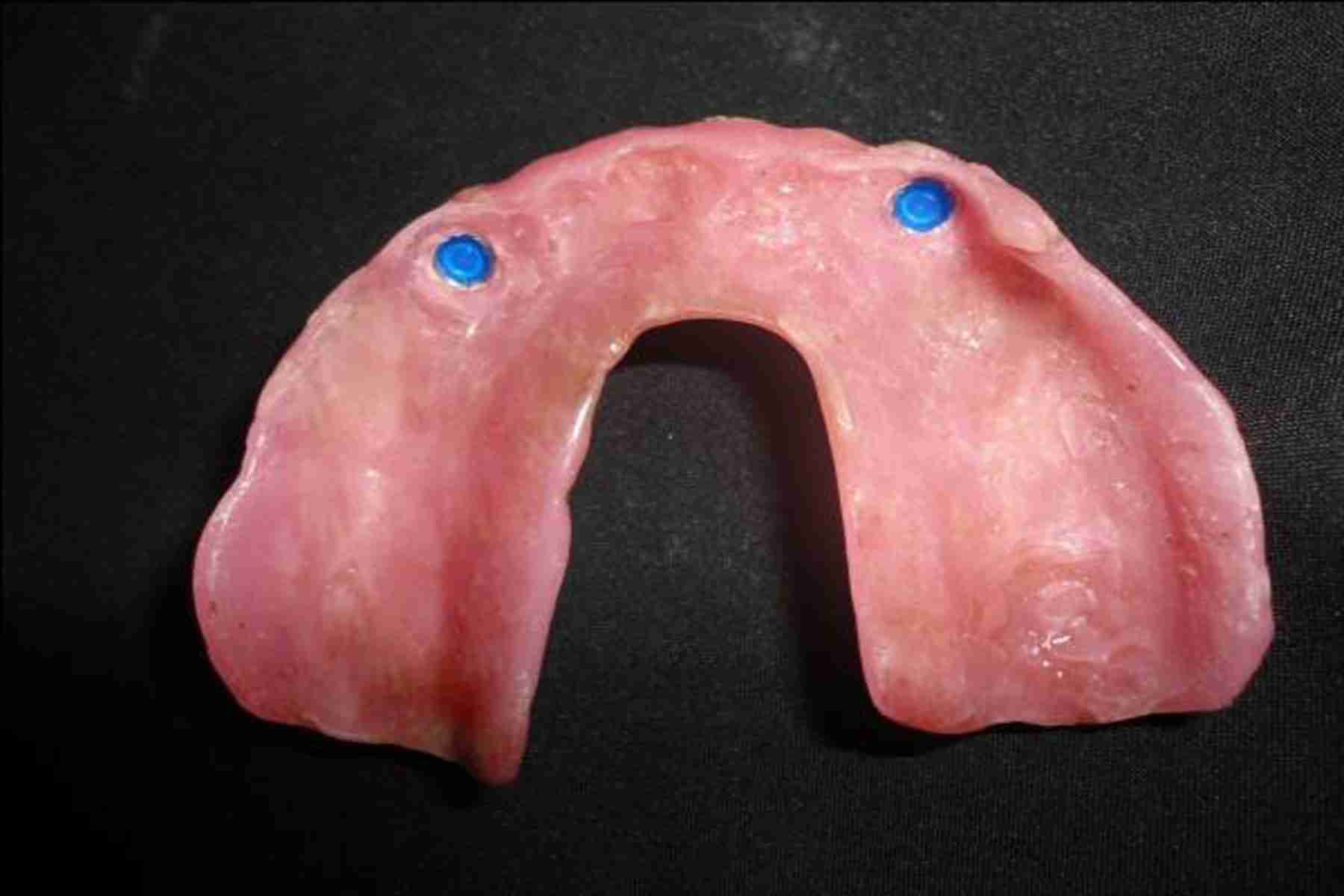
A 55–year–old male reported to Department of Prosthodontics, HKES’s S N Institute of Dental Sciences and Research, Karnataka, India, for replacement of his missing teeth. Patient had received a maxillary acrylic resin removable partial denture six months back. He had major complaint of difficulty in wearing the prosthesis, due to severe gag reflex. Intraoral examination of patient revealed complete edentulous mandibular arch and partially edentulous maxillary arch with13, 15, 23, 24, 25 teeth. Patient had lost his teeth because of caries and periodontal problems. Clinical intraoral examination revealed that maxillary canines and premolars were periodontally sound, with no mobility and no periapical pathology. Radiographic examination revealed that bone support around the maxillary canines and premolars i.e. 13, 15, 23, 24, 25 was good. Patient did not want extraction of remaining maxillary teeth, due to medically compromised conditions. Patient was suffering from diabetes mellitus and had undergone cardiac surgery. After examination, it was observed that patient was more sensitive in posterior region of hard palate. So, to prevent the contact of prosthesis with severe sensitive region of hard palate, it was decided to manage the patient by using prosthodontic technique that included fabrication of maxillary palateless denture. However, systemic desensitization and errorless learning techniques could be used to manage the gag reflex in these patients, but they were not used because they were very slow techniques. Pharmacological techniques were not considered, because patient was suffering from systemic diseases and he was not ready to undergo them. As palateless dentures have compromised retention because of absence of posterior palatal seal area, it was decided to fabricate a maxillary palateless, locator attachment supported overdenture. After intentional root canal treatment of maxillary teeth [Table/Fig -1], these teeth were prepared, so that they could be used as overdenture abutments [Table/Fig-2]. Then, post spaces were prepared in both the canines for placement of female part of locator attachments. They were prepared with pilot drill and counter sink bur provided along with zest anchor locator kit (Zest Anchors, Escondido, CA). After checking parallelism of female part of locator attachments with the parallel post, they were cemented in right and left canine abutments with self cure resin cement (RelyX™ Unicem Self-Adhesive Universal Resin Cement, 3M ESPE, Germany) [Table/Fig-3]. An impression was made after cementation of locator attachments, and a palateless custom acrylic resin tray was fabricated on the cast. After adjusting the custom tray, border molding was done with medium body polyvinyl siloxane (Reprosil, Dentsply, Germany) and final impression was made with light body (Aquasil LV, Dentsply, Germany). Master cast was obtained by pouring the final impression into type IV gypsum product – die stone (Ultrarock, Kalabhai Karson Pvt. Ltd., Mumbai, India). Lingual palatal border was established by placing a bead line prepared on the master cast with a No. 4 round bur. The palatal borders were located at the junction of horizontal and vertical slopes of the palate and they had to be symmetric as possible. Locator attachments and abutments were covered with waxon master cast, and trial denture base was fabricated with chemically cured acrylic resins (Rapid Repair acrylic resin, DPI, Mumbai, India). The placement of wax over locator attachments and abutments prevented the fracture of abutments or attachments on master cast during removal of temporary acrylic denture base. Occlusion rims was fabricated over trial denture base. Horizontal and vertical maxillomandibular records were obtained with record bases and occlusion rims, transferred to a semi-adjustable articulator using a face bow. Artificial teeth were selected and arranged on the record base for a trial denture arrangement and evaluated intraorally for phonetics, aesthetics, occlusal vertical dimension and centric relation. After wax up, the denture was processed in heat cure acrylic resin (Lucitone 199 denture base material, Dentsply, Germany). After finishing and polishing, denture was inserted and adjustments were done. The locator male attachment were incorporated in the denture by direct method [Table/Fig-4] and finally, denture was reinserted [Table/Fig-5]. The patient was scheduled for follow-up visits every three months and he reported no complaints during eighteen months of follow-up.
Root canal treated maxillary canines and premolars

Prepared maxillary teeth abutments

Locator female attachment cemented into maxillary right and left canines

Tissue surface of maxillary palateless denture with male locator attachments
Intra–oral view of palateless maxillary denture

Discussion
Most patients whose gagging is of a psychologic nature should be treated before denture procedures are completed, so that they will be comfortable with well-constructed prostheses. However, severe gag reflex in some of the patients makes it difficult to perform each and every step of denture fabrication properly. There are various treatment modalities for gag reflex management i.e. behavioural, pharmacological and prosthodontic techniques [1]. According to Altamura et al, behavioural modification is the most successful long term method of managing the gagging patient [2]. Behaviour techniques include relaxation technique, distraction, suggestion/hypnosis, systemic desensitization, errorless learning and cognitive behavioral therapy. However, systemic desensitization and errorless learning techniques could be used to manage the gag reflex in these patients, but they were not used, because these are very slow techniques. Schole advised various pharmacological techniques i.e. local anaesthesia, conscious sedation and general anaesthesia, for managing the gagging problem [2]. Pharmacological techniques were not considered because patient was suffering from systemic diseases and he was not ready to undergo them. Prosthodontic techniques include impression technique, modification of custom tray and palateless dentures. Farmer et al, recommended as a possible solution for gagging patients, a history of unsuccessful denture wearing (as a last resort) and for patients with large inoperable maxillary toruses. The patient was managed by using palateless denture technique, because he had more trigger zones in area of soft palate adjoining hard palate [3]. Wright, in a classical study, reported that 43.4% of the patients gagged only after having dentures, and that 83% associated the condition with stimulation and touching of the palate or back of the mouth. In addition, 24.5% felt that a reduction in palatal length greatly improved their ability in wearing dentures, due to decrease in touching and stimulation of the palate by the denture [4]. Border molding and making of secondary impression by conventional approach is difficult in these gaggers. In such patients, a modified custom tray that does not completely cover the palate, can be constructed and used as an impression tray. Conventional palateless denture has less retention and stability, which further gets compromised by extensive ridge resorption, lack of vestibular depth and a shallow palatal vault. Saving few remaining periodontally sound natural teeth and fabricating palateless overdenture produce better retention and stability than removable complete dentures. Fabricating a locator attachment supported denture, further increase the stability and retention by the frictional contact between the locator attachments and denture base. Locator attachment supported overdenture is a good alternative treatment modality for prosthodontic management of patients with severe gag reflex, because of its improved retention, stability, better chewing efficiency. It also decreases alveolar bone resorption, because of the maintenance of teeth as overdenture abutments. It is very much comfortable to patients, because of the less palatal coverage, better heat, cold and taste perception, which are not possible in case of conventional complete denture because, acrylic denture base is a poor conductor of heat [5].
Conclusion
Modification of treatment approaches can enhance patient acceptance and also, successful treatment outcome in gag reflex patients. Palateless locator supported overdenture is definitely a benefit for patients having sever gag reflex with a history of unsuccessful denture wearing. It has better retention, stability and chewing efficiency than conventional palateless dentures.
[1]. Bassi GS, Humphiris GM, Longman LP, The etiology and management of gagging: A review of the literatureJ Prosthet Dent 2004 91:459-67. [Google Scholar]
[2]. Sangur R, Rao L, Varma M, Bashir U, Gagging and its management in relation to prosthodontics. SRM UniversityJ of Dental Sciences 2011 2:124-28. [Google Scholar]
[3]. Farmer JB, Connelly ME, Palateless dentures: Help for the gagging patientJ Prosthet Dent 1984 52:691-93. [Google Scholar]
[4]. Wright SM, Medical history, social habits, and individual experiences of patients who gag with denturesJ Prosthet Dent 1981 45:474 [Google Scholar]
[5]. Singh K, Gupta N, Palateless custom bar supported overdenture: A treatment modality to treat patient with severe gag reflexIndian J Dent Res 2012 23:145-48. [Google Scholar]