Urolithiasis in a child with Spondylocarpotarsal Synostosis Syndrome: A Co-Incidence
Ankur Singh1, Seema Kapoor2, Gaurav Pradhan3
1 Senior Research Associate, Department of Paediatrics, MAMC Associated Lok Nayak Hospital, New Delhi, India.
2 Professor Pediatrics, Department of Paediatrics, MAMC Associated Lok Nayak Hospital, New Delhi, India.
3 Professor, Department of Radiology, MAMC Associated Lok Nayak Hospital, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORESPONDING AUTHOR: Dr. Seema Kapoor, M-439, Ground Floor, Guruharkishan Nagar, Paschim Vihar, New delhi, India.
Phone: 9968604313,
E-mail: drseemakapoor@gmail.com
Spondylocarpotarsal synostosis syndrome (SSS) is an autosomal recessive condition which is characterized by short stature, a carpotarsal coalition and a vertebral fusion, but without any rib anomaly. We are presenting a 7– year– old boy, who had uroliathiasis with the spondylocarpotarsal synostosis syndrome. This association, to the best of our knowledge, has not been reported so far.
Spondylocarpotarsal synostosis syndrome, Uroliathiasis
Introduction
Spondylocarpotarsal synostosis syndrome is a vertebral segmentation defect. It is characterised by a vertebral fusion, mainly in thoracic area and a carpotarsal coalition, but with a normal rib morphology. SSS is inherited as an autosomal recessive disorder. Krakow D et al., first identified mutations in filamin B gene which encodes a cytoskeleton protein, as the cause of SSS, in 2004.
Case Report
A seven–year–old boy who was the product of a 3rd degree consanguineous marriage, presented to us with a short –stature, a chest deformity and a bilateral lateral deviation of elbow joint. He had an on and off pain bilaterally in lumbar region for the past 1 month, with dysuria. No history of fever was forthcoming. Clinical examination revealed a height which was below 3rd centile, with an upper and lower segment ratio of 0.84, a short trunk, pectus excavatum, a cubitus valgus deformity, thoracic scoliosis and lumbar lordosis [Table/Fig-1]. Bilateral renal angles were tender. His neurological, ophthalmological and otolaryngological examinations showed normal pictures. He was average in studies, with normal intelligence, as was assessed by Differential ability Scales-Second Edition (DAS)–II. There was no other obvious clinical dysmorphology.
Photograph showing symmetry of chest with mild pectus excavatum

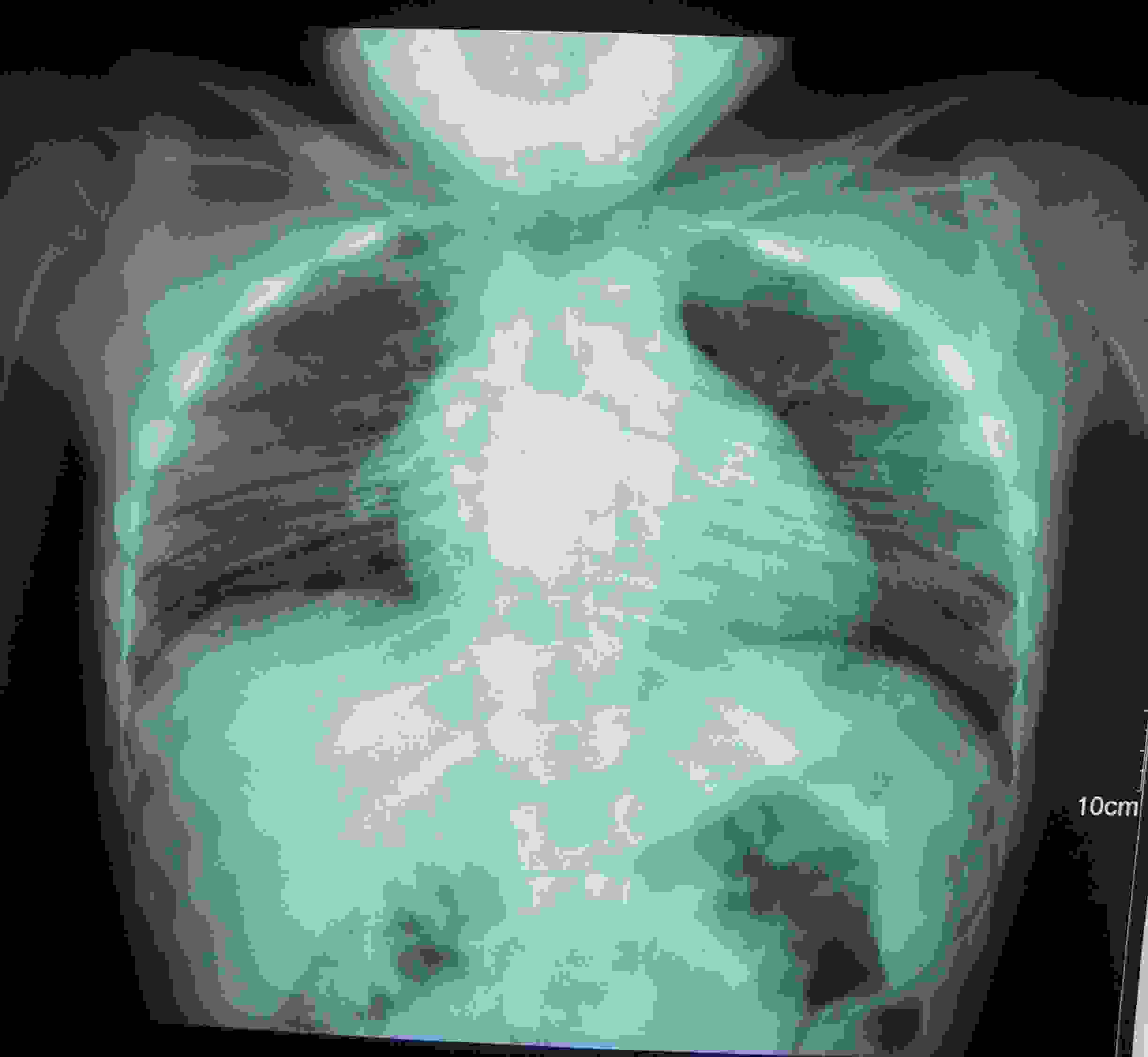
Clinical radiographs revealed a lack of normal segmentation of thoracic vertebrae, minimal dorso-lumbar scoliosis with a convexity to right in dorsal region and a minimal convexity to left in lumbar region [Table/Fig-2]. There was no rib anomaly. X–rays of the bilateral elbow revealed flattening of distal end of humerus, proximal end of radius and ossific centre of capitulum. X–rays of the bilateral hand showed fusion of capitate and hamate [Table/Fig-3]. On radiographs of feet, no tarsal bone fusion was seen. On this basis, a diagnosis of spondylocarpotarsal synostosis was made. Magnetic resonance imaging was not done, as diagnosis was evident on radiographs and as it was unaffordable by the parents of the patient. There was no other obvious deformity. Ultrasonography of the KUB region revealed stones in bilateral kidneys, which were 1.0 x 1.0 cm in size, which were two in number, one on either side. The only unusual finding in our case was presence of uroliathiasis. Constellation of above mentioned skeletal deformities with uroliathiasis has not reported in the published English literature so far, to the best of our knowledge. DNA mutation studies of the filamin gene was not done, as parents could not afford them.
Radiograph revealed a lack of normal segmentation of thoracic vertebrae, minimal dorso-lumbar scoliosis with a convexity to right in dorsal region, minimal convexity to left in lumbar region without any rib anomaly

X–rays of the bilateral hand showed fusion of capitate and hamate
Discussion
Spondylocarpotarsal synostosis syndrome (SSS) (OMIM# 272460) is a rare, multiple congenital anomaly syndrome. The vertebral defects consist of fusion of multiple vertebral bodies in cervical, thoracic and lumbar spine (block vertebrae) and posterior elements of neural arch. The thoracic spine is most commonly involved and it presents with scoliosis if the fusion defects are asymmetric. Other associated features which are reported in literature are ophthalmological abnormalities, cleft palate, sensorineural or conductive deafness and a defective dentition [1]. Eye and dental examinations were normal in present case. He did not have a tarsal bone coalition. In a review of 18 patients which was done by Katia et al., only 6 patients were found to have tarsal synostosis. The unusual finding in our case was presence of uroliathioasis. There are no reports of uroliathiasis in Spondylocarpotarsal synostosis syndrome in published English literature till now. To postulate whether this was due to a deranged calcium turnover or a coincidence is difficult. This highlights the need of a targeted examination of KUB region. There are only two reported cases with renal anomalies, but they do not mention about urolithiasis [2,3]. Individuals with spine deformities with or without chest wall abnormalities are at a risk for thoracic insufficiency syndrome (TIS). The long term management includes chest physiotherapy, management of respiratory tract infections, casting, orthoses and or other specific surgical procedures [4,5]. No long term studies have been done in context to TIS in cases with Spondylocarpotarsal synostosis syndrome.
Differential diagnosis of this condition includes spondylocostal and spondylothoracic dysplasia. Both these conditions present with fused rib anomalies, besides vertebral segmentation defects .The absence of rib anomalies and presence of a carpal bone fusion confirmed our clinical diagnosis.
SSS follows an autosomal recessive pattern of inheritance, with locus of gene on chromosome 3p14 [6]. The mutation in filamin gene encodes a defective cytoskeletal protein which can cause other allelic disorders like Boomrang dysplasia, atelosteogenesis I and III and Larsen’s syndrome.
Genetic studies are backbone for prenatal diagnosis in such cases and other skeletal dysplasia [7,8]. But in developing countries like ours, where such facilities are beyond the reach of many affected families, monitoring with repeated sonographic examinations remains mainstay of investigation.
Conclusion
This case demonstrated that a simple skeletal survey can clinch the diagnosis. A targeted evaluation of KUB region can pick up treatable conditions like urolithiasis. This association or coincidence needs to be evaluated after a significant number of cases have been reported.
[1]. Honeywell C, Langer L, Allanson J, Spondylocarpotarsal synostosis with epiphyseal dysplasiaAm J Med Genet 2002 15:318-22. [Google Scholar]
[2]. Langer LO, Moe JH, A recessive form of congenital scoliosis different from spondylothoracic dysplasiaBD:OAS 1975 11(6):83-86. [Google Scholar]
[3]. Langer LO, Gorlin RJ, Donnai D, Hamel BCJ, Clericuzio C, Spondylocarpotarsal synostosis syndrome (with or without unilateral segmented bar)Am J Med Genet 1994 51:1-8. [Google Scholar]
[4]. Teli M, Hosalkar H, Gill I, Noordeen H, Spondylocostal dysostosis: thirteen new cases treated by conservative and surgical meansSpine 2004 1:1447-51. [Google Scholar]
[5]. Emans JB, Caubet JF, Ordonez CL, Lee EY, Ciarlo M, The treatment of spine and chest wall deformities with fused ribs by expansion thoracostomy and insertion of vertical expandable prosthetic titanium rib: growth of thoracic spine and improvement of lung volumesSpine 2005 1:S58-68. [Google Scholar]
[6]. Steiner C, Ehtesham N, Taylor K D, Sebald E, Cantor R, King L M, A locus for spondylocarpotarsal synostosis syndrome at chromosome 3p14J Med Genet 2004 41:266-69. [Google Scholar]
[7]. Phadke SR, Patil SJ, Kumari N, Krishnani N, Spondylothoracic dysplasia: prenatal diagnosis and the problems of nosologic overlapAm J Med Genet 2007 8:899-902. [Google Scholar]
[8]. Tolmie JL, Whittle MJ, McNay MB, Gibson AA, Connor JM, Second trimester prenatal diagnosis of the Jarcho-Levin syndromePrenat Diagn 1987 7:129-34. [Google Scholar]