Some benign jaw lesions, mostly the local aggressive ones, usually recur after surgical excisions. This is because, in most of the instances, the correct extensions remain undetected on static imaging, which may lead to inadequate resection results in recurrence. Thus, it is important to diagnose the extent of the tumour as accurately as possible.
Panoramic radiography (PR) and other structural imaging modal-ities like CT and MRI often fail to detect subtle bone changes. It is well known that 30 to 50 percent demineralisation of bone has to take place before it becomes visible on radiographs [1,2]. Bone scintigraphy may be positive even if there is approximately a ten percent increase in osteoblastic activity above normal [3]. Most of the morbid processes which involve bone result in increased turnovers or new bone formations [4]. However, some studies [5–8] have concluded that the bone scintigraphy has a high sensitivity but a low specificity. While conventional radiography (CR) which includes PR is more specific [2,9,10], it is insensitive in detecting early bone changes.
Thus, the major disadvantage of radionuclide bone scanning is its nonspecificity, which can be compensated by correlating its uptake pattern, either with radiography or tomography [11–15]. No imaging modality is adequately reliable when it is used alone. This paper investigated the value of correlating the results of these two complementary imaging modalities in defining the nature and extent of the benign lesions of the jaws.
Material and Method
Twenty patients (12 males and 8 females with a mean age 30.4 years) with benign jaw lesions (9 cysts and 11 other benign lesions) were randomly recruited for this study. All subjects underwent radiological (PR) and radionuclide (BS) examinations prior to their surgeries. These investigations were carried out on the same day or within 48 hrs of each other. BS was performed three hrs after an i.v. injection of technetium-99m methylene diphosphonate (99Tcm MDP). Antero-posterior (AP) and lateral projections were taken in all cases. If necessary, oblique or/and whole body scans were carried out. Bone scans were obtained by using a dual head gamma camera which was equipped with a parallel hole collimator. No patient had a recent history of a dental extraction/oral surgery, radiotherapy or chemotherapy. Intra-operative and histopathological examinations of surgical specimens were carried for final confirmation of extent of bone destruction. The data was gathered prospectively but it was evaluated retrospectively. All patients provided informed consents for investigation with technetium bone scan. This study followed the ethical standards of the Committee on Human Experimentation of the institution. The procedures followed were in accordance with the Helsinki Declaration of 1975, as revised in 2000.
The panoramic and scintigraphic studies were evaluated by an oral radiologist and a nuclear medicine specialist who were blinded to the histopathological findings. When disagreements existed, a final diagnosis was reached by a forced consensus. On radiographs, lesions were defined as having sclerotic margins, if at least 75% of the margins appeared to be sclerotic. Otherwise, they were defined as lesions without sclerotic margins. The scinitigraphy was assessed for rate (increased/decreased/normal), intensity (less/more) and extension of radionuclide uptake, in combination with radiography. The extension of the lesion on BS was considered to be positive when there was an asymmetrical uptake which corresponded to the clinical site of the lesion, and where PR demonstrated no evidence of any dental disease. If the site of the lesion corresponded to the site of the dental disease, it was considered to be positive only when there was an increase in size of abnormal uptake on BS as compared to the actual size of the dental disease on PR. To evaluate the efficacy of correlating scintigraphic and radiographic findings, all their results were compared with histopathological and intra–operative findings.
Results
Abnormal scintigrams and increased radionuclide uptakes were found in all cases, even in patients where the disease was expected to be stationary. There were no instances of an abnormal radiograph with a normal scintigraph. Slightly increased uptakes were present in 11 cases and markedly increased uptakes were seen in nine cases. Among 20 cases, 17 showed homogenous uptakes and three showed peripheral uptakes. Nine cysts and seven other lesions presented radiographically as well-defined bone destructions. Among these 16 cases, the extent in 15 lesions, which included 14 lesions with sclerotic borders, was correctly identified on radiographs, while the radiographic and scintigraphic extent was similar in 13 cases. The remaining four cases showed ill-defined bone destructions with absence of peripheral sclerosis on radiographs. The area of an elevated tracer accumulation on scintigraphs was extended beyond the zone of a visible bone destruction which was seen on radiographs in seven cases. The extent of bone involvement in five cases with an ‘extended uptake’ was shown to be underestimated on radiographs, but it was correctly identified on scintigraphs. Falsely extended uptakes were found in two cases. summarizes the correlation of imaging with subsequent histology.
Discussion
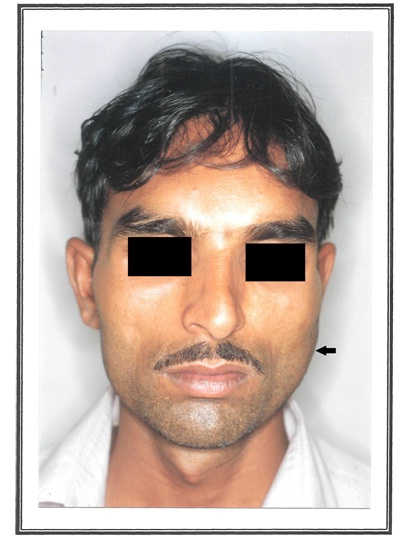
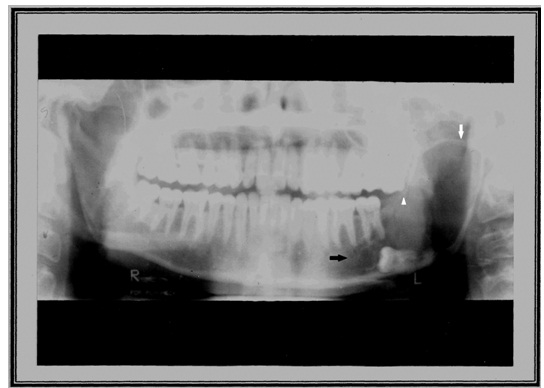
Benign jaw lesions are usually slow growing and less permiative and they provide sufficient time for host tissue to react and build up its defenses. This results in well-defined bone destructions, often with sclerotic margins. Therefore, BJL can be better studied on static imaging in terms of its extension and adjacent anatomy. In a case of mandibular dentigerous cysts [Table/Fig-1] panoramic radiographs [Table/Fig-2] showed sharply defined geographic bone destructions which were associated with sclerotic rims. But some lesions are aggressive and/or invasive and hence, their extent remains undetected on static imaging, which can lead to an incomplete excision and recurrence. On the other hand, bone scintigraphy is functional imaging and it is highly sensitive than radiography [16]. It has an ability to show physiological changes in bone and hence, it offers an earlier detection of pathology. Thus, it remains the sole technique for determining the surgical margin of the disease. However, it has been found to be non-specific [1,9] and its resolution is not as high as that of radiographs and therefore, it does not show morphological alterations. An anatomic localisation of a lesion on BS may be imprecise, unless multiple positioned views are obtained. Although, panoramic radiography is insensitive to early bone changes [8,10,17,18], it provides an excellent survey of the jaws. In addition, dental diseases are better diagnosed and differentiated on it. Thus, it provides complementary information and increases both the specificity as well as sensitivity of BS considerably. Each imaging modality has its own value. However, a combination of PR and BS is recommended in early changes [2,11]. Therefore, an integrated approach of both imagings was carried out in defining the extent and nature of the benign jaw lesions, in order to decide on the surgical margins of the lesion.
Mandibular Dentigerous cyst (←).
Panoramic radiograph shows sharply defined geographic bone destruction surrounding the crown of an unerupted tooth; sclerotic rim (↓), partial destruction of cortex (↑) and anterior extension (→) of the lesion
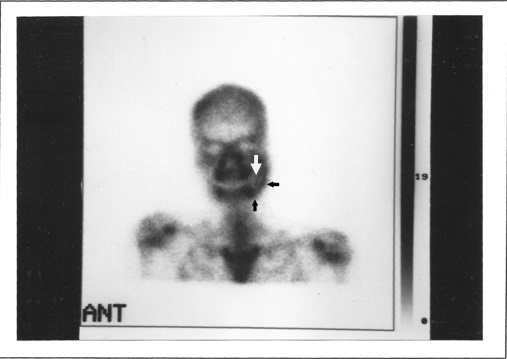
Technetium-99m has a short half-life of six hours and 140 keV gamma energy and the emitted radiation doses are far below the amounts that are toxic to human cells [19]. BS demonstrates whole skeleton at a single time with the use of a small radiation dose. Bone diseases which can be seen on BS as either an increase or decrease in radionuclide uptake, depends on the amount of disturbances in the bone metabolism. The increased uptake is in the reactive bone [20] and not in the neoplasm or inflammation. An increased uptake, namely a “hot spot”, occurs in areas of hyperaemia (may be secondary to disease) and a high osteoblastic activity. irrespective of the accumulation or loss of bone. Most of the disease processes which involve bone result in an altered osteoblastic activity. In our study, an increased uptake was seen in all cases, that suggested presence of an active metabolism. A diminished or an absent uptake, which is called as “cold spot” [4], is thought to be associated with metabolically inactive or an ischaemic bone [12, 21, 22]. We found decreased uptakes in none of our cases. A diminished uptake may be related either to a complete focal replacement of bone by tumour without any osteogenesis or an absence of blood supply to the involved region [12]. As such “cold lesions” can be observed in both benign and malignant lesions [13], a correlation between clinical and radiographic findings becomes essential. A homogenous increase in uptake indicates an increased osteoblastic activity throughout the lesion. A peripheral uptake i.e. an area of diminished uptake, which is surrounded by a zone of increased activity, indicates a large, expansile cyst or a cystic neoplasm [9, 23]. Alani A et al., [24] stated that a peripheral uptake depended on the total area of osteolysis.
In our material, a peripheral activity was found in only three cases. All were large and expansile and they caused a complete central osteolysis [Table/Fig-3]. The size as well as total area of osteolysis was small in remaining 17 cases and therefore, their uptake was homogenous. A high intensity uptake i.e. a high level of osteoblastic activity suggests a fast growing pathology [23]. This type of uptake was found in nine of our cases. A less intense uptake was found in remaining 11 cases, which suggested a quiescent disease process.
Nuclear bone scan; anterior view. Increased radionuclide uptake (← and) surrounding a focal region of diminished uptake (↓), stressing an expansile nature of the lesion
The radiographic extent was correct in 15 cases. Among these, 14 had sclerotic rims, 13 had a similar scintigraphic extent and ten showed a less intense uptake, which suggested a slow growing process. In one case, there was a well-defined bone destruction but with a partial sclerosis. Therefore, if radiographic findings present well-defined bone destructions with sclerotic margins, it can safely be assumed that the biological activity of the lesion is indeed very low. The scintigraphic extent was correctly more extended than the radiographic extent in five of total six cases with absent sclerotic rims, which suggested an aggressive or an infiltrative disease process. In such instances, the differentiation from a malignant neoplasm was difficult. Some studies found similar results [2, 25, 26].
Although several authors [2,27,28] have been using bone scan as an index for detecting the correct extent of the lesion, in order to ensure adequate surgical resection, others have shown that an “extended uptake” occurred beyond the proven limits of focal bone destruction [29–31]. In our case, two false positive uptakes which had occurred due to corresponding dental infections were correctly identified when BS was correlated with PR. Hypothesised mechanism for this phenomenon would include regional hyperaemia [22], dental diseases or peripheral tissue reactions to growing pathology. Although an increased radionuclide uptake which is beyond the obvious radiographic extent is most often a spurious “extended uptake,” our results support the contention that a surgical margin which is beyond the limits of an abnormal uptake will almost invariably be safely beyond the tumour. Chan et al., [32] suggested that invasive lesion to non-lesion ratios (uptakes) which were obtained with the use of Tc SPECT were significantly higher than in those with normal mandible or dental disease. In our study, there was no false negative result on bone scan, which indicated its extreme sensitivity. But few studies with false negative results [5,7,14] were observed. Such cases may arise because of a misinterpretation of dental diseases on scan. Correlating the bone scan with PR can be helpful in resolving such misreadings.
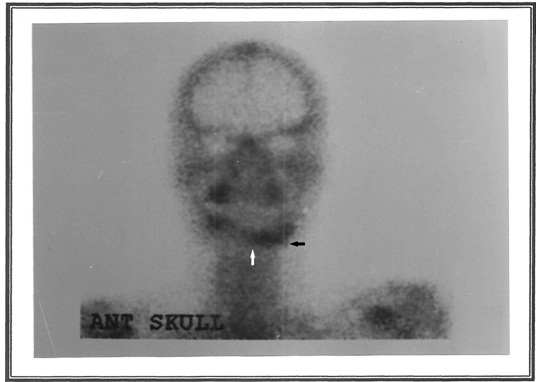
Thus, radiographic extent was correct in 15 cases and it was underestimated in five cases. One of the radiographically underestimated cases was an aggressive ameloblastoma [Table/Fig-4] in an edentulous mandible [Table/Fig-5] which had recurred after first surgery. Panoramic radiograph [Table/Fig-6] showed an ill-defined bone destruction; therefore, a nuclear bone scan [Table/Fig-7] was carried out, which detected the correct extension of the lesion.
Mandibular Ameloblastoma (←)
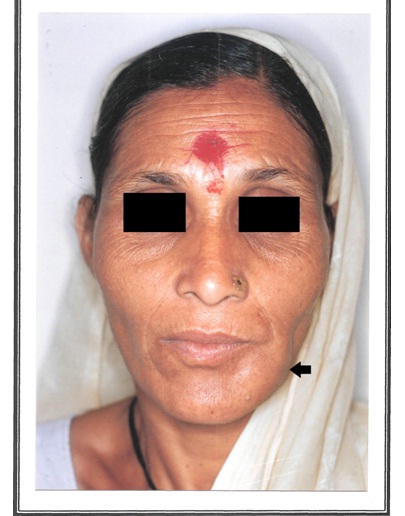
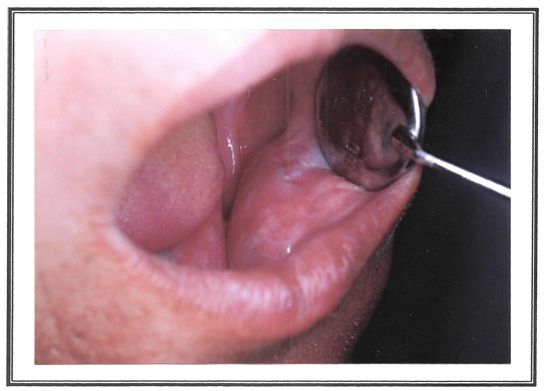
Intraoral swelling in the left side edentulous region of the mandible
Panoramic radiograph shows poorly marginated geographic bone destruction (↓)

Nuclear bone scan; anterior view shows markedly increased uptake clearly exceeding the radiographically visible extent of bone involvement (←), midline extension () but uninvolved lower border
Scintigraphic extent was correct in 18 cases and it was overestimated in two, but the true limits of skeletal involvement in all cases were accurately defined by correlating radiographs (PR) with scintigraphs (BS). PR is accurate in assessing the dimensions of the lesions when the margins are well defined [33]. In benign lesions, when margins are well–defined, however, radiographs remain the primary investigation and they usually yield enough information to determine the surgical margin. However, lesions with ill-defined margins should be carefully followed by employing both imaging modalities [Table/Fig-8].
Correlation between clinical, radiographic, scintigraphic and histopathological findings
| Histological Diagnosis | Clinical findings | Radiographic Findings | Scintigraphic Findings |
|---|
| No | Age | Sex | Region | Size in cm | Pattern of bone destruction | Sclerotic rim | Adjacent Dental pathology | Uptake |
|---|
| Intensity | Type | Extent |
|---|
| Radicular cyst | 1 | 21 | F | Mx | 4×3 | Well-defined XL | + | – | ↑ | H | S |
| 2 | 28 | M | Mx | 3×2 | Well-defined XL | + | – | ↑ | H | S |
| 3 | 24 | M | Mx | 3×2 | Well-defined XL | – | – | ↑ | H | S |
| Dentigerous Cyst | 1 | 27 | M | Md | 7×3 | Well-defined XL | + | – | ↑↑ | P | S |
| 2 | 18 | M | Mx | 4×2 | Well-defined XL | – | – | ↑↑ | H | M |
| 3 | 70 | M | Md | 7×3 | Well-defined XL | + | – | ↑ | P | S |
| Odontogenic Keratocyst | 1 | 27 | M | Md | 2×1 | Well-defined XL | + | + | ↑↑ | H | FM |
| 2 | 23 | M | Md | 3×2 | Well-defined XL | + | – | ↑ | H | S |
| Residual cyst | 1 | 22 | F | Md | 2×2 | Well-defined XL | + | – | ↑ | H | S |
| Ameloblstoma | 1 | 60 | M | Md | 7×3 | Well-defined XL | + | – | ↑↑ | P | S |
| 2 | 32 | F | Mx | 3×2 | Well-defined XL | + | – | ↑ | H | S |
| 3 | 45 | F | Md | 3×3 | Ill-defined XL | – | – | ↑↑ | H | M |
| Osteoma | 1 | 60 | M | Md | 2×1 | Ill-defined XO | – | – | ↑↑ | H | M |
| 2 | 50 | F | Md | 1×1 | Well-defined XO | + | – | ↑ | H | S |
| Cemento-Ossifying fibroma | 1 | 26 | F | Md | 4×3 | Well-defined, mix lesion | + | – | ↑ | H | S |
| 2 | 14 | F | Md | 4×3 | Well-defined, mix lesion | + | + | ↑↑ | H | FM |
| Cherubism | 1 | 12 | F | Md | 3×3 | Ill-defined XL | – | – | ↑ | H | M |
| 2 | 09 | M | Md | 3×3 | Ill-defined XL | – | + | ↑↑ | H | M |
| AOT | 1 | 21 | M | Mx | 3×2 | Well-defined, mix lesion | + | – | ↑ | H | S |
| CEOT | 1 | 20 | M | Md | 4×3 | Well-defined, mix lesion | + | + | ↑ | H | S |
AOT: Adenomatoid odontogenic tumor, CEOT: Calcifying epithelial odontogenic tumor, Mx: Maxilla, Md: Mandible, XL: Radiolucent, XO: Radiopaque, +: Present,– : Absent,: Slightly increased uptake,: Markedly increased uptake, H: Homogenous uptake, P: Peripheral uptake, S: Same as radiographic extent, M: exceeded radiographic extent, FM: falsely exceeded radiographic extent.
Conclusion
The value of a combination of radiography (PR) and scinitigraphy (BS) is very useful for diagnosing the extent of bone resection in BJL, for achieving a better treatment and prognosis.
AOT: Adenomatoid odontogenic tumor, CEOT: Calcifying epithelial odontogenic tumor, Mx: Maxilla, Md: Mandible, XL: Radiolucent, XO: Radiopaque, +: Present,– : Absent,: Slightly increased uptake,: Markedly increased uptake, H: Homogenous uptake, P: Peripheral uptake, S: Same as radiographic extent, M: exceeded radiographic extent, FM: falsely exceeded radiographic extent.