Osteoporosis is defined as “a disease which is characterised by low bone-mass and micro-architectural deterioration of bone tissue, which leads to enhanced bone fragility and a consequent increase in fracture risk [1].” Besides a natural reduction in Bone Mineral Density with age, the National Osteoporosis Foundation has identified many risk factors and predisposing factors for osteoporosis and related fractures in post-menopausal women. Some of the important factors are: a personal history of fractures in adulthood, a history of fragility in a first degree relative, low body weight, poor health, low calcium intake, gastrectomy, and use of oral glucocorticoid therapy for more than 3 months. The financial cost of treating osteoporosis–related injuries is extremely high and hence, it is considered as an increasing health burden for both developed and developing countries. The prevalence of vertebral fractures increases rapidly after the age of 65 years in women. Vertebral fractures are the most common complications of osteoporosis; however, they are frequently asymptomatic and they go undetected [2]. Therefore, health promotion strategies should focus on identifying subjects with a high risk of fractures and preventing osteoporosis-related mortality and morbidity as early as possible.
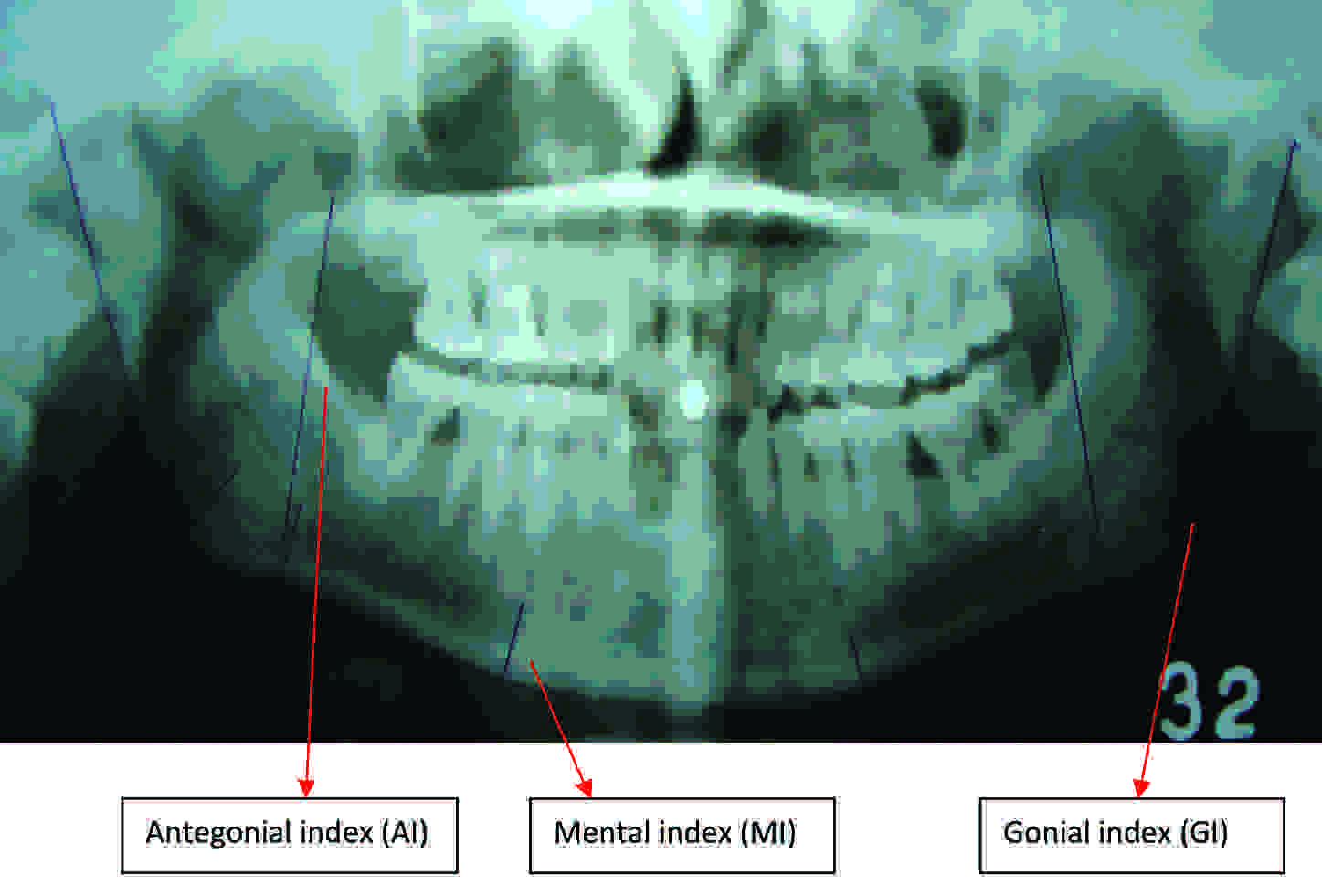
WHO has proposed bone mineral density (BMD) measurements to establish the diagnosis of osteoporosis. DEXA has been recognized as the best available technique for in vivo bone measurement. DEXA can measure BMD at the coxa or spine, but it can also be used to measure the total amount of mineral in the whole skeletal or cubitus [1]. To detect early signs of osteoporosis, it is ideal to perform Bone Mineral Density (BMD) testing of all post-menopausal women who are at risk. Dual energy absorptiometry (DEXA) has been recognized as the best available technique for in vivo bone measurement [3]. But DEXA is an expensive technique and therefore, a less expensive alternate should be agreed upon, to assess the skeletal status in post-menopausal women, especially those who are from low socio-economic strata, which comprise a significant percentage of post-menopausal women in India. Panoramic radiography has been an important component of dental diagnostic radiology for over 40 years. Identifying women with low bone mineral density by using panoramic radiographs is a particular topic that has drawn the attention of researchers over the last decade [4]. Qualitative and quantitative indices which include the mandibular cortical index (MCI), mental index (MI), antegonial index (AI), gonial index (GI) or panoramic mandibular index (PMI) have been used for panoramic radiographs, to assess the bone quality and to observe signs of resorption and osteoporosis [4].
In order to study the strength of correlation between the above mentioned panoramic mandibular indices and BMD results by using DEXA method, we designed a study on post menopausal population of different age groups in Central India, with the following objectives. (i) To assess and compare the relative efficacy, ease of application and measurement of the various mandibular cortical indices which were obtained on panoramic radiographs with bone densitometry data of post-menopausal women and (ii) to evaluate the effectiveness of these measurements in the identification of cases of osteoporosis/osteopaenia.
Material and Methods
A cross sectional study was conducted on 40 post menopausal women who were aged between 40 to 69 years (mean age- 53.50 ± 7.5). The study subjects were randomly selected among those who reported to the Department of Oral Medicine, Diagnosis and Radiology, at Modern Dental College and Research Centre, Indore, M.P, India, from June 8th to Dec 10th 2010. Permission was obtained from the ethical committee of the dental institute before initiation of the study. Written informed consents were obtained from all the patients who participated in the study.
Patients who were in natural menopause (which was recognised to have occurred after 12 months of amenorrhoea and for which there was no obvious pathologic cause) with no history of oophorectomy or hysterectomy, were included in the study. Smokers and alcoholics, patients with any known systemic disease that would affect bone metabolism like hyperparathyroidism, hypoparathyroidism, hyperthyroidism, Paget’s disease, osteomalacia, renal osteodystrophy, cancers with bone metastasis or significant renal impairment and those who were on specific drugs (corticosteroids) which are known to have adverse effects on bone metabolism were excluded from the study.
Prior to the commencement of the study, the examiner was standardised and calibrated by a consultant in the Department of Oral Medicine, Diagnosis and Radiology, to ensure uniform interpretations, and consistent examinations (kappa value=1.00). A comprehensive recording of the case history (both medical and dental) was followed up with the oral examination. The patients were then subjected to panoramic imaging in the Department of Oral Medicine, Diagnosis and Radiology, Modern Dental College and Research Centre, Indore, on a conventional planmeca (Model: PM2002cc Proline), with exposure parameters being in the range of 65-70kVp and 8mA, by utilising Kodak T-Mat, speed E films. The radiographs were evaluated by a subjective determination of patient positioning, head alignment, film density, and contrast, which were within the reviewer’s standard range of quality. Linear and angular measurements were then traced manually by using vernier caliper, scale, protractor and marker pen. The structures of interest were traced on transparencies which were fixed on the radiographs by using the radiographic viewer.
Thereafter, Dual–energy X–ray absorptiometry (DEXA) scan of the left femoral and AP spine (L1–L4) was performed by using a Lunar DEXA Machine at Sodani’s Diagnostic and Imaging Center, Indore. This procedure is the current gold standard for measuring bone mass and detecting osteoporosis [5].
The results of DEXA scan were then compared with the results of the indices which were traced on the panoramic radiographs. Each subject was allocated an identification number and, in order to avoid bias in the measurements, radiographs were measured in a random order, so that the observer was blind to the subject’s details. All the radiographs were reanalysed by the same observer after a two week interval. The mean cortical width on both sides of the mandible was used in this study.
The following radiomorphometric indices were measured on each radiograph [Table/Fig-1]:
Mental Index (MI): Mandibular cortical thickness was measured on the line which was perpendicular to the bottom of the mandible at the middle of the mental foramen [6].
Panoramic Mandibular Index (PMI): The PMI is the ratio of the thickness of the mandibular cortex to the distance between the mental foramen and the inferior mandibular cortex [1].
Gonion Index (GI): Mandibular cortical thickness was measured on the bisectrix of the angle, between the tangent lines of the posterior border of the branch and the bottom of the mandible [7].
Antegonial Index (AI): AI was a measurement of cortical width in the region which is anterior to the gonion, at a point which is identified by extending a line of `best fit’ on the anterior border of the ascending ramus, down to the lower border of the mandible. Where the anterior border of the ramus was markedly curved, the line was drawn to fit as closely as possible, to the straighter, inferior, part of the bone margin which was above the third molar region [8].
Mandibular Cortical Index (MCI): According to the classification of Klemetti et al., [9], MCI is the appearance of the inferior mandibular cortical thickness, which is as follows:
C1: The endosteal margin of the cortex is even and sharp on both sides;
C2: The endosteal margin shows semilunar defects (lacunar resorption) or it seems to form endosteal cortical residues (one to three layers) on one or both sides;
C3: The cortical layer forms heavy endosteal residues and it is clearly porous.
Tracing on OPG showing all the indices recorded
WHO proposed to define osteoporosis on the basis of the T-score [which is the difference between the measured BMD and the mean value of young adults, which is expressed in standard deviations (SD) for a normal population of the same gender and ethnicity]. The WHO diagnostic criteria for osteoporosis defines osteoporosis in terms of a T-score which is below -2.5 and osteopaenia in terms of a T-score which is is between -2.5 and -1 [10].
Statistical Analysis
The recorded data was compiled and entered into a spreadsheet computer program (Microsoft Excel 2007) and it was then exported to a data editor of SPSS, version 18.0 (SPSS Inc., Chicago, Illinois, USA). The patients were classified according to the indices for a later comparison with the bone densitometry results, based on WHO criteria. The data were expressed as mean and standard deviation (SD). Analysis of variance (ANOVA) with post–hoc Tukey’s test was performed to determine group differences in mandibular measurements. Weighted kappa statistics were used to evaluate inter and intra observer agreements. Calculation of sensitivity and specificity of indices which were utilised for detection of bone mass loss was based on the classification of patients into normal or those with bone mass loss, according to the bone densitometry results.
Results
The number of subjects in the age group of 40 – 49 years was 13 (32.5%), in the 50 – 59 years age group, it was 14 (35%) and in the 60-69 years age group , it was 13 (32.5%). A majority were in the osteoporotic (40%) group, followed by osteopaenic (37.5%) and normal (22.5%) groups. Chi–Square test was used to test the difference in ages in the three groups according to the DEXA results. The difference was statistically not significant (p = 0.369) [Table/Fig-2].
Distribution of study population according to age and DEXA report
| Age groups | DEXA report | Total |
|---|
| Normal | Osteopenic | Osteoporotic |
|---|
| 40-49 | 3 (23.1) | 4 (30.8) | 6 (46.2) | 13 (32.5) |
| 50-59 | 3 (21.4) | 8 (57.1) | 3 (21.4) | 14 (35) |
| 60-69 | 3 (23.1) | 3 (23.1) | 7 (53.8) | 13 (32.5) |
| Total | 9 (22.5) | 15 (37.5) | 16 (40) | 40 (100) |
Chi Square value = 4.283; df = 4; p value = 0.369; Not significant
According to the DEXA report, the subjects who had normal bone mineral density were 9 (22.5%), 15 (37.5%) were osteopaenic and 16 (40%) were osteoporotic. The mean values showed significant reductions in the osteoporotic group as compared to normal and osteopaenic groups in all the radiomorphometric indices (Mental Index (p = 0.000); Panoramic Mandibular Index (p = 0.007) and Gonial Index (p = 0.000). This reduction was insignificant in the antegonial index group (p = 0.135) [Table/Fig-3]. According to the results of the post–hoc Tukey test, Mental index showed that both normal (p = 0.000) and osteopaenic (p = 0.038) DEXA groups had statistically significant differences when compared to osteoporotic DEXA group. Only normal DEXA group showed a statistically significant difference in the mean panoramic mandibular index (p = 0.005) as compared to osteoporotic DEXA group. Similarly gonial index also showed a statistically significant difference between the normal DEXA group and osteopaenic (p = 0.002) and osteoporotic (p = 0.000) DEXA groups.
Mean values of Mental, Panoramic Mandibular, Gonial and Antegonial indices according to DEXA results
| Groups according to DEXA | Mental Index | p value | Panoramic Mandibular Index | p value | Gonial Index | p value | Antegonial Index | p value |
|---|
| Mean | SD | Mean | SD | Mean | SD | Mean | SD |
|---|
| Normal (n=9) | 4.8389 | 0.67484a | 0.000* | 0.3722 | 0.05286a | 0.007* | 1.4311 | 0.26760a | 0.000* | 3.5778 | 0.81038 | 0.135 |
| Osteopenic (n=15) | 4.0507 | 0.85398a,b | 0.3053 | 0.05914a,b | 1.0120 | 0.27816b | 3.2053 | 0.78189 |
| Osteoporotic (n=16) | 3.2438 | 0.98934c | 0.2688 | 0.09280c,b | 0.9306 | 0.25365c,b | 2.9263 | 0.71696 |
Tests used: One way ANOVA, Post–hoc Tukey test
One way ANOVA: * indicates statistically significant difference at p ≤ 0.05.
Post–hoc Tukey test: Groups with same letter superscripted are not statistically significant.
The mean values showed a non significant reduction in the 60-69 years age group as compared to 40-49 years and 50-59 years age groups (Mental Index (p = 0.699); Panoramic Mandibular Index (p = 0.107), Gonial Index (p = 0.235) and Antegonial Index (p = 0.135) [Table/Fig-4]. The number of subjects with MCI- C1 was 8 (20%), that with C2 was 21 (52.5%) and that with C3 was 11 (27.5%). MCI was used a diagnostic criteria and it was compared with gold standard i.e. DEXA results. The true negatives were 8 and true positives were 31. The false positive was 1 and false negative was 0. Thus, the specificity was 88.88% and sensitivity was 100%. The negative predictive value was 100% and positive predictive value was 96.87% [Table/Fig-6].
Mean values of Mental, Panoramic Mandibular, Gonial and Antegonial indices according to age. Tests used: One way ANOVA.
| Age group in years | Mental Index | p value | Panoramic Mandibular Index | p value | Gonial Index | p value | Antegonial Index | p value |
|---|
| Mean | SD | Mean | SD | Mean | SD | Mean | SD |
|---|
| 40-49 (n=13) | 4.0715 | 1.2136 | 0.699 | 0.3400 | 0.08042 | 0.107 | 1.1177 | .32156 | 0.235 | 3.4800 | 0.71799 | 0.135 |
| 50-59 (n=14) | 3.9279 | 0.80166 | 0.3050 | 0.06584 | 1.1500 | .32074 | 3.1871 | 0.77235 |
| 60-69 (n=13) | 3.7146 | 1.18426 | 0.2723 | 0.09057 | 0.9477 | .32458 | 2.8646 | 0.79489 |
Showing frequency and percentage of subjects according to MCI.
| Mandibular Cortical Index | Frequency | Percent (%) |
|---|
| C1 | 8 | 20.0 |
| C2 | 21 | 52.5 |
| C3 | 11 | 27.5 |
| Total | 40 | 100.0 |
MCI as a Diagnostic Test.
| Components | Value |
|---|
| Specificity | 88.88888889 |
| Sensitivity | 100 |
| Negative Predictive Value | 100 |
| Positive Predictive Value | 96.875 |
Discussion
Dental panoramic radiography is frequently performed for the diagnosis of diseases which affect the dento-maxillofacial complex. The incidental findings which are detected on dental panoramic radiographs may be used to identify women who have no awareness on their low BMDs and they would benefit from BMD testing [11].Studies which have compared all these indices (MI, PMI, AI, GI and MCI), age correlation and number of teeth which remained, all in a single sample, have not been frequently found in the literature till date [12,13]. It is considered that osteoporosis could be the reason behind mineral density and mass reduction of jawbones [14]. The thickness of the inferior border tends to reduce in subjects with osteoporosis [7,15], although some studies have found no relationship between skeletal and mandibular BMD [16,17].
Cortical thickness of the inferior border of mandible below the mental foramen is the site which has often been measured [14]. The difference in the mean Mental Index between the three groups in our study was found to be statistically significant (p = 0.00). This result was in accordance with the findings of Devlin et al., where MI was found to contribute significantly to a diagnosis of low skeletal bone mineral density [16]. Also, studies which were done by Estera et al., [14] and Taguchi et al., [18] showed similar results. Post–Hoc Tukey’s test showed that MI could importantly differentiate between osteopaenia and osteoporosis. This result was also confirmed by Mahl et al., [7].
PMI is a radiomorphometric method which was presented in 1991 by Benson et al., [19]. It has been suggested that despite the alveolar bone resorption above the foramen, the distance from the foramen to the inferior border of the mandible remains relatively constant throughout life. Also, the selection of a ratio as the basis of the PMI represented an attempt which was made to compensate for image distortion and magnification which were inherent in panoramic imaging. The difference in mean PMIs between the DEXA groups was statistically significant (p = 0.007), which showed a correlation between the low bone mass density in post-menopausal women and the PMI. Studies which were done by Benson et al., [20] and Khojastehpour et al., [21] have also shown similar results, but Drozdzowska et al., in their study, showed that there was no correlation between PMI and DEXA measurement and they suggested that it should not be used as an indicator of skeletal status [17].
In the present study, no significant relationship was observed between AI and low bone mass density (p = 0.135), which was in contrast to the results of Ledgerton et al., [22] and Mahl et al., [7]. Dutra et al., [23] suggested many reasons to prove that AI was a poor index to use for a radiographic osteoporosis assessment. These included the methodological problem of localisation of the line that “best fits” the anterior border of the ascending ramus, the interaction between dental status and AI, the low correlation with MI in younger individuals, and the lack of data which related this index to the BMD values. Therefore, they suggested that its use as a radiomorphometric index should be discouraged.
According to Bras et al.,[24] the relatively constant thickness of cortical bone at the mandibular angle, following the adolescent growth spurt and the decrease in cortical thickness in post-menopausal women, suggested that the cortical thickness may be useful as a parameter for evaluating metabolic bone loss. In our study also, there was a significant difference in the mean GIs of the three groups, which had p values of 0.00. This result was in accordance with those of the other studies which were done by Estera et al., [14] and Mahl et al.,[7].
One of the most commonly studied parameters of mandibular bone with respect to osteoporosis is the porosity of the mandibular cortical bone. Results of our study showed a significant correlation between the skeletal BMD and MCI (p = <0.00). A study which was done by Horner and Devlin on 40 edentulous females showed a significant correlation between BMD and MCI, but there were problems in repeatability of assessments, which could limit their use in clinical practice [25]. Taguchi et al., [2] reported that subjects with severely eroded cortices had significantly lower vertebral BMDs than those with mildly to moderately eroded cortices or normal cortices. The study of Yasar and Akgunlu [13] concluded that cortical width at mental foramen and PMI did not lend themselves to the diagnosis of osteoporosis and MCI, which had a relatively easier application is a useful oral sign in screening patients for osteoporosis.
Our study showed excellent intra-observer variabilities in the measurements (kappa value 1) for all the indices. The study of Jowitt et al., [26] demonstrated that even among expert observers, there were limitations in the MCI reproducibility, particularly in the inter-observer agreements. Drozdzowska et al., had found a substantial intra and inter-observer agreement in their study (k = 0.66-0.75) of MCI, which was better than moderate and worse than almost perfect, which seemed to be sufficient for use in clinical practice by a trained observer, which was in accordance with our study findings [17]. Besides their reproducibility, the validity of these indices, however, depends on their sensitivity and specificity as compared to the bone mineral densitometry results [7]. In our study, MCI was used as a diagnostic criteria and it was compared with gold standard i.e. DEXA results. Thus, sensitivity and specificity of MCI showed good results, with their values being 100% and 88.88% respectively. In another study, the sensitivity and specificity values for MCI were 77% and 53% respectively [7]. The study of Drozdzowska et al., [17] showed a sensitivity and a specificity of 93% and 31 % respectively.
Taguchi et al., in their study, suggested that it was possible that the crude threshold of cortical width for identifying low vertebral BMD or osteoporosis in Japanese post-menopausal women could not be used directly for British post-menopausal women, because of the difference in the sizes of their mandibles [2]. Also, no published data are available, which have prescribed the threshold values for the various mandibular indices, which can be used in the Indian population, as studies with larger sample sizes have not yet been conducted in India.
Conclusion
Finally, dentists who use Orthopantomographs may play a vital role in screening patients with osteoporosis, mainly post-menopausal women; this is because, it is most often advised as a part of routine investigation and as it is also less expensive than DEXA scan. Mandibular Cortical Index can reliably be used as a diagnostic tool for screening patients with osteoporosis. By utilising the results of this study, undertaking further studies in this field may throw some light on patients with secondary osteoporosis and on male patients with low bone mineral density.
Limitations
To determine the reliability of other indices (MI, PMI and GI) as well as determination of specific cutoff values which can be applicable in the Indian population, further studies with larger sample sizes are needed. This would pave way for a further definitive correlation between osteoporosis in mandible and other skeletal bones in the body.
Chi Square value = 4.283; df = 4; p value = 0.369; Not significant
Tests used: One way ANOVA, Post–hoc Tukey testOne way ANOVA: * indicates statistically significant difference at p ≤ 0.05.Post–hoc Tukey test: Groups with same letter superscripted are not statistically significant.