Embryonal Rhabdomyosarcoma Occurring on Mandibular Gingiva in an Adult
Gururaj Patil1, Sangamesh Halawar2, Shitalkumar Sagari3, Roopa Babannavar4, Sharad Purohit5
1 Reader, Jodhpur Dental College General Hospital, Jodhpur National University, Jodhpur, Rajasthan, India.
2 Reader, Department of oral Pathology & Microbiology, VPDC dental college & hospital, Sangli, Maharashtra, India.
3 Senior Lecturer, Jodhpur Dental College General Hospital, Jodhpur National University, Jodhpur, Rajasthan, India.
4 Senior Lecturer, Jodhpur Dental College General Hospital, Jodhpur National University, Jodhpur, Rajasthan, India.
5 Senior Lecturer, Jodhpur Dental College General Hospital, Jodhpur National University, Jodhpur, Rajasthan, India.
NAME, ADDRESS, E-MAIL ID OF THE CORESPONDING AUTHOR: Dr. Roopa Babannavar, Senior Lecturer, Department of Conservative & Endodontics, Jodhpur Dental College General Hospital, Jodhpur National University, Jodhpur, Rajasthan-342001, India.
Phone: 07597216316,
E-mail: rbabannavar84@gmail.com
An embryonal rhabdomyosarcoma (ERMS) is a primitive, malignant, soft tissue sarcoma that recapitulates the phenotypic and biological features of embryonic skeletal muscles. Occurrence of intraoral ERMS in adults is extremely rare. This unique case report highlights the clinical, radiographic, histopathological and immunohistochemical findings of an intraoral ERMS.
Rhabdomyosarcoma, Embryonal rhabdomyosarcoma, Oral, Head and neck
Introduction
Rhabdomyosarcoma (RMS) was first described by Weber in 1854. It was sub-classified by Horn and Enterline into embryonal, alveolar, botryoid, and pleomorphic sub-types [1,2]. ERMS is a primitive, malignant, soft tissue sarcoma that recapitulates the phenotypic and biological features of embryonic skeletal muscles [3]. 28% of RMSs occur in head and neck, and amongst them, 0.04% occur as intra–oral tumours [4,5]. Its occurrence in children is common, but in adults, it is extremely rare [2,5]. This case report emphasises the indifferent presentation of an intra–oral ERMS on mandibular gingiva, with clinical, radiographical, histopathological and immunohistochemical findings.
Case Report
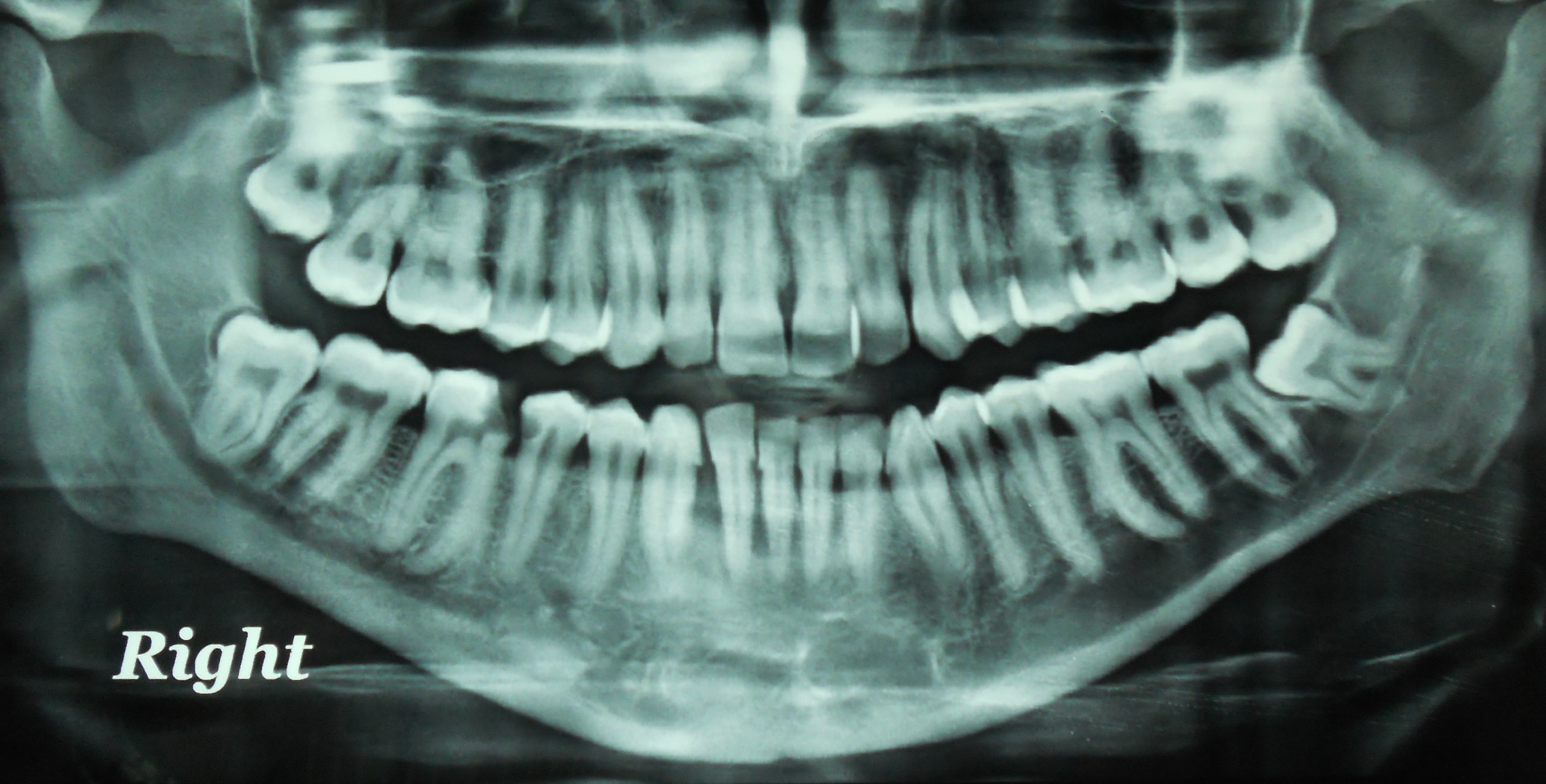
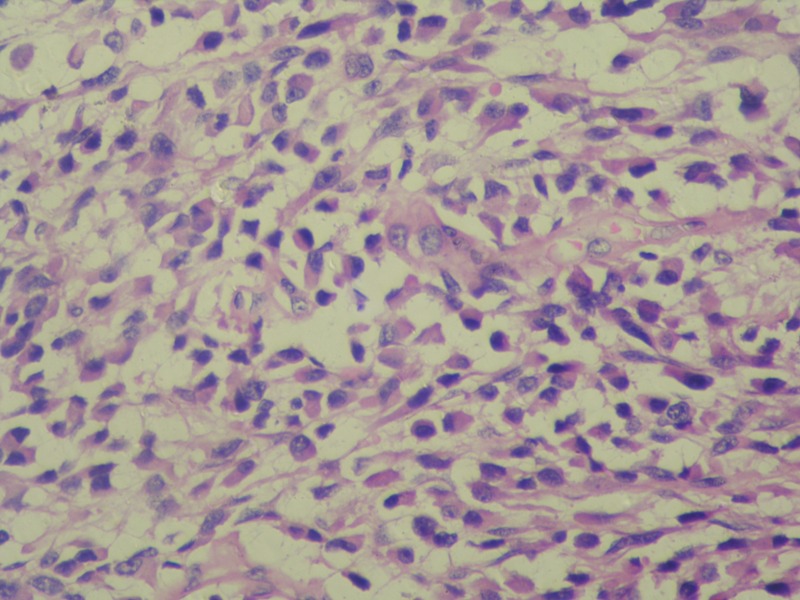
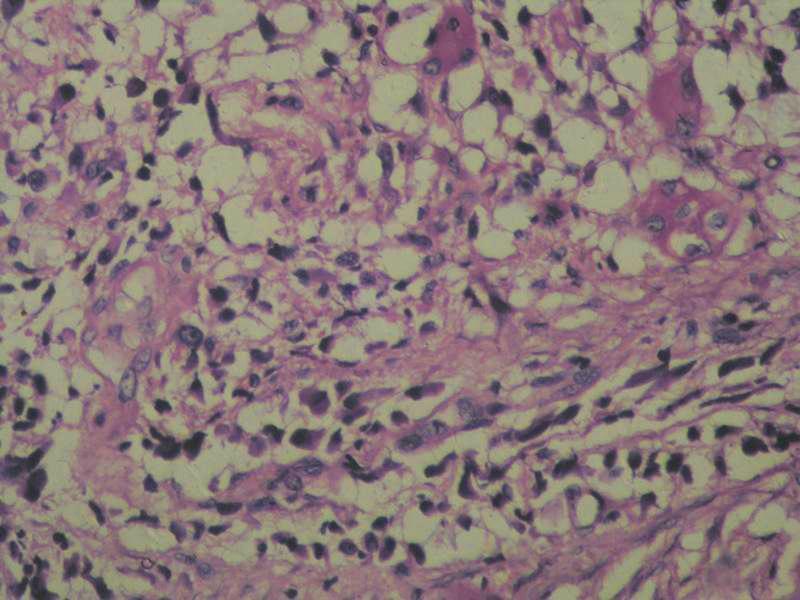
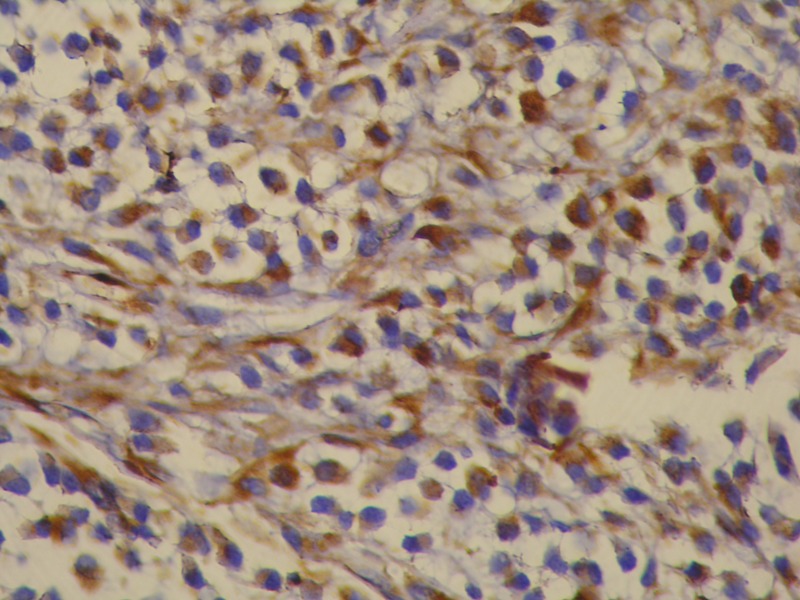
A 34-year-old, male reported with a painless nodule in the lower right, front gingiva. Patient reported a progressive growth of the nodule since past six months. On intraoral examination, a swelling with a lobulated surface, which measured 3 cm × 4 cm, was located on mandibular gingiva. Swelling extended from right central incisor to right first premolar and it had a sessile base [Table/Fig-1]. Radiographic examination showed a superficial erosion of the labial cortical plate [Table/Fig-2]. A clinical differential diagnosis of a peripheral ossifying fibroma and a peripheral giant cell granuloma or a healing pyogenic granuloma was considered. After taking informed consent of the patient, an incisional biopsy was performed. Histopathological sections showed prominent primitive cells with amphophilic cytoplasm and central angulated or oval nuclei. Few stellate cells were seen as well [Table/Fig-3]. Presence of tadpole shaped, strap and spider cells was also evident [Table/Fig-4]. An immunohistochemical analysis was done. Vimentin [Table/Fig-5] was strongly positive, with limited expression for desmin and myoglobin. Patient was treated by hemi- mandibulectomy, followed by radiotherapy. The patient is under follow up since two years, with absence of recurrence.
Lobulated swelling on gingiva

Orthopantomograph showing superficial erosion labial cortical plate
Premitive cells with light ampophilic cytoplasm with oval and angulated nuclei
Tadpole shaped, strap and spider cell
Immunohistochemical expression for vimentine
Discussion
A recent PubMed search for intra–oral RMSs showed only 25 cases reports which have been published in English language literature. The most commonly affected areas are the head and neck region, genitourinary tract and retroperitonium. The head and neck RMSs are anatomically divided into 2 categories: Para meningeal and nonparameningeal [1]. 60% of RMSs are of embryonal subtype [2,3,6]. Though they are most common in children, the average age of occurrence is 7.5 years, with a slightly male predilection [5]. Our patient was older than this average age. Previously reported cases had presented with signs of malignancy [5,6], but present case did not have any such signs, except for a superficial erosion of cortical plate. The histologic architecture of ERMS resembles embryonic muscle differentiation stages, which form aggregates of myoblast and, stellate cells with lightly amphophilic cytoplasm and central oval nuclei [1,2,6]. Thus, only vimentin is present in the cytoplasm of the most primitive cells, and desmin and actin are acquired by developing rhabdomyoblasts. Differentiated cells exhibit myoglobin; myosin, and creatine kinase M, markers which correspond to terminal differentiation [1,4,6]. The present case showed strong positive staining for vimentin and variable staining for desmin and myoglobin. Histological and immunohistochemical features were similar to others’ findings.
Conclusion
Dental practitioners frequently encounter cases of RMSs or ERMSs in children; however, the occurrence a painless swelling in adults is extremely rare and it can pose a diagnostic challenge. This kind of presentation of the lesion, with superficial erosion of cortical plate as only sign of malignancy as, can lead to a misdiagnosis of common benign swellings. This can lead to a delay in diagnosis and treatment. Initial management is critical for a better prognosis of any disease.
[1]. Miloglu O, Altas SS, Buyukkurt MC, Erdemci B, Altun O, Rhabdomyosarcoma of the oral cavity: a case reportEur J Dent 2011 Jul 5(3):340-3. [Google Scholar]
[2]. França CM, Caran EM, Alves MT, Barreto AD, Lopes NN, Rhabdomyosarcoma of the oral tissues two new cases and literature reviewMed Oral Patol Oral Cir Bucal 2006 Mar 1 11(2):E136-40. [Google Scholar]
[3]. Parham D.M., Barr F.G., Pathology and Genetics of Tumours of Soft Tissue and Bone 2002 LyonIARC Press:146-49. [Google Scholar]
[4]. Simon JH, Paulino AC, Ritchie JM, Mayr NA, Buatti JM, Presentation, prognostic factors and patterns of failure in adult rhabdomyosarcomaSarcoma 2003 7(1):1-7. [Google Scholar]
[5]. Chi AC, Barnes JD, Budnick S, Agresta SV, Neville B, Rhabdomyosarcoma of the maxillary gingivaJ Periodontal 2007 Sep 78(9):1839-45. [Google Scholar]
[6]. Gordón-Núñez MA, Piva MR, Dos Anjos ED, Freitas RA, Orofacial rhabdomyosarcoma: report of a case and review of the literatureMed Oral Patol Oral Cir Bucal 2008 Dec 1 13(12):E765-9. [Google Scholar]