Human Gall-Bladder Communicating with Skin: Rare Anatomical Swerve
Arashdeep Singh1, Sandeep Bansal2
1 Associate Professor, Gian Sagar Medical CollegeRam Nagar Patiala, Punjab, India.
2 Senior Resident, Gian Sagar Medical CollegeRam Nagar Patiala, Punjab, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Arashdeep Singh, 941, Phase 4, Mohali Punjab, India.
Phone: 09216684739,
E-mail: docrammi@yahoo.co.in
Cholecysto-cutaneous fistula is an extremely rare phenomenon in present era. We report a case of this rare entity wherein patient presented with unique history of passage of stones per umbilicus. Newer radiological investigations specifically CT fistulography help in surgical planning by not only delineating external fistulas but only diagnosing any internal fistula.
Cholecysto-umbilical, Fistula, CT
Introduction
Cholecysto-umbilical fistula (CCF) is an abnormal epithelial lined tract connecting gall bladder and the umbilicus. It is an extremely rare complication in present era, about 25 cases have been reported in last 50 years. Most of such cases are caused by neglected cholelithiasis or cholecystitis. Cholecysto-umbilical fistula is a diagnostic challenge to attending surgeon, wherein specific history like passage of stones or yellow discharge through fistulous opening may be leading dictation. However, in present era, modalities like Computed Tomography (CT), specifically CT fistulography, not only delineates the fistulous tract accurately, but it also provides sufficient information of rest of abdominal organs (like status of common bile duct, pancreas, liver), thus aiding in preoperative planning of such cases. Management of this rare entity includes broad spectrum antibiotics, elective cholecystectomy, with complete excision of fistulous tract.
Case Report
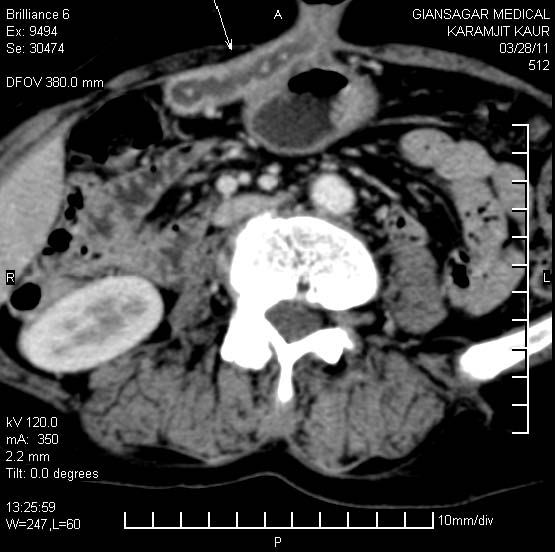
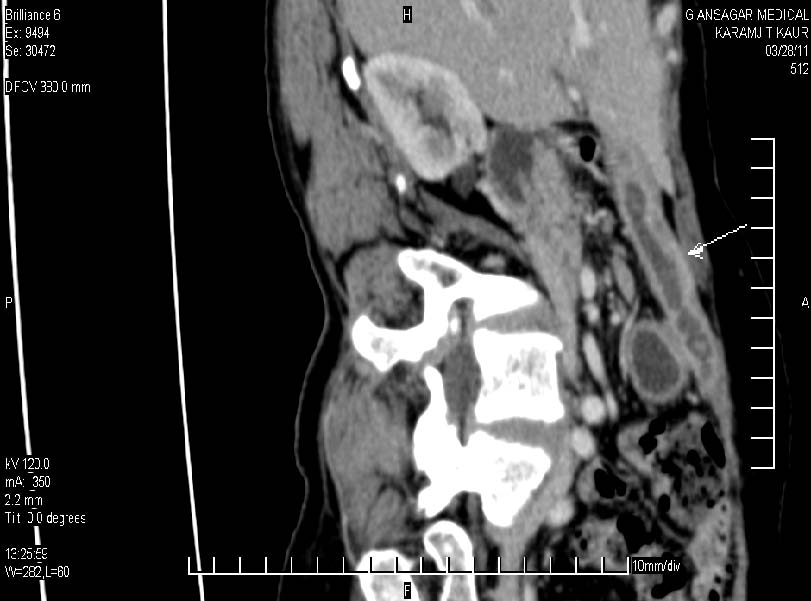
Yellowish watery discharge and passage of stones since past two months is not a routine quotidian history for a 60-year-old lady. Besides this history, our patient also complained of “on and off” fever and right hypochondriac pain since last two years. Clinical examination revealed patient to be well built, afebrile with mildly raised total leucocyte count. Hepatic function tests were normal. Culture of fluid discharged through umbilicus showed a sterile picture. Patient was referred to Radiology Department for ultrasonography and CT scan. Ultrasonography showed “contracted” gall bladder” with thick walls, suggestive of chronic cholecystitis. Contrast enhanced CT performed subsequently showed fistulous tract with enhancing walls, extending from gall bladder fossa to umbilicus, just below anterior abdominal wall [Table/Fig-1 and 2]. This fistulous tract showed hyperdense foci, suggestive of calculi. Common bile duct was normal. CT fistulography was further performed by injecting “diluted contrast” into the fistula, through the external opening at umbilicus, which confirmed the findings [Table/Fig-3]. No ramifications were seen from the tract. Based on radiological and clinical findings, diagnosis of spontaneous cholecysto-umbilical fistula was made and patient was planned for cholecystectomy, with exploration and excision of fistulous tract.
CECT abdomen showing fistulous tract with thick walls underlying anterior abdominal wall opening at umbilicus. Small hyperdense foci are seen in lumen of this tract s/o calculi
Curved reconstructed CT image showing exact extent of the fistulous tract extending it from the region of gall bladder and opening externally at umbilicus
CT fistulography demonstrating no ramifications from the fistulous tract. Filling defects s/o calculi are seen the lumen of the tract

Discussion
Cholecystocutaneous fistula is extremely rare phenomenon since the advent of potent antibiotics and liberal cholecystectomies, with no more than 25 cases being reported in literature in last 50 years [1]. Spontaneous cholecystocutaneous fistula presents after grossly or repeated neglected episodes of cholecystitis, with a ‘painless’ draining fistula opening any where in abdominal wall in right upper quadrant, right iliac fossa, umbilicus or left upper quadrant, with literature also suggesting its opening as far as right groin and right gluteal region [2,3].
Increased intra-luminal pressure in gall bladder caused by obstruction, impairs blood flow and lymphatic drainage, leading to mural necrosis and perforation, which can lead to biliary peritonitis. When process is chronic, it can lead to internal or external biliary fistula formation [1]. These fistulas often arise from fundus of gall bladder, as in present case [3,4].
Thorough history and high level of suspicion is required to diagnose such external biliary fistulas, with classic presentation of this condition being “persistant discharging sinus” with history of gall bladder disease [5]. Diagnostic techniques like ultrasonography may help in diagnosis of cholelithiasis. However, ultrasonography is not a good modality for demonstration of fistulous tract. Hence, computed tomography (CT) scans should be performed for all cases of unexplained abdominal wall suppuration or cellulitis [6] which may delineate the fistulous tract, as in our case. CT fistulography is a newer and non invasive technique which is performed by injecting diluted contrast through fistulous opening. It helps us not only in exact delineation of course of the fistulous tract, its relation to adjacent abdominal organs, but also helps in excluding any associated internal fistula. This information is extremely important for surgical planning of patient.
Management of cholecystocutaneous fistula includes broad spectrum antibiotics, drainage of abscess if any and elective cholecystectomy, with complete excision of fistulous tract [7]. Since patients with CCF are often elderly, with associated co-morbidities, “laparoscopic” cholecystectomy may be a better option than ‘open” cholecystectomy, due to more level of stress associated with latter surgery [8].
Conclusion
Clinical history of yellowish discharge and specifically, passage of stones per umbilicus, should raise high degree of suspicion in mind of attending surgeon, of a ubiquitous gall bladder disease with cholecystocutaneous fistula. Newer radiological services such as Computed Tomography (specifically CT fistulography) may be of great help, not only for diagnosing this rare entity, but also in surgical planning.
[1]. Ijaz S, Lidder Mohamid W, Thompson HH, Cholecystocutaneous Fistula Secondary to Chronic Calculous CholecystitisCase Reports in Gastroentrology 2008 2:71-5. [Google Scholar]
[2]. Davies CJ, Fontaine CJ, Spontaneous cholecysto-umbilical fistulaThe British Journal of Radiology 1984 57:1034-6. [Google Scholar]
[3]. Nicholson T, Born MW, Garber E, Spontaneous cholecystocutaneous fistula presenting in the gluteal regionJ Clin Gastroentrol 1999 28(3):276-7. [Google Scholar]
[4]. Vasanth A, Siddiqui A, O’Donnell K, Spontaneous cholecystocutaneous fistulaSouth Med J 2004 97(2):183-5. [Google Scholar]
[5]. Flora HS, Bhattacharya S, Spontaneous cholecystocutaneous fistulaHPB 2001 3(4):279-30. [Google Scholar]
[6]. Ruy Jorge Cruz Junior, Jorge Nahas, Luiz Francisco Pole de Figueiredo, Spontaneous cholecystocutaneous fistula: a rare complication of gall bladder diseaseSao Paulo Med J 2006 124(4):234-6. [Google Scholar]
[7]. Sayed L, Sangal S, Finch G, spontaneous cholecystocutaneous fistula: A Rare Presentation of GallstonesJournal of Surgical Case Reports 2010 5:5 [Google Scholar]
[8]. Malik AH, Nadeem M, Ockrim J, Complete laparoscopic management of cholecystocutaneous fistulaUlster Med J 2007 76:166-7. [Google Scholar]