Peripheral Ossifying Fibroma Secondary to Pulpo-Periodontal Irritation
Francis Akkara1, Paul Chalakkal2, Chandra Mohan Boyapati3, Rajdeep Pavaskar4
1 Assistant Professor, Department of Oral and Maxillofacial Surgery, Goa Dental College and Hospital, Bambolim-403202, Goa, India.
2 Lecturer, Department of Pedodontics and Preventive Dentistry, Goa Dental College and Hospital, Bambolim-403202, Goa, India.
3 Reader, Department of Coservative Dentistry and Endodontics, Index Institute of Dental Sciences, Indore-452001, Madhya Pradesh, India.
4 Senior Lecturer, Department of Conservative Dentistry and Endodontics, Index Institute of Dental Sciences, Indore-452001, Madhya Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Francis Akkara, Assistant Professor, Department of Oral and Maxillofacial Surgery, Goa Dental College and Hospital, Bambolim – 403202, Goa, India.
Phone: 9823150952,
E-mail: marcfrancis24@yahoo.com
This report has discussed the endodontic and surgical management of a peripheral ossifying fibroma that had occurred in the anterior maxillary anterior region, between a central and a lateral incisor in a 12-year-old child. The lesion was diagnosed to have occurred secondary to a pulpo-periodontal irritation.
Peripheral, Ossifying, Fibroma, Pulpo-periodontal
Case Report
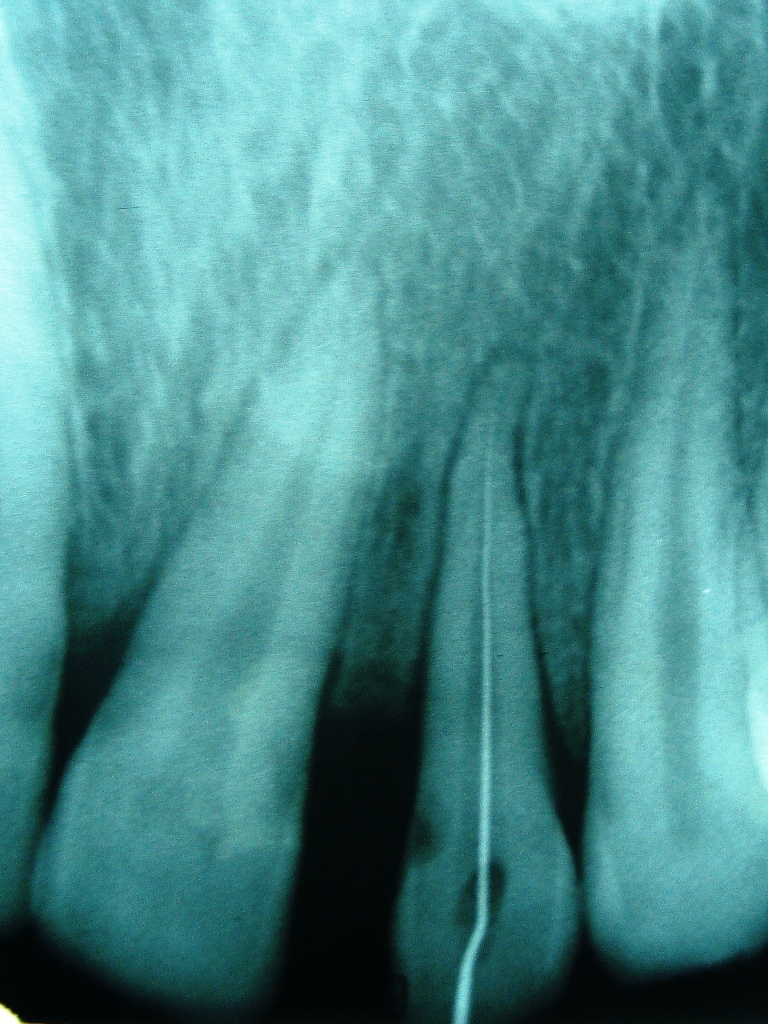
A 12-year-old boy visited the Department of Oral and Maxillofacial Surgery with the complaint of a soft tissue mass in the anterior maxilla, which had progressively enlarged over a period of six months. On examination, the mass was found to be well-circumscribed, sessile, erythematous, firm and painless, which measured 1.5 cm in diameter, spanning from the labial gingiva across to the palatal side, in relation to 21 and 22 [Table/Fig-1 and 2]. The lesion was asymptomatic, non-ulcerated and similar in colour to the adjacent gingiva. 22 appeared to have distalized in relation to 21, resulting in a spacing between the two. There was no evidence of dental caries or crown fractures in relation to 21 and 22. A periapical radiograph revealed alveolar crestal bone loss between 21 and 22, and a radiolucency on the mesioproximal aspect of 22 [Table/Fig-3]. The radiolucency had a pulpal connection, which was suggestive of sub–gingival caries. There was widening of the periodontal space in relation to 22, and the tooth was tender to percussion.



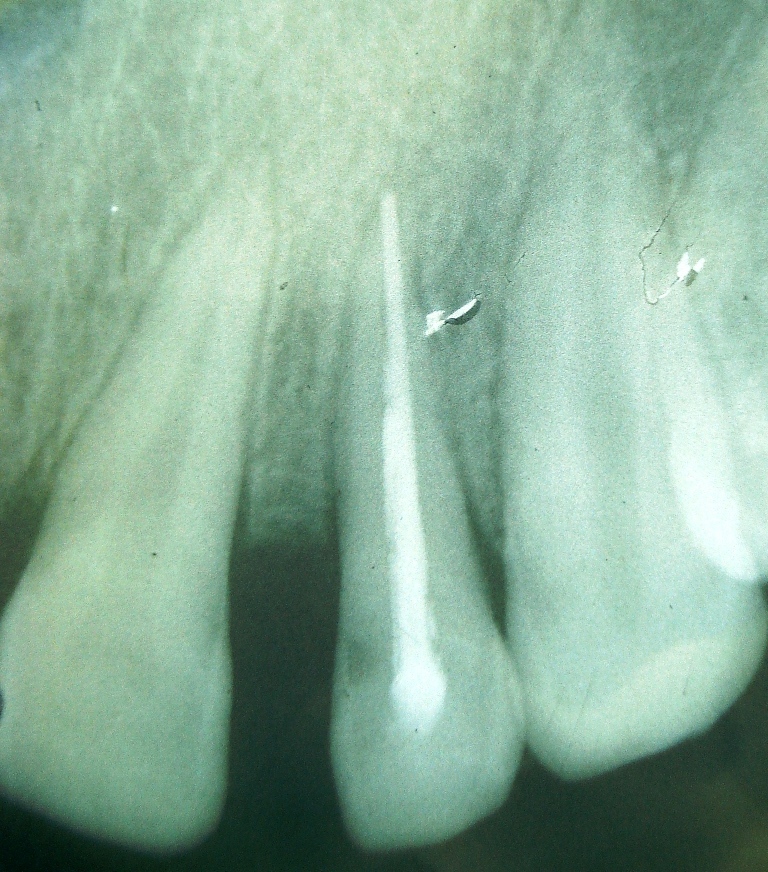
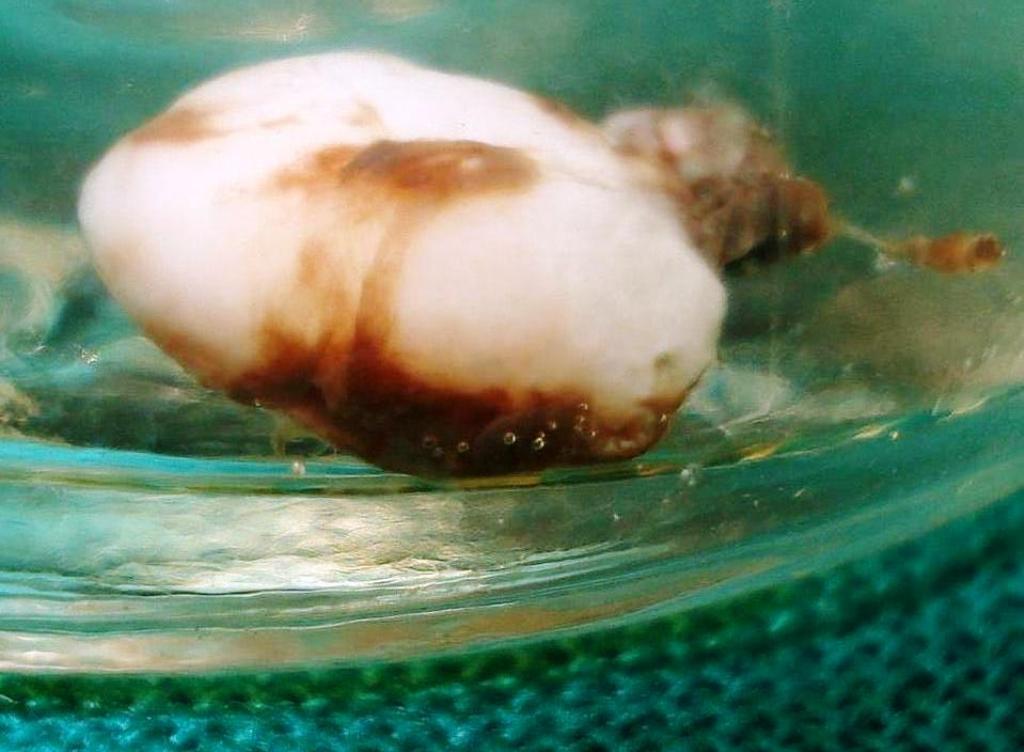
Conventional root canal therapy and obturation with gutta-percha were performed for 22 [Table/Fig-4 and 5]. The lesion was excised along with the underlying periosteum, followed by curettage, and a periodontal pack (zinc oxide based) was placed [Table/Fig-6 and 7]. The specimen was preserved in 10 % formalin and it was sent for a histopathological evaluation [Table/Fig-8].
Working length determination for 22 mm

After placement of periodontal pack

Specimen in 10 % formalin
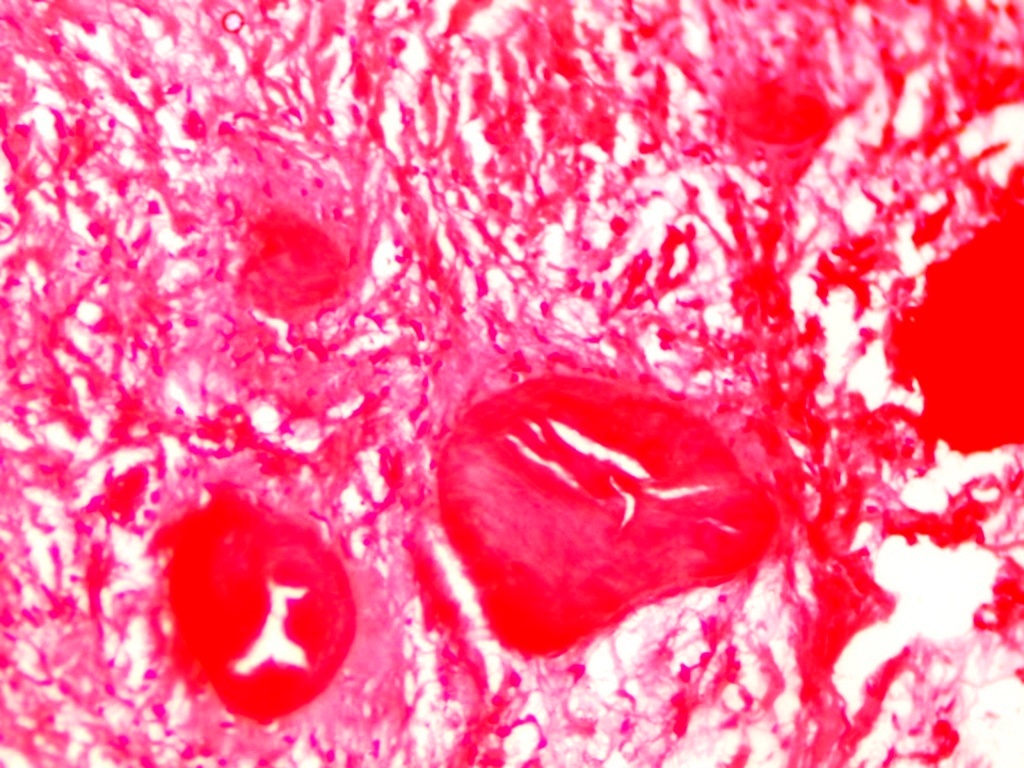
Microscopic evaluation revealed a cellular fibrous connective tissue stroma which contained calcified osseous structures which were covered by a stratified squamous epithelium. The calcified osseous structures resembled trabecular bone. Some areas in the connective tissue showed inflammatory cell infiltrates [Table/Fig-9]. The above features helped us in concluding that it was a case of a peripheral ossifying fibroma.
Bony trabeculae within fibrous connective tissue stroma (H-E staining X 150)
Discussion
A peripheral ossifying fibroma may be defined as a gingival nodule which is composed of a cellular fibroblastic connective tissue stroma which is associated with the formation of randomly dispersed foci of mineralised products, which consists of bone, cementum-like tissue, or a dystrophic calcification [1]. It accounts for 9.6% of all gingival lesions [2]. It has a higher predilection for females; it rarely occurs in the first decade of life; and declines in incidence after 30 years; these are indicative of a possible hormonal influence [3,4]. Its occurrence is found to be more in whites (71%) than in blacks (36%) [5]. In most of the cases, the lesion affects the maxilla (60%), more often in the anterior region.
It has been suggested that a peripheral ossifying fibroma originates from the cells of the periodontal ligament, because, it exclusively occurs in gingival tissues which are close to the periodontal ligaments; oxytalin fibres are often found within the mineralized matrix of the lesion; the age distribution of its occurrence is inversely proportional to the number of permanent teeth which are lost; and the fibrocellular response of a peripheral ossifying fibroma is similar to that of other reactive gingival lesions which originate from the periodontal ligament [6,7].
A peripheral ossifying fibroma may closely resemble a pregnancy tumour, epulis fibrosa, inflammatory hyperplasia, a peripheral giant cell granuloma or a central giant cell granuloma [8]. Excessive proliferation of fibrous connective tissue can occur in response to a gingival injury, gingival irritation, a subgingival calculus or the presence of a foreign body in the gingival sulcus. Chronic irritation of the periosteal and periodontal membranes may cause metaplasia of the connective tissue, resulting in a dystrophic calcification.
In this case, the patient’s lesion could be attributed to the abundant calculus and plaque that were present on adjacent teeth and/or the sub–gingival carious lesion in relation to 22. 22 was affected both endodontically and periodontically, as was evidenced on the radiograph. These might have resulted in chronic gingival irritation, resulting in growth of the lesion. Erosion of alveolar bone and tooth separation in relation to the lesion have also been previously reported [5].
Post operatively, meticulous oral prophylaxis was performed for the patient, that included supra-gingival and sub-gingival ultrasonic scaling and polishing. Oral hygiene maintenance instructions were also given. A recurrence rate of 20% has been reported, mainly due to incomplete removal of the lesion and/or persistence of aetiological factors [9]. However, there has not been any recurrence of the lesion, two years post operatively.
Conclusion
Based on clinical, radiological and microscopic evaluations, the lesion was concluded to be a peripheral ossifying fibroma which had arisen due to irritation from a subgingival caries lesion, calculus and plaque, in relation to the maxillary lateral incisor.
[1]. Neville BW, Damm DD, Allen CM, Bouquot JE, Oral and maxillofacial pathology 1995 PhiladelphiaW.B. Saunders:374-6. [Google Scholar]
[2]. Walters JD, Will JK, Hatfield RD, Cacchillo DA, Raabe DA, Excision and repair of the peripheral ossifying fibroma: a report of 3 casesJ Periodontol 2001 72:939-44. [Google Scholar]
[3]. Kenney JN, Kaugars GE, Abbey LM, Comparison between the peripheral ossifying fibroma and peripheral odontogenic fibromaJ oral Maxillofac Surg 1989 47:378-82. [Google Scholar]
[4]. Miller CS, Henry RG, Damm DD, Proliferative mass found in the gingivalJ Am Dent Assoc 1990 121:559-60. [Google Scholar]
[5]. Cuisia ZES, Brannon RB, Peripheral ossifying fibroma – a clinical evaluation of 134 pediatric casesPediatr Dent 2001 23:245-8. [Google Scholar]
[6]. Ono A, Tsukamoto G, Nagatsuka H, Yoshihama Y, Rivera RS, Katsuramo M, An immonohistochemical evaluation of BMP-2,4, osteopontin, osteocalcin and PCNA between ossifying fibromas of the jaws and peripheral cemento-ossifying fibromas on the gingivalOral Oncol 2007 43:339-44. [Google Scholar]
[7]. Kumar SK, Ram S, Jorgensen MG, Shuler CF, Sedghizadeh PP, Multicentric peripheral ossifying fibromaJ Oral Sci 2006 48:239-43. [Google Scholar]
[8]. Orkin DA, Aimadas VD, Ossifying fibrous epulisOral Surg Oral med Oral Pathol 1984 57:147-8. [Google Scholar]
[9]. Eversole LR, Rovin S, Reactive lesions of the gingivaJ Oral Pathol 1972 1:30-8. [Google Scholar]