Hemifacial Microsomia (HFM) is an asymmetric craniofacial malformation which results in hypoplasia of the components of the first and second branchial arches. There can be various anomalies, which include conductive hearing loss which is caused by external and middle ear deformities. HFM is the second most common congenital facial anomaly which is seen after cleft lip/palate. For the pre-surgical evaluation of this anomaly, diagnostic imaging and classification of the facial structures, based on OMENS classification, is of prime importance. The management of this developmental malformation is multidisciplinary. We are presenting a series of three cases with diverse clinical and radiographic features which ranged from mild facial asymmetry and ear malformation to facial paralysis.
Developmental malformation, Diagnostic imaging, Hemifacial microsomia, OMENS classification
Case Series
Case 1
A 17-year-old female patient reported to the dental hospital, complaining of a facial asymmetry since birth. Clinical examination revealed an underdeveloped left side of the face, with hallowing facial structures in the preauricular region [Table/Fig-1]. On same side, ear lobe was malformed [Table/Fig-2]. Maxillary and zygomatic bones of the ipsilateral side were smaller in size as compared to those on right side. The left eye was at a lower level than the right one. Lateral protrusive movements of the mandible, towards the left side, were restricted. On palpation, posterior aspect of left side of pre auricular region felt depressed. The condylar movements were not felt on the left side and the external auditory meatus could not be traced on the same side. Left side mandibular growth appeared to be arrested and during an intra-oral examination, mouth opening appeared to be restricted (27 mm inter incisal distance) and to deviate towards left side. Posterior cross bite and crowding in maxillary teeth were also present [Table/Fig-3].
Gross facial asymmetry and arrested growth of the left side of the face

Malformed left ear with absence of external auditory meatus

Posterior cross bite, crowded maxillary teeth with malocclusion

A postero-anterior (PA) skull projection revealed absence of upper part of ramus, condyle and coronoid process on left side [Table/Fig-4]. All third molars were unerupted and 43 was impacted in symphysis region. The same findings were confirmed by Lateral Oblique [Table/Fig-5] and panoramic radiographs.
Postero-anterior skull projection showing absence of upper part of ramus, condyle and coronoid on left side, both orbits not at the same level, mandibular midline shift towards the left side
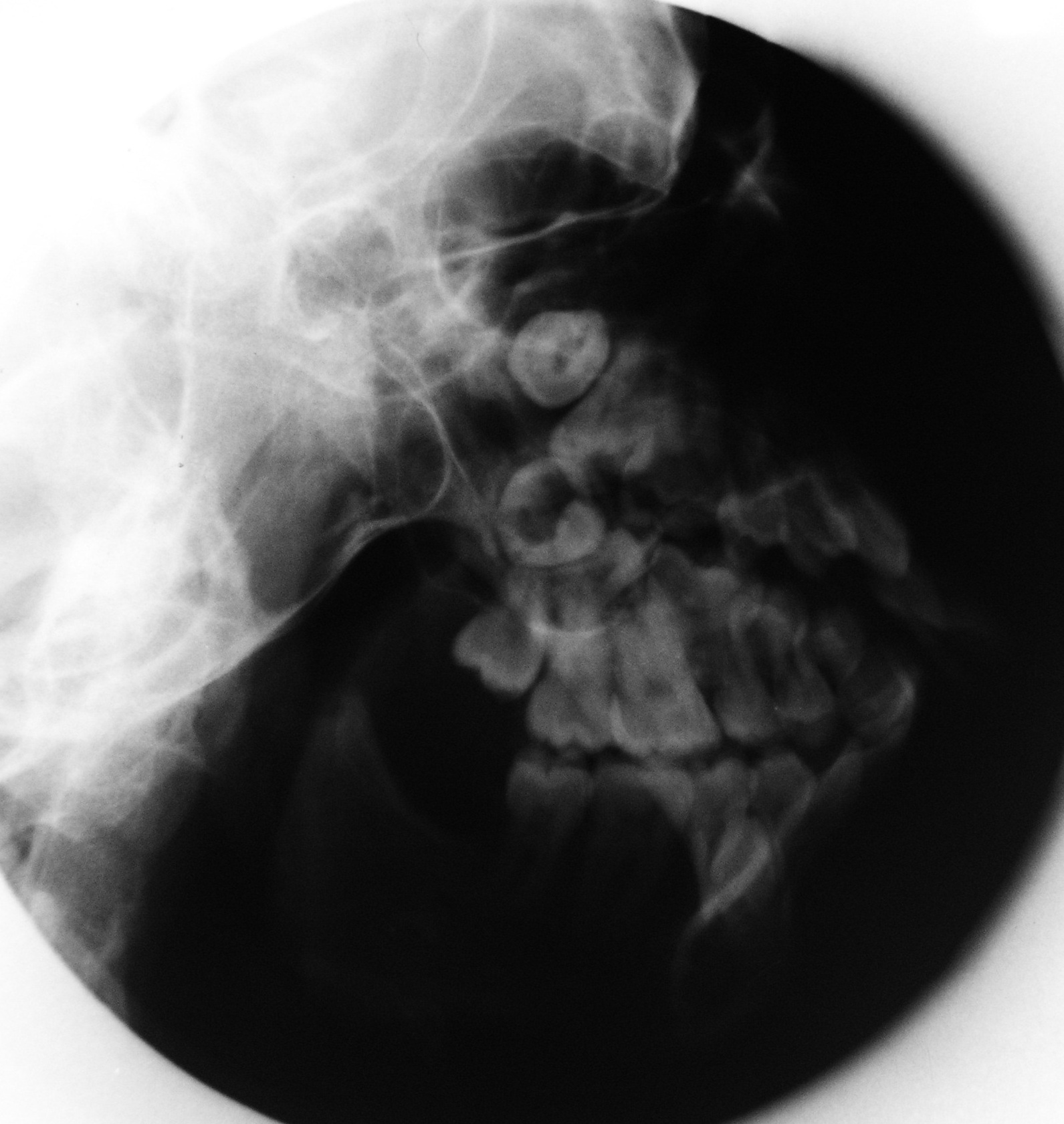
Left lateral oblique view of the mandible showing absence of upper part of ramus, condyle and coronoid on left side

On correlating the clinical and radiologic findings, a diagnosis of HFM was made and the patient was referred to Oral Maxillofacial Surgery and Orthodontia Department for aesthetic rehabilitation of hypoplastic mandible and correction of crossbite.
Case 2
A 25-year-old female patient reported to our dental hospital with the complaint of a facial asymmetry on the right side, which had been there since birth. Her history revealed that she also had paresis of the facial muscles on the right side.
On examination, a facial asymmetry was observed on the right side of the face, with the right pinna being situated at a much lower level than the left one and it was small and malformed [Table/Fig-6]. The mandible deviated towards the right side on opening the mouth, with a malocclusion. Panoramic radiographs revealed a small hypoplastic ramus and condyle on the right side, with a prominent antegonial notch [Table/Fig-7]. A Computed Tomography (CT) scan also revealed the same [Table/Fig-8]. The patient was advised to start with orthodontic treatment and to undergo plastic surgery for the gross facial asymmetry.
Facial asymmetry of the right side of the face with the small and malformed right pinna situated much lower than the left one

Panoramic radiograph revealed a small hypoplastic ramus and condyle on the right side with a prominent antegonial notch

3D CT scan showing facial asymmetry and a small hypoplastic ramus on the right side

Case 3
A 32-year-old male patient reported to the dental hospital, complaining of malaligned teeth. His history revealed that since birth, he had not been able hear through the right ear, which had been deformed and there was paralysis of facial muscles on the right side.
An extra-oral examination revealed mild facial asymmetry on the right side of the face, with a rudimentary right pinna and the presence of a preauricular skin tag [Table/Fig-9]. The external auditory meatus was also absent on the right side. The patient was unable to wrinkle his forehead or draw back the angle of his mouth on smiling on the right side. When the patient tried to close his right eye, the eyeball rotated upwards, demonstrating a positive Bell’s sign [Table/Fig-10]. An intra-oral examination revealed an open bite on left side, a missing 33 and deviation of midline towards the left side [Table/Fig-11]. Panoramic radiographs revealed a small hypoplastic ramus, condyle and coronoid process on the right side, with a prominent antegonial notch and 33 was impacted and malformed. The patient was referred for orthodontic and prosthetic treatment.
Rudimentary right pinna and the presence of preauricular skin tag with the absence of the external auditory meatus

Mild facial asymmetry on the right side of the face with positive Bell’s sign

Intra-oral picture showing open bite on left side and missing 33 and deviation of mandibular midline towards the left side

Discussion
In 1881, Hemifacial Microsomia was first described by Carl Ferdinand Von Arlt. HFM involves first and second branchial arch derivatives with highly variable phenotypes. It is also known as first and second branchial arch syndrome, otomandibular-facial dysmorphogenesis and lateral facial dysplasia [1]. HFM is primarily a syndrome of the first branchial arch, which involves underdevelopment of the temporomandibular joint, mandibular ramus, muscles of mastication and the ear. Abnormal development of the auricular hillocks leads to microtia or atresia of the pinna and it is proportional in severity to the abnormal external auditory canal development [2].
HFM is the most common congenital facial anomaly, which is second only to facial clefts [2,3]. There is a definite male predilection, with the right side being more commonly affected [4]. Abnormal accessory hillocks become preauricular tags, which were present in our patients. Hearing loss may result from underdevelopment of the osseous components of the auditory system and a diminished or absent external auditory meatus. Occasionally, second branchial arch defects which involve the facial nerve and facial muscles coexist with hemifacial microsomia.
During jaw development of vertebrate embryos, cranial neural crest cells from the posterior mesencephalic neural fold and the first rhombomeres migrate to the first pharyngeal arch to give rise to skeletal maxillo-mandibular elements [Couly et al., 2002]. In contrast, masticatory muscles are formed by 1st pharyngeal arch (PA1) cephalic. The consequence is a lateral deviation of the mandible, which is accompanied by a malocclusion and a hearing deficiency. Most of the times, the masseter muscle is found to be absent at the affected site [5].
HFM is a complex malformation syndrome with a large host of genetic and teratogenic associations and a wide spectrum of clinical features which involve the facial skeleton and other organ systems [6,7]. Deformities may include auricular defects, preauricular tags and fistulae, microtia-atresia, mandibular, maxillary, and orbital hypoplasia, micropthalmia, epibulbar dermoid, strabismus, conductive or sensoneural hearing loss, and hypoplastic facial muscles [8]. HFM which is associated with vertebral, cardiac and renal defects is called as Goldenhar syndrome. The term, ‘oculoauriculovertebral dysplasia’ (OAVD) was suggested by Gorlin for this disorder [9].
The clinical picture of HFM varies from a little asymmetry in the face, to severe under-development of one facial half, with orbital implications, a partially formed ear or even a total absence of the ear. The chin and the facial midline are off-centred, and they get deviated to the affected side. Often, one corner of the mouth is situated at a higher level than the other, giving rise to an oblique lip line. Other asymmetric symptoms are the unilateral hypoplastic maxillary and temporal bones, a unilateral shorter zygomatic arch and malformations of the external and internal parts of the ear. Auditory problems (conducive deafness) which are caused by malformations in the middle ear and facial nerve dysfunction (temporal and zygomatic branches of the facial nerve) are very common in these patients [4,5].
The two most frequently used classifications are the skeletal–auricular–soft tissue (SAT) and the orbital asymmetry–mandibular hypoplasia–ear malformation–nerve dysfunction–soft tissue deficiency (OMENS) classifications [4]. The OMENS classification is the most comprehensive one and, therefore, it is one of the most commonly used systems [6]. All 3 cases which have been reported here were classified by using OMENS classifications [Table/Fig-12].
The diverse clinical and radiographic features as seen in the three cases of HFM,, ranging from mild facial asymmetry and ear malformation to the severe facial paralysis
| Sl. No. | Features | Case 1 | Case 2 | Case 3 |
|---|
| 1 | Facial Deformity | Severe | Severe | Mild |
| 2 | Orbit size / Position | Eye located lower than positon on affected side | Normal | Normal |
| 2 | Small or Anomalous Pinna | Malformed Pinna | Small Pinna in a lower position | Rudimentary with absence of EAM |
| 3 | Pre-auricular skin tags | Absent | Absent | Present |
| 4 | Condylar aplasia/hypoplasia | Aplasia of ramus, condyle & coronoid process. | Condylar hypoplasia | Condylar hypoplasia |
| 5 | Malocclusion | Present | Present | Present |
| 6 | Impacted/ Missing teeth | Mandibular canine on contralateral side impacted. | All teeth erupted. | Mandibular canine on contralateral side impacted |
| 7 | Hearing loss | Absent | Absent | Present |
| 8 | Facial Paresis/ Palsy | Absent | Mild facial Paresis | Facial Palsy with positive Bell’s sign |
| 9 | OMENS Classification | O2 M3E2N0S3 | O0M2BE1N2S3 | O0M2BE2N3S1 |
Imaging plays an important role in establishing the diagnosis. Conventional radiography with the use of panoramic radiographs provides an easy comparison between the malformed and the normal side. CT can provide both a three dimensional rendition of the soft tissue of the face and an image of the underlying bone. It helps in establishing the degree of anatomical malformation and the relationship of the deformity to the adjacent craniofacial skeleton [7,8].
All the above case reports had almost similar clinical features and imaging findings, except that facial nerve paralysis was seen only in the third case report. Facial palsy has been reported to occur in 22%–50% of patients with HFM [9]. Diagnosis of such cases depends on a thorough medical history taking and meticulous clinical examinations. Panoramic radiographs and CT imaging substantiate the clinical diagnosis to be an accurate one.
The management of HFM necessitates a multidisciplinary approach. The surgery may be done during growth phase or after the growth phase is over. Excisions of the preauricular skin tags and cartilage remnants can remove certain amount of social stigma which is associated with this condition. Treatment options may include,limited autogenous bone grafting of deficient portions of the craniofacial skeleton, a bilateral mandibular advancement in patients with mild to moderate mandibular micrognathia, a combined Le Fort I
osteotomy, a bilateral mandibular osteotomy, genioplasty, microvascular free flaps for augmenting the soft tissue of the face on the affected side and costo-chondral grafts which can be used to provide a new growth centre for treating this anomaly [4,10].
[1]. Ross R.B., Lateral facial dysplasia (first and second branchial arch syndrome, Hemifacial microsomia)Birth Defects Orig Art Ser 1975 11:51-59. [Google Scholar]
[2]. Kapur R, Kapur R, Sheikh S, Jindal S, Kulkarni S, Hemifacial microsomia: a case reportJ Indian Soc Pedod Prevent Dent 2008 26:S34-S40. [Google Scholar]
[3]. Dhillon M, Prakash R, Mohan S, Hemifacial microsomia: a clinicoradiological report of three casesJ Oral Sci 2010 52:319-24. [Google Scholar]
[4]. Romsee MC, Verdonck A, Schoenaers J, Carels C, Treatment of hemifacial microsomia in a growing child: the importance of co-operation between the orthodontist and the maxillofacial surgeonJ. Orthod 2004 31:190-200. [Google Scholar]
[5]. Heude E, Rivals I, Couly G, Levi G, Masticatory muscle defects in hemifacial microsomia: a new embryological conceptAm J Med Genet A 2011 Aug 155A(8):1991-5.doi: 10.1002/ajmg.a.34095. Epub 2011 Jul 8 [Google Scholar]
[6]. Vento AR, LaBrie RA, Mulliken JB, The O.M.E.N.S. classification of hemifacial microsomiaCleft Palate Craniofac J 1991 28:68-77. [Google Scholar]
[7]. Cohen MM Jr, Rollnick BR, Kaye CI, Oculoauriculovertebral spectrum: an updated critiqueCleft Palate Craniofac. J 1989 26:276-86. [Google Scholar]
[8]. Mielnik-Błaszczak, Maria, Katarzyna Olszewska, “Hemifacial Microsomia–Review of the Literature.”Dent. Med. Probl 2011 48(1):80-85. [Google Scholar]
[9]. Terzis JK, Anesti K, Developmental facial paralysis: a reviewJ Plast Reconstr Aesthet Surg 2011 Oct 64(10):1318-33. [Google Scholar]
[10]. McCarthy JG, Craniofacial microsomia. Joseph Grabb and smith’s plastic surgery, sixth edition by Charles HThorneChapter 26:248-55. [Google Scholar]