Systemic Mastocytosis: Predominantly Involving the Bone, A Case Report
Ketan P Mallya1, Sushma Belurkar2, Annamma Kurian3, Laxmi Rao4, Bikash Singhania5
1 Specialty Medical Officer, Department of Pathology, Melaka Manipal Medical College, Manipal, Karnataka State, India.
2 Associate Professor, Department of Pathology, Kasturba Medical College, Manipal, Karnataka State, India.
3 Associate Dean and HOD, Department of Pathology, Melaka Manipal Medical College, Manipal, Karnataka State, India.
4 Professor, Department of Pathology, Kasturba Medical College, Manipal, Karnataka State, India.
5 Post-Graduate Student, Department of Pathology, Kasturba Medical College, Manipal, Karnataka State, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Ketan P Mallya, Speciality Medical Officer, Department of Pathology, Melaka Manipal Medical College, Manipal, Karnataka State, India.
Phone: 9535138593,
E-mail: Mallya.ketan@manipal.edu
Systemic mastocytosis (SM) is a rare clonal disorder of mast cells that can range from chronic smouldering type to aggressive mast cell leukaemia. It presents with non–specific symptoms like urticaria pigmentosa, unexplained flushing, hypotension and abdominal cramps, which may lead to a misdiagnosis, if there is no high index of clinical suspicion. This is a case report of a 52–year–old lady, with systemic mastocytosis, who presented with severe chronic back ache and no other clinical features. X – ray revealed lytic lesions in the lumbar vertebrae and bone marrow aspiration and a trephine biopsy examination showed infiltration by mast cells, with a positivity for Toluidine blue stain and CD 117. She was also noted to have peripheral eosinophilia, which is frequently encountered with this condition. She was diagnosed to have chronic indolent systemic mastocytosis which involved the bone predominantly.
Case Presentation
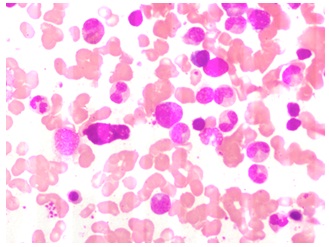
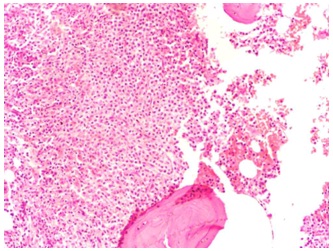
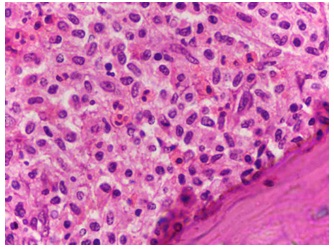
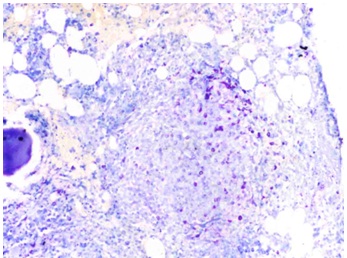
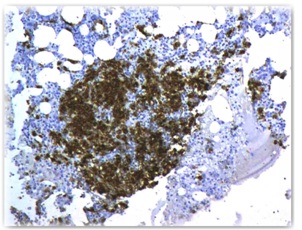
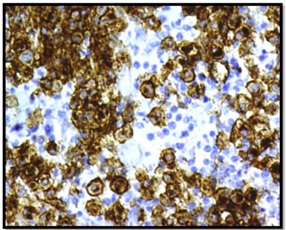
A 52–year–old lady presented with severe upper and lower back ache since 8 months. There was no obvious precipitating factor for the backache. She did not give any history of abdominal cramps, unexplained flushing or skin lesions. She had no major illnesses in the past. On examination, severe tenderness was seen in the lumbar region. There was no organomegaly. X – ray of the spine showed lytic lesions in the L1 – L5 vertebrae. Her blood counts and routine biochemical tests were within normal limits, except for eosinophilia (11%) in peripheral blood. Erythrocyte sedimentation rate was increased to 66 mm/ Ist hour. Common infectious diseases which affected bone predominantly were ruled out by further investigations. Serum protein electrophoresis was normal. Endoscopy was also normal, except for pan-gastritis. Hence, a bone marrow aspiration and a trephine biopsy were requested, for further evaluation. The aspirate showed myeloid hyperplasia with mild increase in mast cells and eosinophils [Table/Fig-1]. The bone marrow trephine biopsy showed a cellular marrow with focal aggregates of hypo-granulated mast cells. The cells were polygonal to spindle shaped, mainly arranged in sheets and whorls, which were seen in the Para trabecular areas. Eosinophilia was present and surrounding marrow showed myeloid hyperplasia with normal erythroid and megakaryocytic series [Table/Fig-2 and 3]. In Toluidine blue stained sections, the cytoplasmic granules within neoplastic mast cells stained metachromatically along with background granular staining [Table/Fig-4]. The sections which were stained with CD 117 showed positivity in the neoplastic mast cells [Table/Fig-5 and 6]. Patient was asked to follow up at the OPD for further treatment.
Bone marrow aspirate showing eosinophils and a mast cell, Wright – Giemsa stain; (400 X)
Bone marrow biopsy with Para trabecular infiltration of mast cell, H&E stain; (100 X)
Para trabecular infiltration of spindle shaped mast cells with many eosinophils; H&E stain (400 X)
Toluidine blue stain with positive staining in the mast cells (100X)
Positive staining by immunohistochemistry in mast cells with CD 117(Low magnification)
Higher magnification of staining with CD 117
Discussion
Systemic mastocytosis is a heterogenous disorder with varied clinical presentations. When bone is involved, both lytic and sclerotic bone lesions are seen, which are caused by heparin, prostaglandin and histamine releases respectively. Fractures of the bones (long bones -10-20% and vertebrae -3-10%) are commonly encountered [1].
Criteria for diagnosis [
2–
5]
According to WHO criteria, one major and one minor or three minor criteria should be present, to diagnose the disorder.
Major
Multifocal dense aggregates of mast cells are detected in sections of bone marrow and are confirmed by tryptase immunohistochemistry or special stains.
Major
Biopsies should show > 25% mast cells with an atypical morphology or in aspirate smears, > 25% cells must be immature or atypical.
Mast cells co-express CD117 with CD2 and/or CD25.
Detection of KIT point mutation at codon 816 in bone marrow, blood or other extra–cutaneous organs.
A serum tryptase level of ≥20 ng/ml.
In patients with an associated clonal haematologic neoplasm, diagnosis of systemic mastocytosis by using the WHO criteria could be difficult [4].
Indolent systemic mastocytosis has a good prognosis and transformation into an aggressive variant or development into another haematological malignancy is infrequent. Isolated bone marrow mastocytosis and smoldering systemic mastocytosis are subtypes of ISM, that present with particularly low and high burdens of disease respectively. Unlike other more aggressive variants of mastocytosis, organopathy which is related to mast cell-infiltration is not seen in indolent systemic mastocytosis, despite the high mast cell burden.
In our patient, one major criterion (multifocal dense infiltrates of mast cells in bone marrow sections, with positive special stains) and one minor criterion (greater than 25% of mast cells being spindle shaped and hypogranulated) were present. However, there were no skin lesions, gastro intestinal symptoms or organomegaly. The patient also had peripheral blood eosinophilia, as well as the eosinophils were increased in the bone marrow, which is Frequently seen in association with SM. Eosinophilia can be one of the prognostic factors in SM, especially when it is associated with FIP1L1/PDGFR α mutation, as it helps in targetted therapy [3].
Stem cell factor and mutations of its receptor c–kit proto–oncogene play a critical role in mast cell proliferation and dysregulation (a point mutation at Val 816 for Asp) [6]. Mastocytosis, in the absence of skin lesions, could be very aggressive. Imatinib mesylate therapy might result in complete remission of SM cases with wild type KIT and certain KIT mutations such as F522C, or the FIP1L1-PDGFR α fusion gene, but not of D816V-KIT-bearing SM [6].
Conclusion
Systemic mastocytosis is a rare disorder that could be misdiagnosed due to its nonspecific clinical presentations, which can lead to a delay in treatment. A high index of clinical suspicion is needed in this regard. In our patient who presented with severe back pain of 8 months duration, with no other symptoms to aid the diagnosis, a bone marrow aspiration and trephine biopsy examination clinched the diagnosis.
[1]. Horney Hans-Peter, Valent Peter, ‘Diagnosis of mastocytosis: General histopathological aspects, morphological criteria and immunohistochemical findings’Leukemia Research 2001 25:543-51. [Google Scholar]
[2]. Brockow Knut, Akin Cem, Huber Mary, Metcalfe Dean D, ‘Assessment of the extent of cutaneous involvement in Children and adults with mastocytosis: Relationship to symptomatology, tryptase levels and bone marrow pathology’J. Am. Acad. Dermatol 2003 (48):508-16. [Google Scholar]
[3]. Walz Christoph, Subklewe Marion, Horny Hans-Peter, Flaig Michael, Reiter Andreas, Kirchner Thomas, ‘Advanced systemic mastocytosis as a mimicker of metastatic clear cell renal cell carcinoma’Leukemia Research 2012 36:799-801. [Google Scholar]
[4]. Akin Cem, Scott Linda M, Metcalfe Dean D, ‘Case report; slowly progressive systemic mastocytosis with high mast-cell burden and no evidence of a non-mast-cell hematologic disorder: an example of a smoldering case?’Leukemia Research 2001 25:635-38. [Google Scholar]
[5]. Pardanani A, Akin C, Valent P, ‘Pathogenesis, clinical features, and treatment advances in mastocytosis’Best Practice and Research Clinical Haematology 2006 19(3):595-615. [Google Scholar]
[6]. Alvarez-Twose Ivan, de Olano David Gonzalez, Sanchez-Munoz Laura, Matito Almudina, Esteban-Lopez Maria I, Vega Arantza, ‘Clinical, biological and molecular characteristics of clonal mast cell disorders presenting with systemic mast cell activation symptoms’J. Allergy Clin.Immunol 2010 125:1269-78. [Google Scholar]