Eosinophilic Cystitis Mimicking Bladder Tumour – A Rare Case Report
Manimaran D1, Karthikeyan T M2, Sreenivasulu M3, Mrinalini V R4, Gopinath V5
1 Associate Professor, Department of Pathology, Melmaruvathur Adhiparasakthi Institute of Medical Sciences & Research, Tamilnadu, India.
2 Associate Professor, Department of Pathology, Melmaruvathur Adhiparasakthi Institute of Medical Sciences & Research, Tamilnadu, India.
3 Assistant Professor, Department of Pathology, Melmaruvathur Adhiparasakthi Institute of Medical Sciences & Research, Tamilnadu, India.
4 Professor & HOD, Department of Pathology, Melmaruvathur Adhiparasakthi Institute of Medical Sciences & Research, Tamilnadu, India.
5 Assistant Professor, Department of Urology, Melmaruvathur Adhiparasakthi Institute of Medical Sciences & Research, Tamilnadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Karthikeyan T M, Associate Professor, Department of Pathology, Melmaruvathur Adhiparasakthi Institute of Medical Sciences & Research, Tamilnadu, India.
Phone: 9994743277,
E-mail: karthikyan.tmariappan@gmail.com
A 16–year–old male presented with urinary urgency, a frequency of 4 months duration and intermittent gross haematuria which were there since one month. Eosinophilia was noted in complete blood count and CT KUB with contrast showed a filling defect in the right lateral wall, over the vesicoureteric junction. Cystoscopy revealed a sessile mass lesion over right vesico–ureteric junction, with bullous oedema . Rest of the mucosa was normal. Transurethral resection of lesion was performed and histological examination showed features of eosinophilic cystitis. Patient was treated with corticosteroids, antimicrobial agents and antihistaminics and he is recovering well. We are presenting this case for its rare presentation and its possibility of mimicking a bladder tumour. Biopsy of the lesion was diagnostic and an early treatment showed good results.
Eosinophilic cystitis, Urinary bladder
Introduction
Eosinophilic cystitis is a rare and a poorly understood clinico–pathologic entity which mimics bladder tumours. It is characterised by extensive local eosinophilic infiltration of all layers of bladder wall. Even though many aetiological factors have been proposed, the exact mechanism of the lesion remains obscure. According to van der Ouden, the most common presenting symptoms are urinary frequency (67%), dysuria (62%), gross/ microscopic haematuria (68%), suprapubic pain (49%) and urinary retention (10%) [1].
Case Report
A 16 year old male presented to our Urology Department with complaints of urinary urgency, a frequency of 4 months duration and intermittent gross haematuria of one month’s duration. He had no history of bronchial asthma, hypertension, diabetes mellitus or drug allergy. His general physical examination was unremarkable. A routine haematological examination showed peripheral eosinophilia (10%). His biochemical profile was within normal limits. Analysis of midstream urine showed RBCs- 25-30 / HPF, pus cells -3-5 /HPF and few epithelial cells. Urine culture showed no growth. Urine cytology showed squamous cells and some atypical urothelial cells. A malignancy was therefore suspected and CTKUB with contrast and a cystoscopic examination of bladder were performed.
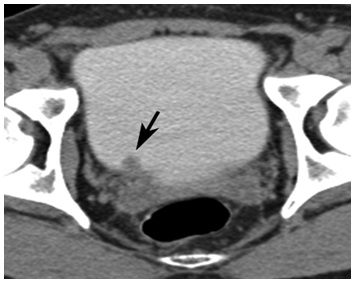
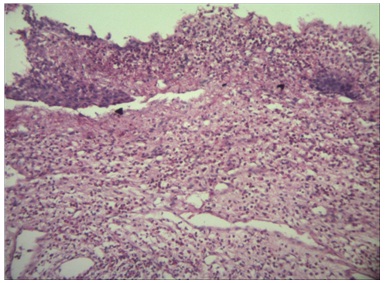
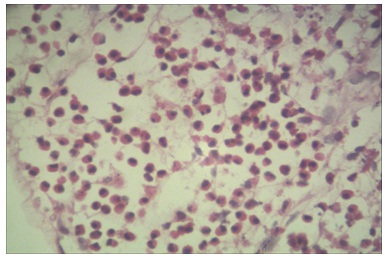
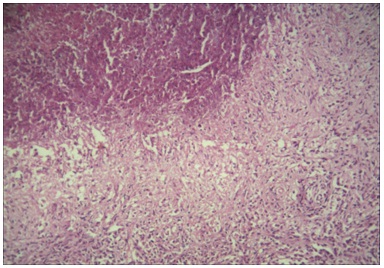
CTKUB showed a filling defect in the right lateral wall of bladder near vesicoureteric junction [Table/Fig-1]. Cystoscopy showed a mass lesion which measured 1.5x1x0.5 cm, over right vesicoureteric junction .Transurethral resection of the lesion was carried out and the sample was subjected to a histopathological examination. Grossly, the specimen consisted of grey white soft tissue fragments which measured 1.5x1x0.5 cm. Microscopy showed an ulcerated transitional epithelium with stromal oedema and congested blood vessels [Table/Fig-2]. There was diffuse infiltration of mucosa by eosinophils and few lymphocytes, with areas of haemorrhage and inflammatory necrosis [Table/Fig-3 and 4]. There was no evidence of malignancy or parasites in the sections which were studied.The patient was treated with corticosteroids, antimicrobial agents and antihistaminics and his post–operative period was uneventful. Until recent follow up, the patient was asymptomatic and there was no recurrence.
CTurogramsobtained during excretory phase show a 12-mm mass (arrow) near the right ureterovesical junction
Bladder biopsy with denuded epithelium, mucosal edema and infiltration by eosinophils into lamina propria.(H&E X 10)
Edematous lamina propria with infiltration by plenty of eosinophils.(H&E X 40)
Inflammatory necrotic area (left upper corner) seen along with viable tissue showing inflammatory infiltrate.(H&E X 10)
Discussion
Eosinophilic cystitis, a rare inflammatory disorder of urinary bladder which is of uncertain aetiology, was first described in 1960 by Brown and Palubinskas [2]. It has been reported in patients with a history of vesical injuries, chronic vesical irritation, bladder surgery, parasitosis, allergy to food and drugs, malignancies and other conditions [3–5]. The mean age at diagnosis is 41.6 years, with an equal distribution in both sexes [4]. Our case was unique in that it had occurred in a male boy who was aged sixteen years, who did not have any other associated disorder.
Patients usually present with dysuria, frequency, nocturnal enuresis, suprapubic pain and recurrent haematuria [6,7]. Our patient presented only with dysuria, frequency and intermittent haematuria, but without nocturnal enuresis and suprapubic pain. Peripheral eosinophilia was also observed, but not in the range of hypereosinophilic syndrome [4,8]. Some patients with eosinophilic cystitis present with pyuria and a positive urine culture [9]. Our patient presented with peripheral eosinophilia and a negative urine culture.
The cystoscopic abnormalities are usually associated with a wide spectrum of findings which range from mucosal erythema to fungating mass lesions. While patients with localised form of disease are more commonly associated with bladder injuries, patients with diffuse bladder involvement are associated with allergic diathesis like asthma, allergic gastroenteritis, etc [8]. In the present case, patient presented only with peripheral eosinophilia and there was no history of allergy or drug intake. From our observations, it is imperative that clinicians should be aware of varied presentations.
Since cystoscopy cannot distinguish eosinophilic cystitis from other conditions such as bladder neoplasms or other benign inflammatory diseases, a histopathological examination is mandatory [10]. The gold standard for diagnosing such lesions is deep bladder biopsy. Otherwise, the diagnosis can be missed. Histological changes can be acute, chronic or mixed. The acute changes are characterised by oedema and congestion, with transmural eosinophilic infiltrates. There can be mucosal ulceration, muscle necrosis and muscle fibrosis [6,7].
Treatment of eosinophilic cystitis is based on resection of bladder lesion, followed by treatment with antihistaminics, corticosteroids and antibiotics, as well as removal of possible allergens [9]. In refractory cases, cyclosporine and azathioprine are recommended [4,10,11].Partial cystectomies were performed in cases of circumscribed lesions, that showed no tendency of disappearing spontaneously [11]. The cure rate was 81.7 % in a series of 147 cases [12]. Most of the patients were cured but recurrence is a frequent finding.
Eosinophilic cystitis is a very rare entity with varying clinical features and it should be included in the differential diagnosis of various mass lesions of bladder. A histological examination is the gold standard method, which should be used for establishing the diagnosis. Early detection and a prompt treatment are expected, for better outcomes.
[1]. Van den Ouden D, Diagnosis and management of eosinophilic cystitis: a pooled analysis of 135 casesEur Urol 2000 Apr 37(4):386-94. [Google Scholar]
[2]. Brown EW, Eosinophilic granuloma of bladderJ Urol 1960 83:665-68. [Google Scholar]
[3]. Thompson RH, Dicks D, Kramer SA, Clinical manifestations and functional outcomes in children with eosinophiliccystitisJ Urol 2005 Dec 174(6):2347-9. [Google Scholar]
[4]. Pomeranz A, Eliakim A, Uziel Y, Gottesman G, Rathaus V, Zehavi T, Eosinophilic Cystitis in a 4-Year-Old Boy: Successful Long-Term Treatment With Cyclosporin APediatrics 2001Dec 108(6):e113 [Google Scholar]
[5]. Hellstrom HR, Davis BK, Shonnard JW, Eosinophilic cystitis.A study of 16 casesAm J Clin Pathol 1979 Nov 72(5):777-84. [Google Scholar]
[6]. Teegavarapu PS, Sahai A, Chandra A, Dasgupta P, Khan MS, Eosinophilic cystitis and its managementInt J Clin Pract 2005 Mar 59(3):356-60. [Google Scholar]
[7]. Galutira PJ, Canonigo BB, Cabansag MR, Bolong DT, Ong RC, Lopez RA, Presenting manifestations of eosinophilic cystitis in two Filipino childrenInt Urol Nephrol 2010 Sep 42(3):557-63. [Google Scholar]
[8]. Popert RJ, Ramsay JW, Owen RA, Fisher C, Hendry WF, Eosinophilic cystitis mimicking invasivebladder tumour: discussion PaperJ R Soc Med 1990 Dec 83(12):776-89. [Google Scholar]
[9]. Popescu OE, Landas SK, Haas GP, The spectrum of eosinophilic cystitis in males: case series and literature reviewArch Pathol Lab Med 2009 Feb 133(2):289-94. [Google Scholar]
[10]. Salman M, Al-Ansari AA, Talib RA, El Malikel F, Al-Bozaom IA, Shokeir AA, Eosinophilic cystitis simulating invasive bladder cancer: a real diagnostic challengeInt Urol Nephrol 2006 38(3-4):545-08. [Google Scholar]
[11]. Verhagen PC, Nikkels PG, de Jong TP, Eosinophilic cystitisArch Dis Child 2001 Apr 84(4):344-06. [Google Scholar]
[12]. Mu-Tsun Shih, Tai-Lung Cha, Guang-Huan Sun, Dah-Shyong Yu, Chih-Wei Tsao, Eosinophilic Cystitis Simulating Invasive Bladder Cancer:Report of a Case and Review of the LiteratureJ Med Sci 2012 32(3):139-42. [Google Scholar]