Tuberculosis is an ancient disease but is still a major public health problem in most of the world [1]. Tuberculosis appears to be increasing throughout the world due to various factors like increasing number of immunocompromised patients, aging population, multiple drug resistant strains of the bacillus [2]. Though pulmonary tuberculosis is the most common form, extrapulmonary tuberculosis (EPTB) also contributes to significant morbidity and mortality. The various extrapulmonary sites are lymph nodes, intestines, bone, joints, meninges, genitourinary tract etc. [3]. Osteoarticuar tuberculosis comprises 1-4.3% of all tuberculosis cases [4–6] and 10-15% of all extrapulmonary tuberculosis cases [2,7].
Bone and joint TB (BJTB)/ osteoarticular TB is a secondary form of TB occuring most commonly due to hematogenous seeding [2,5,8]. Retrograde lymphatic and contiguous dissemination are the other less common modes of dissemination [8].
Several studies have demonstrated spinal involvement in a significant number of cases [1,2,6]. However contradictory findings have been found in some other studies [8,9]. Watts and Lifeso, in a review of current concepts of Bone and Joint TB mentioned that spinal tuberculosis has existed for at least 5000 years, and mummified remains from northern Egypt dating 3400 B.C. provide strong evidence of its presence. The authors also mention that the first known description of tuberculous spondylitis was written in Sanskrit, sometime between 1500 and 700 B.C [1]. In the late eighteenth century, Pott provided the classic description of spinal TB and noted its association with paraplegia [1,10].
Osteoarticular tuberculosis can cause significant morbidity and a high index of suspicion is needed for early diagnosis so as to avoid destruction and disability [2,4,10]. Even with adequate medical and surgical treatment, osteoarticular TB can be associated with morbidity and mortality [11]. EPTB usually takes the form of arthritis or osteomyelitis. Rarely it can present as tenosynovitis or bursitis. The common sites of involvement are spine and weight bearing joints. Osteoarticular tuberculosis is commonly encountered in the elderly in developed countries but in developing countries like India it is common around 30 years of age.
Studies have been carried out upon epidemiology, clinical aspects and therapeutic strategies for pulmonary tuberculosis. But, studies available on extra pulmonary tuberculosis, with reference to incidence and bacteria positivity are scarce [12]. Musculoskeletal TB has been infrequently reported especially in developed world [13]. We retrospectively reviewed all the cases of osteoarticular tuberculosis and focused the study on clinicao-morphological features and response of the patients to ATT. The aim was to define the role of histopathological examination in a laboratory where advanced molecular methods of diagnosis and mycobacterial culture were not available.
Material and Methods
The study was retrospective in nature and the data collected was for the duration of 3 years. The cases were retrieved from the histopathology section of the Department of Pathology, Teerthanker Mahaveer Medical College, Moradabad between Jan 2010 to Dec 2012. A total of 16 cases were diagnosed as/suspected to be tuberculosis of bones and/ joints. The clinical information including age, sex, site, and duration of illness, symptoms, local examination findings, provisional diagnosis and X-ray findings were noted from the case files. Haemoglobin, TLC, DLC and ESR were done routinely at our haematology laboratory. In 2 cases synovial fluid was subjected to routine culture and sensitivity. ESR was available in 12 cases.
The operative procedure varied according to the case, comprising arthrotomy and debridement, synovial biopsy, aspiration of pus, cord decompression etc. In 4 cases the operative necrotic/purulent material was sent for AFB detection by smear examination. The biopsy samples were examined grossly and processed using the routine histopathologic technique (fixation and paraffin embedding) and then stained with Haematoxylin-Eosin.
Ziehl–Neelsen (ZN) stain was used to detect tubercular bacilli and Periodic acid-Schiff (PAS) stain to rule out fungal infection. Microscopic features, with emphasis on necrosis, granulomas and giant cells were noted, along with any identifiable parent tissue. The follow up record was analysed with respect to compliance and response to ATT.
Results
A total of 16 cases with histopathologic findings confirming TB or suspicious of tuberculosis of bone and/ joint were found during the study period. The ages of patients were in a wide range of 6 to 60 years with an average being 23.6 years; however maximum number of cases (81.25%)were seen between 11 and 30 years. A single patient aged 6 years and an elderly aged 60 years were identified [Table/Fig-1]. Sex distribution revealed slight male predominance with male to female ratio of 1.3:1 [Table/Fig-2].
Distribution of cases according to age
| Sr. No. | Age group (years) | No. of cases | % |
|---|
| 1 | 0 – 10 | 1 | 6.25 |
| 2 | 11 – 20 | 7 | 43.75 |
| 3 | 21 – 30 | 6 | 37.50 |
| 4 | 31 – 40 | 1 | 6.25 |
| 5 | 41 – 50 | - | - |
| 6 | 51 – 60 | 1 | 6.25 |
| Total | | 16 | 100 |
Distribution of cases according to sex
| S. No. | Sex | No. of cases | % |
|---|
| 1 | Males | 9 | 56.25 |
| 2 | Females | 7 | 43.75 |
| Total | | 16 | |
The commonest symptom was pain with swelling. In 3 cases, pain was noted after local trauma. Only one case had constitutional symptom in the form of fever. The duration varied from 2 months to 1 year. 2 of the 3 cases of spinal TB had paraplegia. One patient presented with multiple sinuses over an ankle and Madura foot was suspected. 2 cases of knee joint TB presented with cold abscess.Variable local X-ray findings like osteolytic lesion, osteopenia, periarticular erosion, reduced joint space were noted. In 2 cases, X-ray was normal. None of the cases had chest X-ray reports. ESR was raised in 12 cases; maximum recorded was 52 mm. Tuberculosis was suspected clinically in 7 cases (44%), considering the fact that TB is rampant in this geographical region. All the cases were HIV negative.
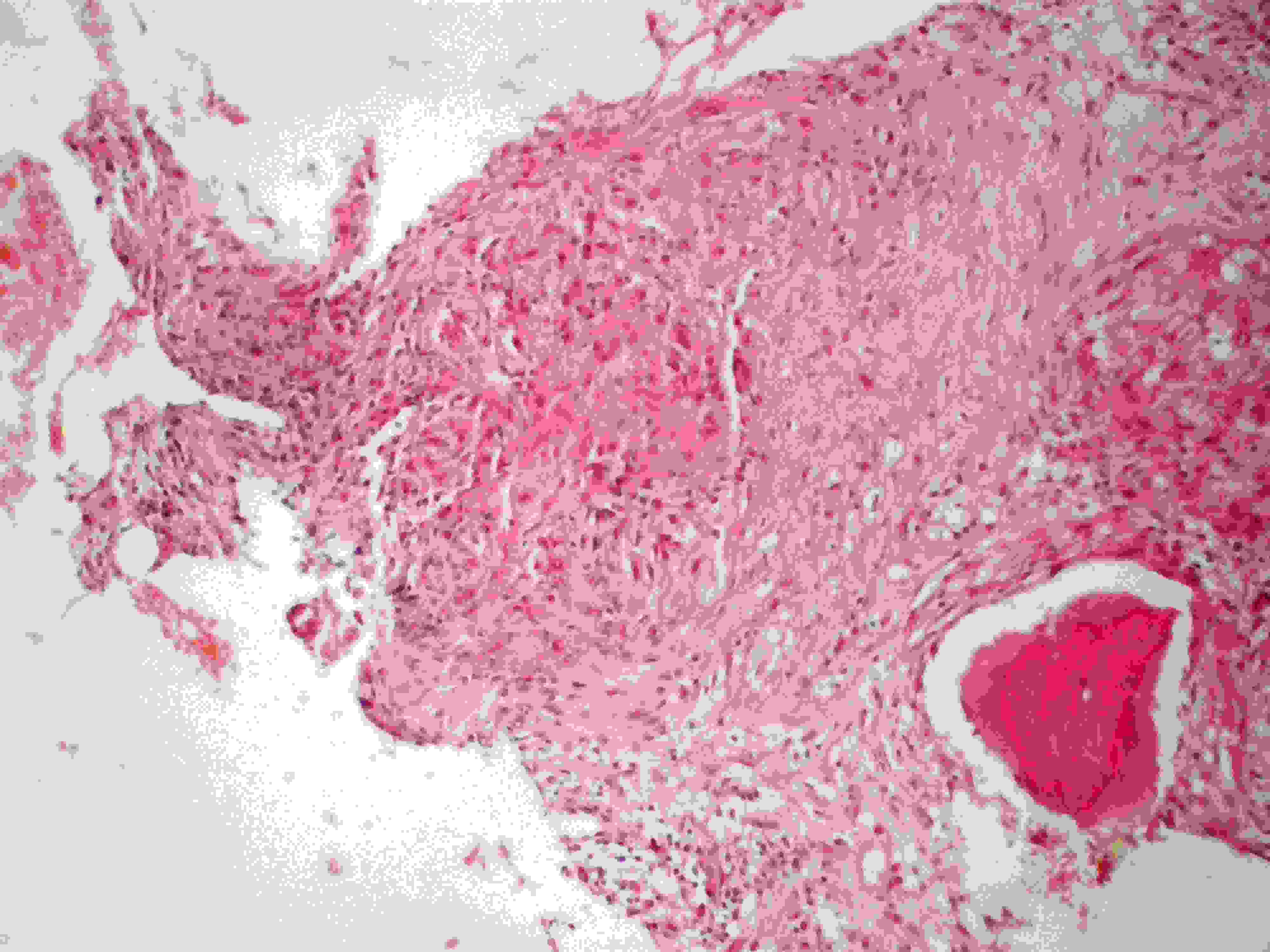
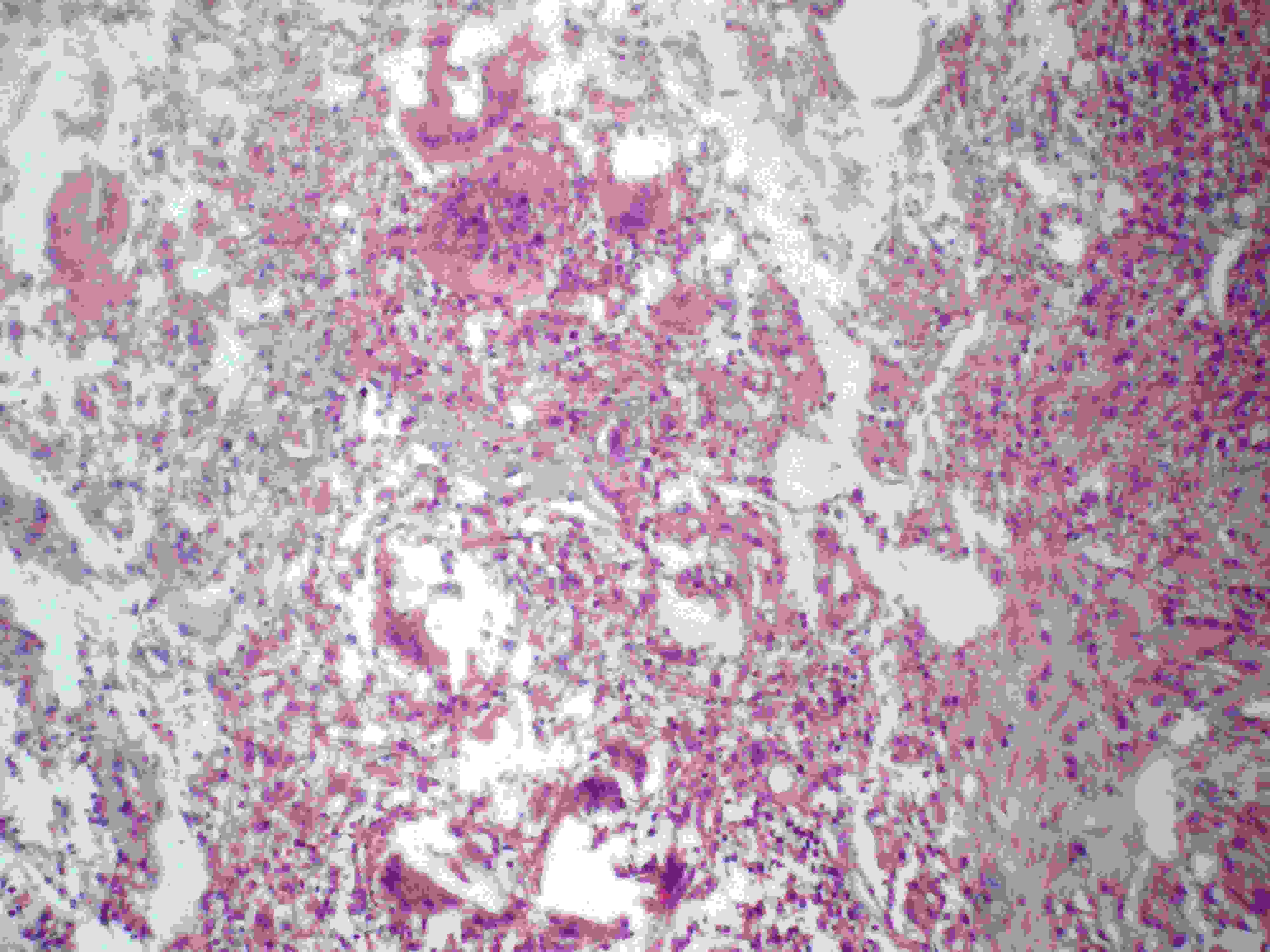
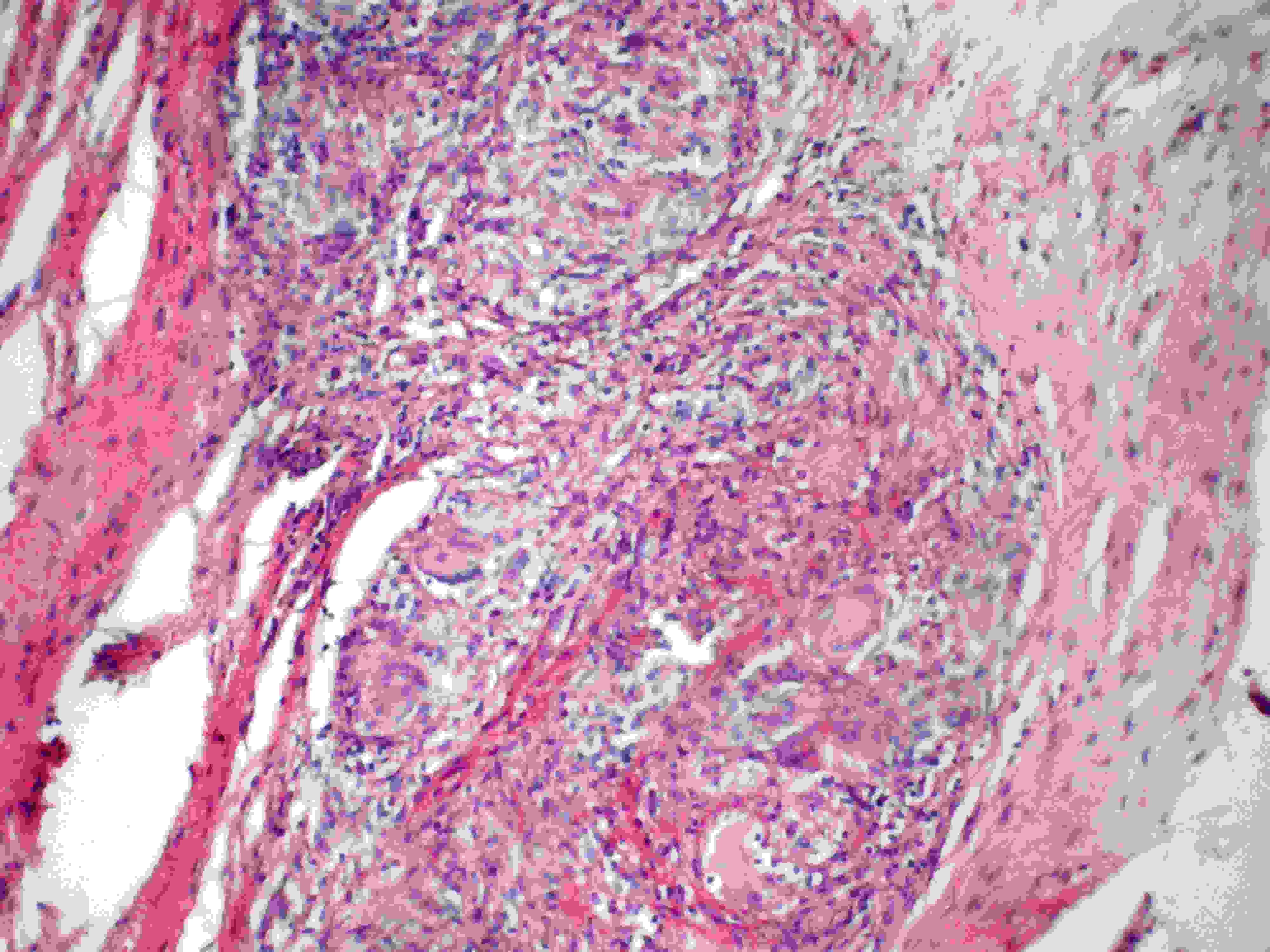
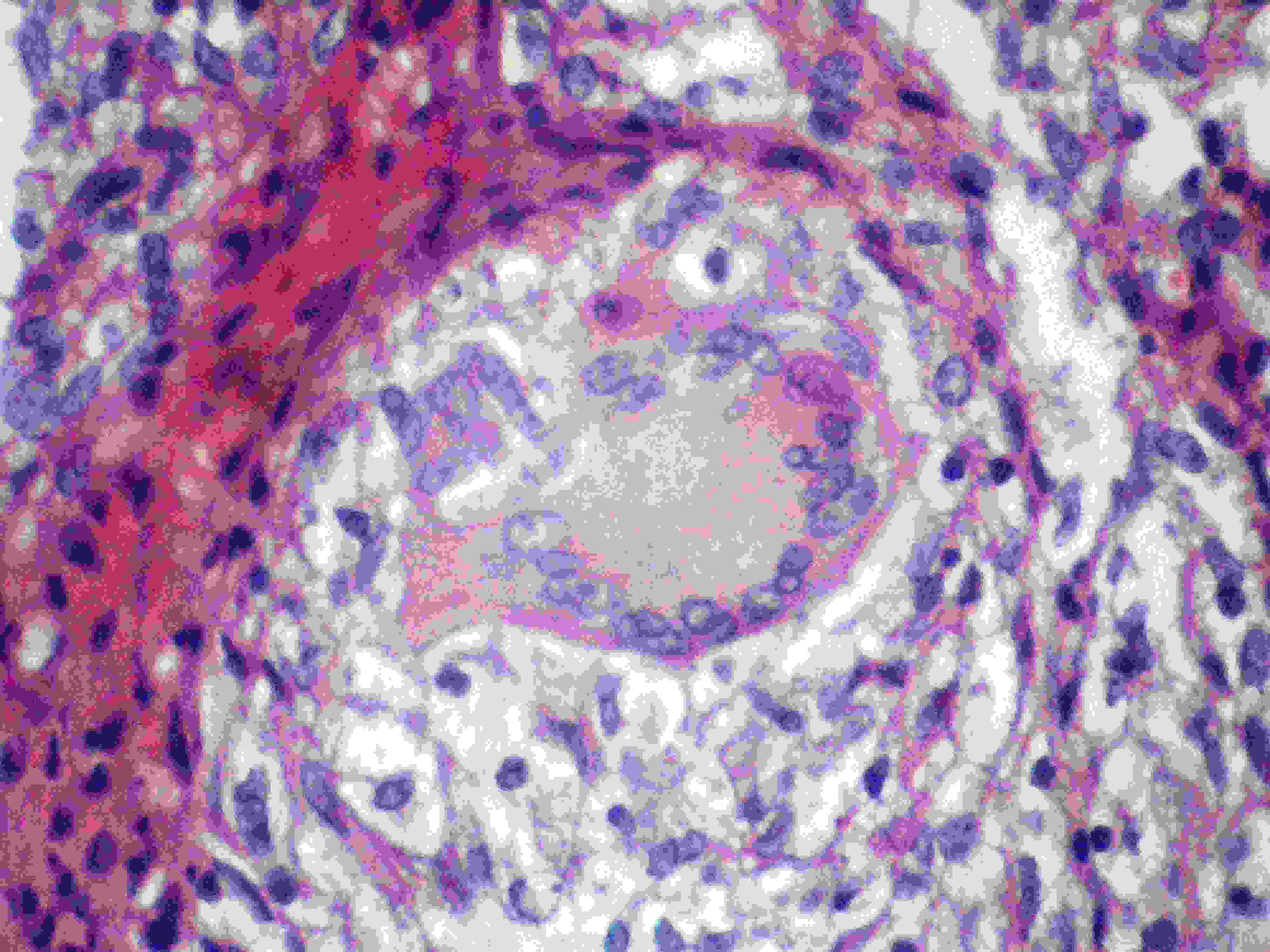
In 4 cases, smear of purulent or debrided material was studied and 3 were AFB positive. This study revealed clear prevalence of osteoarticular TB in lower limbs (68.75% of cases).The commonest site was knee joint (7cases), followed by spine and ankle (3 cases each) [Table/Fig-3]. The diagnosis was established based on biopsy findings. All the cases showed typical epithelioid cell granuloma, which was necrotising in 11 cases and giant cells were present in 13 cases [Table/Fig-4,5,6–7]. Ziehl-Neelsen stain for acid fast bacilli was done and found positive in 4 (25%) cases, one case was negative for AFB but was strongly Mantoux positive. PAS stain was done to rule out any fungal etiology of granuloma formation and was negative in all cases.
Distribution according to site of lesion
| S. No. | Site | No. of cases | Percentage (%) |
|---|
| 1 | Knee | 7 | 43.75 |
| 2 | Spine | 3 | 18.75 |
| 3 | Ankle | 3 | 18.75 |
| 4 | Metatarsus | 1 | 6.25 |
| 5 | Elbow | 1 | 6.25 |
| 6 | Wrist | 1 | 6.25 |
| Total | | 16 | 100 |
Photomicrograph of tuberculous osteomyelitis showing fairly well defined epithelioid granulomas with a small piece of bone (x100, H&E)
Photomicrograph showing ill defined granulomas with numerous giant cells and small foci of necrosis (x100, H&E)
Well defined epithelioid granulomas with several giant cells in fibrocollagenous tissue (x100, H&E)
High power of a granulomas showing Langhan’s giant cell (x400 H&E)
With the above histopathological picture, considering the clinical scenario, unavailability of latest technology like PCR at this centre, poor socio economic status of the patients and most important, in the view of high prevalence of tuberculosis in this district and adjacent area, a diagnosis of osteoarticular tuberculosis was rendered [Table/Fig-8] Type of osteoarticular involvement).
Patterns of Osteoarticular TB in the study
| Joint Involvement (Arthritis) * | 8 |
|---|
| Osteomyelitis | 2 |
| Both bone and joint | 1 |
| Spondylodiscitis (Spinal) † | 3 |
| Cold abscess ‡ | 1 |
| Sinus | 1 |
| Total | 16 |
* Includes one case of both ankle joint and tendinous involvement.
† One of the spinal cases presented with cold abscess.
‡ Possibly from tibial osteomyelitic lesion; X-ray showed lytic lesion in upper end of left tibia
ATT was started in 12 cases, and 4 cases were lost to followup after surgery. All, except one of the12 patients had regular treatment and follow up. All the cases have responded well to standard combination antitubercular therapy (ATT). 3 cases were still on therapy with good response.
Discussion
Osteoarticular/ skeletal tuberculosis as a form of extra pulmonary TB forms 1-4.3% of all TB cases [4–6] and 5-15% of all EPTB [2,6,7,8]. Yoon HJ et al., found out that BJTB formed the 3rd most common type of EPTB, after pleural and lymph node TB [12]. Similar findings were published in study of National and district level survey conducted under Revised National Tuberculosis Control Programme (RNTCP) in one year period in India. In this survey however lymph node involvement was the commonest, followed by pleural and bone and joint involvement. The bone and joint TB in that study at district level comprised 8.9% of cases [14]. Watts and Lifeso in their review found an increasing prevalence of TB in USA, both pulmonary and BJTB which is attributed to various factors [1]. Jutte et al., also found increasing prevalence of BJTB in Netherlands in recent years, mainly in non-Dutch subjects [6].
Studies in different countries (Romania, Spain, Israel and Korea) have found 19, 26, 38 and 41 cases respectively, over a span of 10 years [8,9,12,15]. However, in a study at a busy teaching institute in Thailand, 99 cases of osteoarticular TB were found from the electronic data base during a 2 year period, which appears to be a very significant number of cases [11]. In our study, 16 cases were found in 3 years’ duration. None of our patients gave past or family history of tuberculosis. Chest X-ray was not available in our cases.
BJTB is a secondary form of tuberculosis, most often due to seeding of marrow cavity occurring via haematogenous route [8]. History of pulmonary disease was available in 1/3rd of cases reviewed by Watts and Lifeso [1]. Jutte et al., found a concurrent pulmonary TB in 15% of cases [6] while a higher figure of 30.3% was found in Muangchan and Nilganuwong’s series [11].
Several studies and reviews have found a predominance of spinal involvement [1,2,6,11] most often thoracic spine with however, low or no spinal involvement in some other studies [8,9]. In our series spinal cases were not predominant and 2 of our 3 spinal cases were thoracic and 1showed lumbar involvement.
TB of joints is most often monoarticular [2,4]. 50% of our cases had tuberculous arthritis. Knee joint involvement was the most common in our series. TB osteomyelitis forms 3% of bone and joint tuberculosis [5]. In our series 2 cases of osteomyelitis and one case of osteomyelitis with arthritis was found. Apart from the common patterns of spondylodiscitis, arthritis and osteomyelitis, less common manifestation as tenosynovitis, bursitis and pyomyositis can be encountered [11].
In general, EPTB is more common in children [1]. Enache et al.,’s 10 years’ case review found that 2/3rds of patients were older than 40 years [8]. Much higher median age of 50 and 60 years has been noted in some studies [9,11]. In our study the average age was 23.6 years.
Watts and Lifeso mention, that in a community of high prevalence, most of the population has been infected by 20 years of age [1]. Spinal TB is more common in first 3 decades of life [5,7].
A female predominance is noted in some studies [6,11,12] while others have found osteoarticular TB to be more common in males [8,14]. In our study a slight male predominance was seen. Clinically, pain is the commonest symptom, as encountered in our series [11,15]. Local swelling and sinuses can be seen in some cases [2]; one of our cases showed multiple sinuses.
Monoarticular arthritis is common in case of joint tuberculosis [2,4]. ‘Night cries’ can be encountered in TB of hip and knee joints [14]. Neurological symptoms may be present in spinal TB [1] with Pott’s paraplegia being the most important complication and can be seen in 30% of cases [7]. 2 of our spinal cases had paraplegia. These can present as emergency in some cases [16]. A cold abscess is an important presentation in spinal TB and provides an important diagnostic clue [5]. Constitutional symptoms are not common [12].
Only one of our cases had fever. However all 15 cases of TB sacroliitis described by Ramlakan and Govender had constitutional symptoms [17]. Wares et al., mention that in spinal cases, constitutional symptoms commonly precede local symptoms. X-ray features have been found to be non-specific [1,13]. A high index of clinical suspicion is necessary [2,13,15] and in the series by Enache et al., 26% were clinically suspected of BJTB [8]. Delay in diagnosis can occur, especially in Caucasian population [18]. A good 44% of cases in our study were suspected to be tuberculosis clinically. In the study by Jutte et al., in Netherlands, there was a mean delay in diagnosis of non-spinal BJTB by 35 weeks [6].
The diagnostic modalities are several and depend on prevalence of TB in the community, availability and affordability. Raised ESR has been observed [17,12,13], but it is neither specific nor reliable [1]. Mantoux has limited role in adults in high prevalence area but can be useful in children under 5 years [14]. Only one of our case, a 23 year old female had Mantoux positivity (20 mm). Yoon HJ et al., observe that diagnostic criteria for EPTB are limited and this prompted them to retrospectively analyse various forms of EPTB with reference to clinical patterns, diagnostic methods, underlying diseases and X-ray findings [12].
Purulent fluid/ synovial fluid can be examined for AFB. A direct smear of operative specimen can show positivity for AFB in as low as 27% of cases [2]. In our study 3 out of 4 cases (75%) were AFB positive. In general, EPTB tends to be paucibacillary [14]. Yoong HJ et al., divided their cases of EPTB into 3 categories-1.Confirmed TB-had positive culture 2. Suspected TB- had positive smear/ chronic granulomatous inflammation 3. Possible TB-favourable radiological and clinical response to Rx [12]. However, an ideal work up may not be possible under all circumstances. Wares et al., opine that attempts should be made to confirm by histopathologic examination and /or bacterial examination [14]. Culture is considered to be gold standard. The material could be a biopsy specimen, cold abscess or sinus tract specimen [2,5]. Low percentage of culture positivity has been found by Yoong HJ et al., (11.2% of all EPTB) and by Muangchan and Nilganuwong (19.2 % for osteoarticular TB) [12,11]. However, review article by Haider et al., found 63% positivity [2].The drawback of conventional culture technique is that it is time consuming. Mycobacterial culture was not done in our patients.
Histologic picture forms one of the important diagnostic criteria [19]. Biopsy of bony lesion/ synovium/ soft tissue masses may be required to clear up diagnostic confusion [2]. Watts and Lifeso opine that in area of high prevalence with limited resources when clinical features and X-ray suggests TB, treatment can be started without biopsy. Further, they mention that failure to respond to chemotherapy, or in cases of substantial neurological impairment, or when resistant strains or other diseases are suspected, a biopsy is indicated [1]. In the series of 19 cases studied by Encahe et al., biopsy was diagnostic in 18 cases, which showed epithelioid granulomas and caseous necrosis. In 2 cases they resorted to PCR technique because of non-specific granulomatous response [8]. In the series by Muangchan and Nilganuwong diagnosis by biopsy was done in 46.5% of cases [11]. In the case of elbow joint TB reported by Sagoo et al., when initial steroid treatment did not bring complete relief, a synovial biopsy with debridement was done (along with smear, culture and PCR) [13].
An alternative to biopsy could be FNAC. In the 11 cases of FNAC of bone and soft tissues, granulomas, AFB on smear and a positive culture was seen in 73%, 64% and 83% of cases respectively [20].PCR technique can increase the sensitivity and help exclude non tuberculous mycobacterial infection of soft tissue [2]. However it is not widely available [7]. Titov et al., are of the opinion that combined PCR and biopsy is promising for diagnosis of TB arthritis [19].
Muangchan and Nilganuwong report that diagnosis in 33.3% of their cases was based on PCR [11]. Wares et al., are of the opinion that current diagnostic practices need to be evaluated with formulation of diagnostic algorithms. The authors are of the opinion that Medical colleges can play an important role by offering the diagnostic services [14]. Early diagnosis of osteoarticular TB is important to prevent advanced destruction and suffering [4] especially important in spinal TB, as the outcome greatly depends on early diagnosis [14]. A strong suspicion is important for diagnosis [12].
Multidrug ATT is the cornerstone of treatment [2,7]. Operative procedures are adjunct to ATT [1]. Treatment results are good with low morbidity and mortality [18]. Even in the advanced cases, good response can be seen [4]. However in Munagchan and Nilganuwong’s study, though improvement was noted, they were associated with residual deformities [11].
All the cases started on ATT (total 12 cases) in this study, showed good response, barring one patient who was lost to follow up. The remaining 4 patients did not come for further management after the biopsy. Treatment of BJTB which is a major public health problem is possible if it is recognised early and pre requisite for recognition is that a diagnostic possibility be considered [1].
Conclusion
Osteoarticular TB is one of the important forms of extra pulmonary TB and having significant consequence if not recognised and treated early on. Involvement of weight bearing joints and spine is common. In high prevalence areas, young adults are more commonly affected. A history of pulmonary TB is not obtained in a significant number of cases. A high degree of clinical suspicion along with the radiological, microbiologic and biopsy findings are important for diagnosis and starting ATT which is the main stay of treatment.
* Includes one case of both ankle joint and tendinous involvement.
† One of the spinal cases presented with cold abscess.
‡ Possibly from tibial osteomyelitic lesion; X-ray showed lytic lesion in upper end of left tibia