Dentin hypersensitivity is generally characterized by a short sharp pain which arises due to exposed dentin typically, in response to external stimuli such as thermal, evaporative, tactile, osmotic or chemical forces and which cannot be explained by any other form of dental defect or pathology [1]. Pain which is caused by dentin hypersensitivity hinders an individual’s everyday activities, such as brushing, eating, drinking, speaking, and even breathing [2]. However, a majority of the patients do not seek treatment for desensitizing their teeth, because they do not perceive dentin hypersensitivity as a severe oral health problem and prefer over the counter products when the problem becomes severe [3].
In general, the incidence of hypersensitive dentin ranges from 10% to 30% of the population [2]. Studies have shown that dentin hypersensitivity was frequently observed between the age group of 20 and 50 years, with women showing more prevalence [4].
This condition generally involves the facial surfaces of teeth near the cervical border, and it is very common in canines, premolars, and molars [5]. It has been established beyond doubt that the aetiology of dentin hypersensitivity is multifactorial. Most common clinical cause is gingival recession [6] which exposes the root surface due to periodontal treatment, surgical/dental operative procedures, gum diseases, aging and incorrect tooth brushing or association of two or more of these factors [7,8]. Other factors include patients’ deleterious habits, poor hygiene, diet, exposure of teeth to chemical products, chewing tobacco, excessive occlusal forces, and premature occlusal contacts [9,10].
Several theories have explained dentin hypersensitivity; the most widely accepted theory is hydrodynamic theory which was presented by Brannstrom and Astron [11], which suggested that the fluids within the dentinal tubules flowed due to thermal, mechanical, evaporative, and osmotic stimuli. The flow of liquids in dentinal tubules can trigger nerves along the pulpal canal of the dentin, thus causing pain [12]. Thus, the main approach in the treatment of dentin hypersensitivity is closing dentinal tubules by e.g. crystal precipitation in tubule lumen or hydroxyapatite melting [3]. In general, laser therapy, preparations with fluorine, hydroxyapatite, strontium and zinc chlorides and potassium oxalate, as well as dental adhesives and glass ionomer cement are used for the treatment of dentin hypersensitivity [8,13,14]. Despite the large number of published studies, however, there is still no consensus on as to which product constitutes the “gold standard” for dentin hypersensitivity treatment [3,9].
At present, the commonly used desensitizing agents generally are favourable for a short-time, while they blow the mark in a long-term. So, the development of new desensitizing agents is needed [3,8]. The search for a natural desensitizing agent with long lasting effects has led to the observation that propolis had promising effects on dentin hypersensitivity [16]. Propolis is a naturally-occurring bee product. It is widely used in homeopathic and herbal practices as an antiseptic, anti-inflammatory, antimycotic, and a bacteriostatic agent [16]. Some in vitro studies have shown that, propolis had a clinically significant effect on reduction of dentin permeability [17], but to date, only very few studies have been done on desensitizing effect of Propolis in–vivo.
So, the aim of the present in–vivo study was to “evaluate the clinical effect of two different desensitizing agents on reduction of dentin hypersensitivity”.
Material and Methods
An in–vivo, randomized, double blind, split mouth, negative controlled clinical trial was conducted among patients of central jail, Bhopal, who fulfilled the following selection criteria.
Selection Criteria
Inclusion Criteria
Patients who were aged 18– 40 years, who resided in Central Jail, Bhopal, India.
Patients who had at least 3 caries-free cervical lesions with dentinal hypersensitivity.
The loss of dentin should be less than 2 mm deep as per Tooth Wear Index (TWI) code ‘2’ and ‘3’ (a defect of up to 2 mm thick/ loss of enamel and a substantial loss of dentin, but not exposing pulp or secondary dentin) [18].
Patients with adequate oral hygiene and only those who were willing to participate in the study.
Exclusion Criteria
Patients with a history of any systemic illnesses and/or psychological diseases, and previous hospitalization.
Teeth which had dental caries, cracks or fractures in the cervical areas of the teeth.
Teeth with TWI codes 0 (no change of contour), 1 (minimal loss of contour) and 4 (a defect which was more than 2 mm deep/ pulp exposure, or exposure of secondary dentin).
Teeth with any extensive or unsatisfactory restorations, prostheses or orthodontic appliances which involved the cervical areas.
Patients with a history of drug addictions and use of analgesic and/or anti-inflammatory drugs.
Patients who failed to give their consents.
Withdrawal criteria: Patients who failed to complete the follow-up after undergoing initial treatment.
Method of Collection of Data
The research protocol was approved by the Ethics Committee of People’s Dental Academy, Bhopal. Approval from the higher authorities of the Central jail, Bhopal, was also taken to conduct the trial.
A preliminary screening of 100 individuals was done at central jail premises, Bhopal. A pre-designed Dental Chart Form was used for each patient to record cervical abrasion by using Tooth Wear Index (TWI, Smith and Knight, 1984) [18]. The TWI is usually assessed on visual examination. It evaluates all the tooth surfaces (i.e. cervical, buccal (labial), lingual and occlusal or incisal). In the present study, only the cervical surfaces were evaluated for abrasion and they were coded according to criteria of TWI. This modification was done to focus on the objectives of the study.
Patients who scored TWI codes ‘2’ or ‘3’ and had at least 3 cervical lesions with dentinal hypersensitivity were eligible for participation in the study. The purpose behind this selection was just to keep the trial conditions as similar as possible among all the study participants.
Participants were informed about the purpose and design of the investigation and they signed appropriate informed consent forms.
Sample size: A sample which consisted of 73 teeth of 13 patients with dentinal hypersensitivity, who had fulfilled the selection criteria. The power of the sample was 80% for the default significance level (alpha level) at 0.01. The experimental period was 3 weeks.
Experimental procedure: Clinical diagnosis was performed by using a uniform source of light which was provided by a conventional operating dental light system, a mouth mirror, an explorer and periodontal probe in the dental wing of Central Jail, Bhopal.
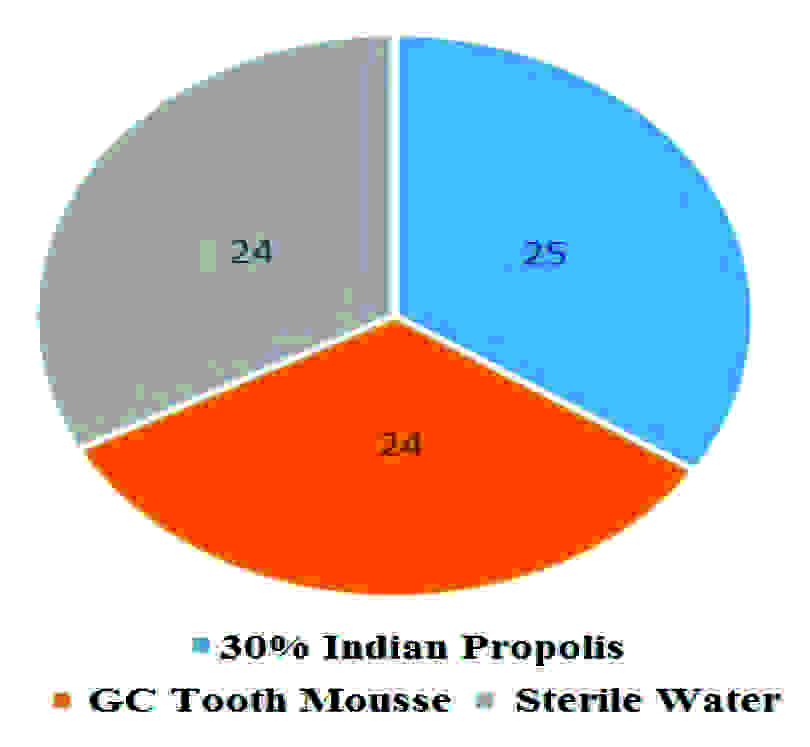
A registry of patients who met the selection criteria was created and a Clinical Report Form (CRF) was prepared for each participant. All the teeth were divided into three treatment groups. A list of selected teeth was prepared and they were arranged in a sequence. One tooth was randomly selected from the list and remaining additional teeth were selected at evenly spaced intervals of 3 units systematically, till a desired sample of 25 was obtained for Group A. A similar procedure was employed to select the teeth for Group B and Group C and desired samples of 25 and 24 were obtained respectively.
Group A: 30% Indian Propolis as a test group (n=25).
Group B: GC Tooth Mousse (RecaldentTM) (n=24).
Group C: Sterile distilled water (n=24).
In order to avoid bias on the part of the investigators and the patients, a double blind technique was used, where neither the scorers of the pain who examined the patients nor the patients themselves were aware of the desensitizing agents which were applied.
Method of Application: The desensitizing agents were applied by a trained and experienced operator, on days 1, 7, 14 and 21 as follows:
Removal of debris and calculus, if any, around the affected teeth by using hand scalers.
Isolation of the teeth with cotton rolls.
Drying of tooth surfaces with a cotton pellet.
Application of Propolis extract and sterile water directly on the dentinal hypersensitivity sites by using truncated needles and letting them to dry for 60 seconds. GC tooth mousse was applied to the sensitive lesions as was recommended by the manufacturer.
Taking care to ensure that none of the products touched other zones of the oral mucosa.
Removal of excess of desensitizing agents by using cotton pellets.
The patients were instructed not to rinse, eat or drink for 30 minutes after the treatment and to avoid using any other professionally or self-applied desensitizing agent in the course of the investigation.
Examiner calibration: The effectiveness evaluation was done by a calibrated examiner. The calibration of the examiner was done at the Department of Public Health Dentistry in Peoples Dental Academy, Bhopal. The examiner was trained and calibrated to record the sensitivity patterns on a group of 10 patients who were diagnosed with dentinal hypersensitivity. The intra examiner weighted kappa value was calculated by using the baseline values for hypersensitivity and by reexamining all the patients. It was determined to be 0.73.
Treatment evaluation procedure: Each tooth received two stimuli [19]: Clinical probing (tactile stimulus) and Air blast (thermal evaporative stimulus). The probing stimulus was applied under slight manual pressure in the mesio-distal direction on the cervical area of the tooth. The test was repeated three times before the final score was recorded. Air blast was applied with an air syringe for 1-2 sec. at a distance of 1 cm from the tooth surface, to avoid desiccation of the dentin surface, while the adjacent teeth were protected by the examiner’s finger [20]. The degree of hypersensitivity which was reported by the participant with each stimulus was determined according to the Verbal Rating Scale (VRS) [19], from 0 to 3, in which: 0= no discomfort, 1= minimum discomfort, 2= mild discomfort, and 3= intense discomfort. The values were collected before the intervention (baseline values) and after each application, on days 1, 7, 14, and 21 respectively.
Statistical Analysis
All the data were entered into a personal computer in a Microsoft Excel sheet. Descriptive statistical analysis was performed by using SPSS. software, version 19. The reduction in dentin hypersensitivity in all the three treatment groups at different time intervals was analyzed by using Chi–square test. All the results which were obtained were tabulated and graphs were prepared. The level of statistical significance was set at 0.01.
Results
A total of 13 male patients with a mean age of 37 years, who presented 73 hypersensitive teeth, were evaluated in the study. All the participants followed and completed the trial and so the patient compliance rate was 100%. [Table/Fig-1] shows the distribution of teeth into 3 treatment groups.
Showing the total number of teeth distributed in each group
[Table/Fig-2] shows distribution of types of teeth which were affected by dentin hypersensitivity. The highest number of teeth which were affected with dentin hypersensitivity were anterior and pre-molars (30 each), followed by molars (n=13).
Distribution of types of teeth affected with dentin hypersensitivity
| Treatment Group | Incisors (n) | Canines (n) | Pre-molars (n) | Molars (n) | Total (n) |
|---|
| 30% Indian Propolis (Group A) | 11 | 4 | 6 | 4 | 25 |
| GC tooth mousse (Group B) | 8 | 1 | 13 | 2 | 24 |
| Sterile water (Group C) | 2 | 4 | 11 | 7 | 24 |
| Total | 21 | 9 | 30 | 13 | 73 |
[Table/Fig-3] shows percentage reduction in severity of dentinal hypersensitivity for each group at different time intervals for air blast stimulus. In 30% Indian propolis group, at baseline, highest number of teeth showed moderate pain i.e. 56%. After 4th application, the number of teeth with mild pain was 60%. The difference in reduction of severity of teeth was statistically significant (i.e. p= 0.000).
The percentage reduction in severity of dentinal hypersensitivity for each group at different time intervals for air blast stimulus
| Groups | Severity | Baseline score n (%) | 1st application (Day 1st) n (%) | 2nd application (Day 7th) n (%) | 3rd application (Day 14th) n (%) | 4th application (Day 21st) n (%) | Statistical inference |
|---|
| 30% Indian propolis (Group A) | No Pain | 0 (0%) | 6 (24.0%) | 2 (8%) | 5 (20%) | 3 (12%) | χ2 = 50.9 df = 12 p = 0.000* |
| Mild | 4 (16%) | 7 (28%) | 19 (76%) | 14 (56%) | 15 (60%) |
| Moderate | 14(56%) | 11 (44%) | 4 (16%) | 6 (24%) | 7 (28%) |
| Severe | 7 (28%) | 1 (4%) | 0 (0%) | 0 (0%) | 0 (0%) |
| GC tooth mousse (Group B) | No Pain | 1 (4.2%) | 8 (33.3%) | 11 (45.8%) | 17 (70.8%) | 16 (66.7%) | χ2 = 57.6 df = 12 p = 0.000* |
| Mild | 7(29.2%) | 11 (45.8%) | 11 (45.8%) | 6 (25%) | 8 (33.3%) |
| Moderate | 9(37.5%) | 4 (16.7%) | 2 (8.3%) | 1 (4.2%) | 0 (0%) |
| Severe | 7(29.2%) | 1 (4.2%) | 0 (0%) | 0 (0%) | 0 (0%) |
| Sterile water (Group C) | No Pain | 0 (0%) | 1 (4.2%) | 1 (4.2%) | 3 (12.5%) | 1 (4.2%) | χ2 = 19.1 df = 12 p = 0.086 |
| Mild | 9(37.5%) | 8 (33.3%) | 4 (16.7%) | 9 (37.5%) | 7 (29.2%) |
| Moderate | 7(29.2%) | 8 (33.3%) | 14 (58.3%) | 10 (41.7%) | 15 (62.5%) |
| Severe | 8(33.3%) | 7 (29.2%) | 5 (20.8%) | 2 (8.3%) | 1 (4.2%) |
*p<0.01.
In GC tooth mousse group, at baseline, highest number of teeth had moderate pain (37.5%). In 2nd application, no tooth showed severe pain. While, after 4th application, teeth with no pain increased to 66.7%. The difference in reduction of severity of teeth was statistically significant (i.e. p= 0.000).
In placebo group, the difference in reduction of the severity of teeth was not statistically significant (i.e. p= 0.086).
[Table/Fig-4] shows percentage reduction in severity of dentinal hypersensitivity for each group at different time intervals for probing stimulus. In 30% Indian propolis group, at baseline, 36%, teeth had moderate pain. After 4th application, the teeth with mild pain increased to 52%; however, 36% teeth had no pain. The difference in reduction of severity of teeth was statistically significant (i.e. p= 0.001).
The percentage reduction in severity of dentinal hypersensitivity for each group at different time intervals for probing stimulus
| Groups | Severity | Baseline score n (%) | 1st application (Day 1st) n (%) | 2nd application (Day 7th) n (%) | 3rd application (Day 14th) n (%) | 4th application (Day 21st) n (%) | Statistical inference |
|---|
| 30% Indian propolis (Group A) | No Pain | 3 (12%) | 9 (36%) | 8 (32%) | 10 (40%) | 9 (36%) | χ2 = 34.5 df = 12 p = 0.001* |
| Mild | 8 (32%) | 8 (32%) | 15 (60%) | 9 (36%) | 13 (52%) |
| Moderate | 9 (36%) | 8 (32%) | 2 (8%) | 6 (24%) | 3 (12%) |
| Severe | 5 (20%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) |
| GC tooth mousse (Group B) | No Pain | 3(12.5%) | 9 (37.5%) | 7 (29.2%) | 15 (62.5%) | 18 (75%) | χ2 = 52.2 df = 12 p =0.000* |
| Mild | 8(33.3%) | 7 (29.2%) | 12 (50%) | 9 (37.5%) | 6 (25%) |
| Moderate | 6 (25%) | 8 (33.3%) | 3 (12.5%) | 0 (0%) | 0 (0%) |
| Severe | 7(29.2%) | 0 (0%) | 2 (8.3%) | 0 (0%) | 0 (0%) |
| Sterile water (Group C) | No Pain | 2 (8.3%) | 5 (20.8%) | 2 (8.7%) | 1 (4.2%) | 0 (0%) | χ2 = 18.5 df = 12 p = 0.100 |
| Mild | 7 (29.2% | 4 (16.7%) | 10 (43.5%) | 11 (45.8%) | 9 (37.5%) |
| Moderate | 6 (25%) | 10 (41.7%) | 9 (39.1%) | 9 (37.5%) | 11 (45.8%) |
| Severe | 9(37.5%) | 5 (20.8%) | 2 (8.7%) | 3 (12.5%) | 4 (16.7%) |
*p<0.01.
In GC tooth mousse group, at baseline, the teeth with mild pain were 33.3%, those with moderate pain were 25% and those with severe pain were 29.2% respectively. After 4th application, teeth with no pain increased to 75%. The difference in reduction of the severity of teeth was statistically significant (i.e. p= 0.000).
In placebo group, the difference in reduction of the severity of teeth was not statistically significant (i.e. p= 0.100).
[Table/Fig-5] shows the overall reduction in dentinal hypersensitivity, both for air blast and probing stimulus. In GC tooth mousse group, the overall reduction in DH was 91.6%. However, in 30% Indian propolis group, the overall reduction was 78%.
overall reduction in dentin hypersensitivity both for air blast and probing stimulus
| Group | Rapid reduction (1st & 2nd application) n (%) | overall reduction (after final application) n (%) | No reduction (after final application) n (%) |
|---|
| 30% Indian propolis (25) | 19.5 (78%) | 19.5 (78%) | 5.5 (22%) |
| GC tooth mousse (24) | 19.5 (81.2%) | 22 (91.6%) | 2 (8.4%) |
| Sterile water (24) | 7 (29%) | 8.5 (35.4%) | 15.5 (64.5%) |
Discussion
The present study was a pioneering randomized, double blind controlled clinical trial that evaluated the clinical effect of 30% ethanolic extract Indian propolis as compared to that of GC tooth mousse in reducing dentin hypersensitivity.
Distribution of dentin hypersensitivity according to severity which was examined in our study was consistent with Kielbassa’s observation, that moderate dentin hypersensitivity was more prevalent than severe or mild varieties [21]. The mean age of 37 years of the study sample correlated with the data which was reported by other researchers, which indicated that dentinal hypersensitivity primarily affected adults who were aged 20-50 years [4]. Similarly, Murray’s [5] observation that pre-molars were commonly affected by dentin hypersensitivity, coincided with the results of our study.
A split mouth study design was adopted which had advantages of same pain perception, oral hygiene habits, dietary habits and psychosomatic factors. It is generally recommended that more than one stimulus should be used in clinical studies which are done on dentinal hypersensitivity. This study utilized air blast and probing stimulation for the evaluation of dentin hypersensitivity. These two methods were reported to be accurate for the investigation of hypersensitivity levels according to Snowinski et al., [22]. In the current study, the effectiveness of the agents was evaluated by using VRS which has been widely used in human clinical and physiological research to assess subjective states [19].
Tung et al., postulated that the materials CPP-ACP and propolis precipitate and obstruct the dentinal tubules and that they decrease dentinal permeability by 85% or more [23]. In this study, agents i.e. GC tooth mousse and 30% ethenolic extract of Indian propolis effectively reduced the dentinal hypersensitivity.
In 1999, Mahmoud et al. conducted a pioneer study on the effect of propolis on dentin hypersensitivity in–vivo. In this study, it was concluded that propolis had a positive effect on the control of dentin hypersensitivity [24]. In the present study, it is seen that there was a significant reduction in the severity of dentinal hypersensitivity among the teeth which were assigned to 30% Indian propolis group. Its action was slightly slower as compared to that of GC tooth mousse, but still, the number of teeth with mild pain increased markedly. This could be attributed to high content of flavanoids in propolis which may have produced the occluding effect [24]. Flavanoids may be able to suppress the information of free radicals by binding heavy metals in ions which are known to catalyze many processes leading to the appearance of full radicals [24].
G.C. tooth mousse contains casein phosphopeptide (CPP) and amorphous calcium phosphate (ACP). CPP stabilizes ACP and forms nano complexes with ACP at the tooth surface, thereby providing a reservoir of calcium and phosphate ions which favors mineralization [25]. In our study, G.C. tooth mousse was found to be the most effective among the test groups (p<0.01). The initial observation of this medicine revealed that its action was most effective in the first days of application. Perhaps, in order to increase its desensitizing effect, it has been recommended that, this application should be repeated at intervals which were shorter than 7 days [25].
The sterile water, which was used as a negative control in our study showed the least (35.4%) reduction in dentin hypersensitivity. This slight reduction in dentin hypersensitivity may be attributed to placebo effect and participation bias. This study was peculiar in being one of the few where a true placebo, water, was applied to the test teeth.
Dentin hypersensitivity studies are subject based. Therefore, several factors can influence the measurement of pain. To date, none of the methods which have been used to assess the measurements have been found to be completely successful. However, it may be suggested that the aim of dentin hypersensitivity studies is to relieve patients’ discomfort. Hence, long-term studies and repeated applications of desensitizing agents are necessary. To date, no standard procedures have been developed to test products which have been designed for treatment of this condition; hence, comparison of products between trials is fraught with difficulties. In addition, well-designed control groups and working with more subjects may be of great help in obtaining more reliable results.
Study Limitations and Recommendations
No females participated in this study.
Further clinical studies which involve a larger number of patients for evaluating long term effects of dentinal hypersensitivity treatment with propolis are recommended.
Conclusion
Within the parameters of this study, the following conclusions can be drawn:
GC tooth mousse was the most effective among all three treatment agents, followed by 30% ethanolic extract of Indian propolis.
GC tooth mousse and 30% ethanolic extract of Indian propolis not only showed a rapid reduction in dentin hypersensitivity, but also the highest patient satisfaction, without any side effects.
*p<0.01.
*p<0.01.