Recurrent Phaeohyphomycosis: A Case Report
SN Shirbur1, SR Telkar2, BV Goudar3, Tony Mathew4
1 Professor, Department of General Surgery, S Nijalingappa Medical College, HSK Hospital and Research Centre. Navanagar, Bagalkot-587103, India.
2 Assistant Professor, Department of General Surgery, S Nijalingappa Medical College, HSK Hospital and Research Centre. Navanagar, Bagalkot-587103, India.
3 Associate Professor, Department of General Surgery, S Nijalingappa Medical College, HSK Hospital and Research Centre. Navanagar, Bagalkot-587103, India.
4 Resident, Department of General Surgery, S Nijalingappa Medical College, HSK Hospital and Research Centre. Navanagar, Bagalkot-587103, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr S.N. Shirbur, Professor, Department of General Surgery, S Nijalingappa Medical College, HSK Hospital and Research Centre. Navanagar, Bagalkot-587103, India.
Phone: 09448972509,
E-mail: dr.shirbur.s@gmail.com
Phaeohyphomycoses are rare, opportunistic, fungal infections which are usually seen in immunocompromised individuals. We are reporting a case of a 40-year-old man with recurrent cutaneous phaeohyphomycosis, who did not have any clinical evidence of immunodeficiency, who presented with signs which resembled a malignancy of the skin.
Phaeohyphomycoses, Fungal infection
Case Report
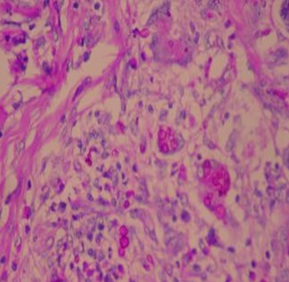
A 40-years-old male, who was agriculturist by occupation, who had no previous medical illness, presented with a recurrent growth over the left forearm and elbow region, which he had got operated 3 years back. He was otherwise in sound health. The patient denied any apparent antecedent trauma, contact with chemicals, arthropod bites, a family history of or contact with a person with similar lesions or foreign travel. The lesions were non itchy and they were formed by several confluent nodular areas (cauliflower like) which had a foul smelling haemopurulent discharge. He had similar growths over his forehead, back and left elbow 3 years back, which were excised and grafted in a local hospital. He was on irregular antifungal treatment. His physical examination revealed three non-tender, cauliflower like growths in the medial, anterior and lateral aspects of arm, just above elbow joint, of sizes 5 × 5 cm, 10 × 5 cm and 6 × 3 cm respectively (over the grafted areas). On naked eye examination, no grains were visualised in the haemopurulent discharge [Table/Fig-1]. There was no restriction in the movements of elbow. Regional lymph nodes were not enlarged and there was no thickening of peripheral nerves or loss of sensations. The systemic examination revealed no abnormalities. Results of the following laboratory studies were normal or negative: complete haemogram, blood chemistry analysis, Venereal Disease Research Laboratory (VDRL) test and Human Immunodeficiency Virus (HIV) antibody. An X-ray of the affected extremity showed no sign of osteolysis or a periosteal reaction. At the initial visit, a 3-mm punch biopsy was aseptically obtained from each lesion and specimens were sent for histopathological studies. The histological sections revealed phaeohyphomycosis; a mycosis which is caused by a dematiaceous (brown or black) fungus [Table/Fig-2]. Since the growth was exuberant and fungating, he was subjected to a wide excision and skin grafting, which were done in a single setting. Excised tissue sections were stained with haematoxylin and eosin, Gomori’s Methylamine Silver (GMS) stain and periodic acid – Schiff staining and they demonstrated numerous darkly pigmented, septate, hyphal fragments which were admixed with yeast like spores, which were consistent with the diagnosis of Phaeohyphomycosis. Histopathological examination of the serial sections showed no evidence of dysplasia or any carcinomatous changes. The margins of excised tissue were clear of any fungal pathology. He was put on a long term antifungal treatment.
Showing Recurrent Phaeohyphomycosis of the forearm

Showing microscopic appearance of haeohyphomycosis
Discussion
Aiello coined the term, ‘phaeohyphomycosis’ in 1974, which refers to mycosis which is caused by a dematiaceous (brown or black) fungus [1]. Dematiaceous fungi are characterised by their dark pigmentation which is derived from the melanin complex in their cellular wall. They are ubiquitous in nature and are found mostly in soil and vegetation. An infection is probably introduced by a traumatic inoculation or inhalation of the aetiologic agent. A trivial, un-noticed trauma could have been responsible for initiation of the infection in this case [2–5]. Clinical presentations are greatly influenced by the immune status of the host. Skin and subcutaneous tissue involvement is termed as subcutaneous phaeohyphomycosis, and it is characterised by papulonodules, verrucous, hyperkeratotic or ulcerated plaques, cysts, abscesses, pyogranuloma, non-healing ulcers or sinuses. In addition, immunocompromised patients are at a risk of locally invasive phaeohyphomycosis, and rarely, but often fatal pneumonia or disseminated disease. All dematiaceous fungi are similar and they can’t be differentiated in the tissues, solely on the basis of their morphologies. For a specific identification, culturing is required. In India, the commonly associated genera which are seen are exophiala, phialophora, cladosporium, curvularia, fonsecaea and alternaria [5]. Laboratory diagnosis includes isolation of fungal hyphae on potassium hydroxide mounts and culture on Sabouraud’s dextrose agar. Histopathologically, the lesions show brown-walled septate hyphae or yeast or a combination of both in tissue. The Fontana-Masson stain (specific for melanin), periodic acid – Schiff and Gomorimethenamine – silver stain can be used to confirm the diagnosis [5–6]. The optimal treatment of phaeohyphomycosis often includes a surgical excision which is combined with anti – fungal therapy for several months. Some authors have proposed Mohs micrographic surgery as an effective therapeutic option. This constitutes an alternative to the prolonged, expensive pharmacological treatments that require laboratory follow – ups. An additional benefit is the minimal tissue loss with surgical removal of the lesions [7]. Reported overall cure rates for phaeohyphomycosis could not be found in the literature.
Conclusion
Despite a difficult diagnosis and a rare occurrence, physicians and surgeons should be aware of infection with this emerging fungus, especially in immunocompromised patients. It should also be remembered that it can often be misdiagnosed as a carcinomatous non healing ulcer. Surgery is effective for the eradication of phaeohyphomycosis and for potentially eliminating the need of a costly long – term antifungal therapy.
[1]. McGinnis MR, Rinaldi MG, Winn RE, Emerging agents of phaeohyphomycosis: pathogenic species of Bipolaris and ExserohilumJ Clin Microbiol 1986 Aug 24(2):250-59. [Google Scholar]
[2]. Caligiorne RB, de Resende MA, Dias-Neto E, Oliveira SC, Azevedo V, Dematiaceous fungal pathogens: analysis of ribosomal DNA gene polymorphism by polymerase chain reaction-restriction fragment length polymorphismMycoses 1999 42(11-12):609-14. [Google Scholar]
[3]. Sharma NL, Mahajan V, Sharma RC, Sharma A, Subcutaneous pheohyphomycosis in India--a case report and reviewInt J Dermatol. 2002 Jan 41(1):16-20. [Google Scholar]
[4]. Somani VK, Razvi F, Sharma VK, Sita VN, Sucharita V, Primary cutaneous phaeohyphomycosisIndian J Dermatol Venereol Leprol 1996 Nov-Dec 62(6):363-64. [Google Scholar]
[5]. Revankar SG, Dematiaceous fungiMycoses 2007 50:91-101. [Google Scholar]
[6]. Rinaldi MG, PhaeohyphomycosisDermatol Clin 1996 14:147-53. [Google Scholar]
[7]. Bogle MA, Rabkin MS, Joseph AK, Mohs micrographic surgery for the eradication of phaeohyphomycosis of the handDermatol Surg 2004 Feb 30(2 Pt 1):231-33.discussion 233 [Google Scholar]