Whenever the treatment revolves around structural balance and aesthetic harmony, the crux remains to be the periodontal health of the existing dentition. In such scenarios where restorations and aesthetics are of concern, biologic width (BW) is the initial and final frontier. Considering attrition of teeth, the resistance which is offered by them is definitely at a lower level as compared to teeth with adequate height. Clinical crowns of worn out teeth are seriously handicapped when it comes to bearing the occlusal loads, which can be brought back to normalcy by crown lengthening . Crown lengthening includes the surgical removal of soft and hard periodontal architecture to gain (vertical dimension) a supracrestal tooth length, thus allowing a longer clinical crown reestablishment of BW. This paper has described the full mouth rehabilitation of severe fluorozed and attrited teeth in a 35–year male with the use of an interdisciplinary approach (6 Handed Dentistry).
Crown lengthening, Biologic width, Vertical dimension
Introduction
Attrition is the mechanical loss of tooth structure (from the opposing tooth) in due course of time. It primarily affects the enamel, which then progresses to the layers below. The common reason for attrition is bruxism (the parafunctional habit- clicking and clenching the teeth together apprehensively). Apart from this, the other circumstances in which the clinical crown becomes short are Amelogenesis imperfecta [1], and Dentinogenesis imperfecta [2] and in fluorozed teeth, it is hypomineralised enamel [3].
An obviously evident common spot at which the ware starts is the incisal or occlusal surface, development of a facet being part of deterioration. Incisal/occlusal wares are common when the opposing teeth move against one another in vertical direction, leading to a decrease in vertical dimension (VD).
The concept of crown lengthening (CL) was first introduced by D.W. Cohen [4]. The ultimate goal of CL is to provide the tooth structure above the alveolar crest, which is adequate for a stable dentogingival complex and for placement of a restorative margin, thus assuming the best marginal seal for retention of both a provisional and an aesthetically pleasing final restoration.
Restoring dentition to normal functional efficiency can only be achieved by restoring VD, where biologic width (BW) is of top priority. BW management is the engineering of the periodontal soft and hard structures, which results in a sound foundation. BW is defined as the physiologic dimension of the junctional epithelium and connective tissue attachment. BW concept is the result of pioneering studies which were done by Gargiulo AW [5]. They found that in the average human, the connective tissue attachment occupies 1.07 mm of space above the crest of the alveolar bone and that the junctional epithelium which is below the base of the gingival sulcus, occupies another 0.97 mm of space. The combination of these two measurements constitutes the BW (2.04 mm). This explains the violation of BW, which is a common scenario in day to day practice, which occurs due to misinterpretation of the width. These findings have been established by Vacek [6] . In this study, mean measurements were 1.34 ± 0.84mm for sulcus depth; 1.14 ± 0.49 mm for epithelial attachment; and 0.77 ± 0.32 mm for connective tissue attachment [6].
Kois mentioned that a length of 3 mm was crucial for gratifying the requirements for a constant BW. Defiance of the BW may cause bone resorption and inflammation [7].
Case Report
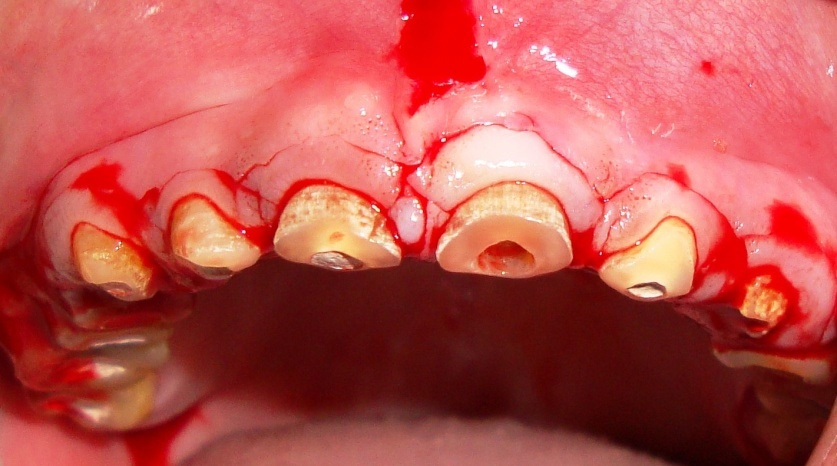
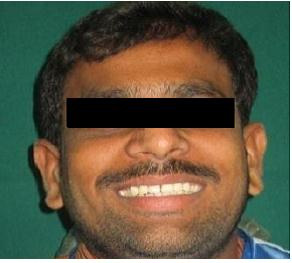
A 35–year–old male patient was referred to the Department of Periodontics with the chief complaint of a generalised decrease in size of teeth and discolouration. On examination, it was seen that there was severe attrition and a decrease in VD, which had resulted in a decrease in the height of the lower third of the face. Severe attrition also had led to compromised aesthetics. The patient was in good general health and he was not on any medication; he was neither a smoker nor a tobacco chewer. He gave a history of chipping off of the tooth structure during chewing, which could be attributed to severe fluorosis of the teeth, as patient belonged to Nalgonda district in Andhra Pradesh, India, which is endemic for fluorosis, where the concentration of fluoride in the drinking water ranges from 1.5-5 parts per million [8–10]. Patient’s parents and brother also had similar dental complaints. A thorough examination that included a clinical examination and a radiographic examination was done for an effective rehabilitation of severely compromised oral dentition. Maxillary and mandibular impressions were made by using irreversible hydrocolloid impression material and a pair of diagnostic casts was made. Insufficient clinical crown lengths were observed throughout the mouth. The overall prognosis of the patient was fair. Patient was informed about the treatment plan and his consent was taken for the same [Table/Fig-1,2 and 3].
Pre-operative facial view with severe fluorosis and attrited teeth

Pre-operative left lateral view with severe fluorosis and attrited teeth

Photograph showing the Incision
Treatment Plan
Since the treatment involved an interdisciplinary approach, a meticulous planning was needed. The treatment was carried out in different phases. In the initial Phase I therapy, scaling and root planing was performed and in the later phase, root canal treatment (RCT) for all the teeth was performed. In the surgical phase, baseline treatment of CL was performed quadrant wise. Final phase was the restorative phase in which the Porcelain which was fused to metal (PFM) crowns was given throughout the teeth where RCT and CL was performed.
Procedure
Maxillary and mandibular impressions were made with alginate and the diagnostic casts were prepared after completion of the endodontic treatment. Bite guards/templates were prepared by Department of Prosthodontics. After the phase I therapy, patient was recalled after a week, to check for the oral hygiene status. A quadrant wise approach was preferred for CL and before beginning the procedure, measurements for BW, alveolar crest height, sulcus depth, and foreseen gingival zenith were recorded.The BW was measured for each tooth by probing with UNC 15 probe to the bone level (bone sounding) and subtracting the sulcus depth from the resulting measurement. By maintaining aseptic conditions, local anaesthesia was administered in the form of nerve block and infiltration. The template was sited and by taking the apical edge of template as the reference point, the bleeding spots were marked with a probe.
The first incision, being the reverse bevel incision, was given on the labial/buccal and lingual/palatal areas, at the level of the gingival border of the template. Scalloping of the full thickness flap was accomplished while expecting the absolute underlying osseous contour [Table/Fig-4 and 5]. Creation of exact BW for the periodontal milieu requires a precise osseous contouring, which was performed by using Ochsenbein Nos. 1 and 2, Hu-Friedy, Chicago, IL and carbide/diamond burs and properly irrigating latter, for preventing any bone necrosis. The most important step was contouring of the interdental bone for allowing an apt closure of the wound, or else the main purpose would remain unsolved. The osseous contouring was performed with following steps like vertical grooving and osteotomies of the interdental and marginal bone. The above mentioned steps were followed in all four quadrants, with approximation of flap at crest of the alveolar bone, by using vertical mattress (interrupted) suture technique, since the amount of keratinized gingiva was 4 to 5 mm, followed by placement of a periodontal pack.
Intra–operative view after osteotomy in the Maxillary anterior teeth
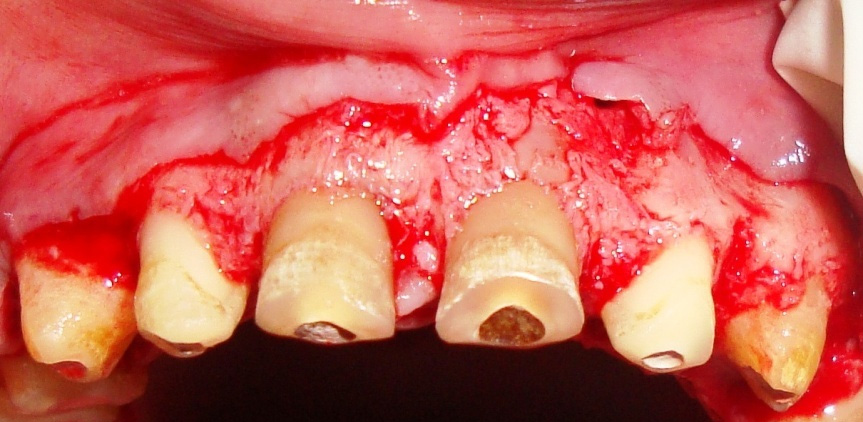
Intra–oral view after crown preparation of all the teeth

Since strict aseptic conditions were maintained, only non-steroidal anti-inflammatory drug (Tab IMOL BID for 2 days) were prescribed, with a cold pack application for the quadrant which was operated on (10 seconds on and off for 5 minutes), only on the day of surgery. Patient was advised not to rinse nor spit for the next 24 hours to avoid excessive exertion. He is advised not to brush nor floss the operated site for one week. The patient was recalled after one week for removal of the suture and the pack and healing was evaluated [Table/Fig-6].
Photograph showing healing after performing CL in all the Quadrants

Once the CL was performed in all the quadrants, the patient was referred after 2 weeks to Department of Prosthodontics for subsequent treatment, after ensuring proper healing. As the VD was reduced, a full mouth rehabilitation with increasing VD was planned. CL procedures were done to obtain a sufficient clinical crown length and a ferrule effect.Margins of the PFM crowns were planned as subgingival rather than supragingival, as latter was thought to sequence more plaque accumulation than supraor sub gingival margins. The patient’s casts were mounted on a semi-adjustable articulator (Hanau Articulator;USA) by using a face-bow record and an interocclusal record was made with the aid of a polyvinylsiloxane occlusal registration material. After the diagnostic wax-up, tooth preparation was done [Table/Fig-7 and 8] and it was followed by a gingival retraction with the use of retraction cords and impressions were made by using polyvinylsiloxane impression material. Later, provisional restorations were given, followed by metal try [Table/Fig-9]. Final finished crowns after bisque trial and final glazing were cemented using appropriate luting agent [Table/Fig-10,11,12 and 13]. The case was followed for the past one year and the prosthesis seemed to be in good condition.
Maxillary Cast showing Die sectioning with individual PFM Crowns

Mandibular cast showing Die sectioning with individual PFM Crowns


Facial view after giving the PFM Crowns



Patient appearance after placing the PFM crowns
Discussion
Crown Lengthing is done for aesthetic improvement and for teeth with subgingival caries or fractures, this also establishes a BW, thus enabling a proper prosthetic management. The greatest focus in the above situation is attaining an ideal BW of a generalized 3mm, along with an increased VD, which were successfully achieved. A precise diagnostic and an interdisciplinary advent is obligatory for obtaining better-quality, conservative and predictable outcomes in aesthetically conceded areas. Periodontal health is of supreme significance for all teeth, restored and comprehensive together. Accordingly, CL, in addition to restorative treatment, can fashion anticipated results, thus retaining good aesthetics and periodontal health. All targets were achieved, which were in accordance with those of the studies which were done by Gargiulo, Orban’s and Sato [11] with a perfect space for restoration and periodontal milieu.
Conclusion
Squaring the root cause (attrition) does not solve the purpose, for establishing VD with procedures like CL; the Smirk periodontal milieu has the last laugh. It is all the more imperative to follow the guidelines for maintenance of the periodontium.
[1]. Seow W. K., “Clinical diagnosis and management strategies of amelogenesis imperfect variants,”Pediatr Dent 1993 15:384-93. [Google Scholar]
[2]. O’Connell AC, Marini JC, Evaluation of oral problems in an osteogenesis imperfecta populationOral Surg Oral Med Oral Pathol Oral Radiol Endod 1999 87:189-96. [Google Scholar]
[3]. Sherwood Anand I, Fluorosis varied treatment optionsJ Conserv Dent 2010 13:47-53. [Google Scholar]
[4]. Cohen ES, Atlas of cosmetic and reconstructive periodontal surgery 1994 2492nd edPhiladelphiaLea and Febiger:370-80. [Google Scholar]
[5]. Gargiulo AW, Wentz FM, Orban B, Dimension and relations of the dentogingival junction in humansJ Periodontol 1961 32:262 [Google Scholar]
[6]. Vacek JS, Gher ME, Assad DA, Richardson AC, Giambarresi LI, The dimensions of the human dentogingival junctionInt J Periodontics Restorative Dent 1994 14:155-65. [Google Scholar]
[7]. Kois J, New paradigms for anterior tooth preparation: Rationale and techniqueOral Health 1998 88:19-22.:25-27.:29-30. [Google Scholar]
[8]. Akpata ES, Fakiha Z, Khan N, Dental fluorosis in 12-15 year old rural children exposed to fluorides from well drinking water in the Hail region of Saudi ArabiaCommunity Dent Oral Epidemiol 1997 25:324-27. [Google Scholar]
[9]. Rao Venugopal V, Chakravarthy R, Ratnakar KS, Familial aggregation and segregation in endemic fluorosis in the villages located in the fluoride belts of Nalgonda distrct, Andhra PradeshIUP J Genet Evol 2010 11:50-1153. [Google Scholar]
[10]. Rao Ramamohana NV, Rao N, Rao Surya Prakash K, Schuiling RD, Fluorine distribution in waters of Nalgonda district, Andhra Pradesh, IndiaEnvironmental Geology 1993 21:84-89. [Google Scholar]
[11]. Gargiulo A, Krajewski J, Gargiulo M, Defining biologic width in crown lengtheningCDS Rev 1995 88:20-23. [Google Scholar]