Spontaneous Intrahepatic Type II Gallbladder Perforation: A Rare Cause of Liver Abscess – Case Report
Kumkum Singh1, Amit Singh2, Shivaji H Vidyarthi3, Satyaprakash Jindal4, Chandra Kumar Thounaojam5
1 Professor & Head, Department of Surgery, Jawahar Lal Nehru Medical College, Ajmer Rajasthan-305001, India.
2 Senior Resident, Department of Surgery, Jawahar Lal Nehru Medical College, Ajmer Rajasthan-305001, India.
3 Senior Resident, Department of Surgery, Jawahar Lal Nehru Medical College, Ajmer Rajasthan-305001, India.
4 Assistant Professor, Department of Surgery, Jawahar Lal Nehru Medical College, Ajmer Rajasthan-305001, India.
5 Resident, Department of Surgery, Jawahar Lal Nehru Medical College, Ajmer Rajasthan-305001, India.
NAME, ADDRESS, E-MAIL ID OF THE CORESPONDING AUTHOR: Dr. Kumkum Singh, Professor & Head, Department of Surgery, K19, Adarsh Nagar, Ajmer Rajasthan 305001, India.
E-mail: Kum_singhajm@yahoo.co.in
A liver abscess formation is a rare complication of a gallbladder perforation, with a cholecystohepatic communication. Niemeier, in 1934, classified free gallbladder perforations and generalised biliary peritonitis as an acute or a Type I gallbladder perforation, a pericholecystic abscess and localised peritonitis as a subacute or a Type II gallbladder perforation, and cholecystoenteric fistulas as chronic or Type III gallbladder perforations. We are describing a 50–year–old male patient who presented with right upper quadrant pain and was found to have an intrahepatic perforation of the gallbladder. Our patient had a Type II perforation. We have discussed the diagnostic work-up and the management of this rare entity. Due to the high mortality that can be caused by a delay in making the correct diagnosis, a gallbladder perforation represents a special diagnostic and surgical challenge.
Gallbladder perforation, Liver abscess, Niemeier classification
Case Report
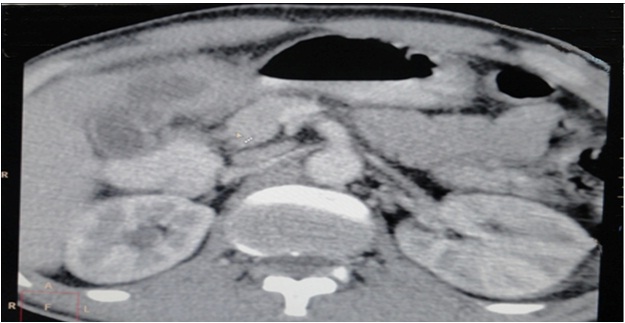
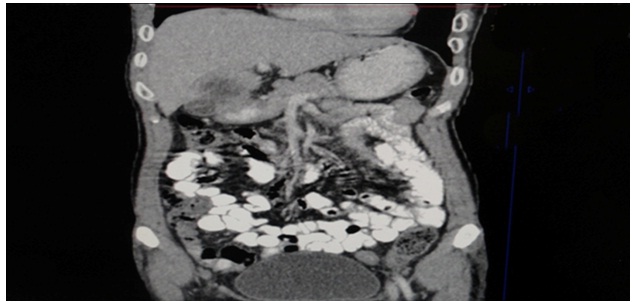
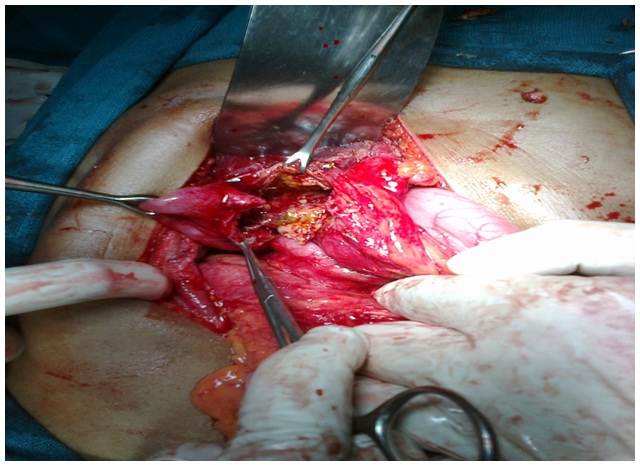
A 50 years old male patient presented with right upper quadrant pain which he had since the past 1 year. Pain was chronic, dull aching in nature and non–radiating. It was mild to moderate in severity, and there were no aggravating or relieving factors. The patient did not give any history of jaundice, fever, vomiting or abdominal distension. On examination, he was found to have a tenderness in the right hypochondrium, but there was no guarding, rigidity or rebound tenderness. No underlying swelling or lump could be appreciated. All laboratory investigations were within the normal limits, except alkaline phosphatse, which are marginally increased. Ultrasonography of abdomen was suggestive of a solitary, 74×39 mm, hypoechoic area in the region of the pylorus, which was probably suggestive of a malignant mass. A few small portahepatis and peripancreatic lymph nodes were seen, along with mild hepatomegaly and, organized sludge in the lumen of the gallbladder. CECT of abdomen was suggestive of a well defined rounded, peripheral rim enhancing, hypodense lesion of size 38×34×43 mm, which was seen in segment 4 of the liver, which was suggestive of a liver abscess. This cavity communicated with the gallbladder [Table/Fig-1 & 2]. Few enlarged peripancreatic lymph nodes were seen (the largest measured 1.1 cm). A diagnosis of an intra-hepatic rupture of gallbladder which had led to a liver abscess, was made. On exploratory laparotomy, it was seen that dense adhesions were present in the gallbladder region, which involved the left lobe of the liver, gallbladder and pylorus. On opening the abscess cavity of left lobe of liver, 50 cc pus was aspirated and a communication was found between abscess cavity and gallbladder [Table/Fig-3]. A subtotal cholecystectomy was done due to presence of dense adhesions in the region of the Calots triangle. Surgery was supplemented with medical therapy in the form of antibiotics (ceftriaxone, and metronidazole), analgesics and proton pump inhibitors for stress ulcer prophylaxis. Enteral nutrition was started on the third post-operative day. The patient made an uneventful recovery and was discharged on the 8th post-operative day.
An axial image of CECT abdomen reveals hepatic abscess communicate with gallbladder
CECT abdomen shows intrahepatic communication of gallbladder and hepatic abscess
Intraoperative findings gallbladder communicate with liver abscess cavity
Discussion
Perforation of the gallbladder is seen in 0.8 - 3.2% of the cases which is present with acute cholecystitis [1], but there is no data on the incidence of gall bladder perforation in patients of chronic cholecystitis. Most of the cases presented with a rupture of biliary contents into the peritoneal cavity. Development of an intra–hepatic abscess with an intra–hepatic perforation represents a rare complication and it has rarely been reported in literature. Although some similar cases had been reported earlier [2] this case was rare, as this case had presented in the era of advanced diagnostic modalities and broad spectrum antibiotics. Comparision of some similar cases has been given in [Table/Fig-4].
Comparisons of similar cases U/S, CT +/- =findings suggestive or not suggestive confirm diagnosis
| S.No. | Author’s | Year’s | Title | Feature’s |
|---|
| Age | Sex | Presentation | Diagnosis | Treatment |
|---|
| Lab | U/s | CT |
|---|
| 1 | Singla S L et al., [3] | 1998 | Gall bladder carcinoma presenting as liver abscess | 65 | M | Acute (Fever) | normal | - | + | Open cholecystectomy with drainage of abscess |
| 2 | Aditya S Bhatwal et al., [4] | 2012 | An usual presentation of gallbladder perforation with hepatic sub capsular collection | 60 | M | Acute (Pain abdomen) | Alakaline-Phosphatase ← | + | + | Open cholecystectomy with peritoneal levage |
| 3 | N P Kamlesh et al., [5] | 2012 | Intra–hepatic rapture of empyma gallbladder | 70 | M | Acute (Pain abdomen) | AST, ALT ← | + | + | U/s guided percuteneous drainage with laproscopic cholecystectomy |
| 4 | KumKum Singh et al., | 2013 | Spontaneous intra–hepatic Type II gallbladder perforation a rare cause of liver abscess | 50 | M | Chronic (Pain abdomen) | AST, ALT ← | - | + | Open subtotal cholecystectomy with drainage of hepatic abscess |
The mortality of this complication is high, even after an aggressive management and multiple interventions, thus making it a diagnostic and a surgical challenge [6]. The gallbladder fundus is most common site for a perforation. A gallbladder perforation is associated with cholelithiasis, infection, malignancy, trauma, corticosteroid therapy, diabetes mellitus, atherosclerotic heart disease, impaired vascular supply, old age and male sex.
Gall bladder perforations are divided into three categories according to the chronicity (acute, subacute, and chronic) and type of perforation (into free abdominal cavity, development of a pericystic abscess, and development of fistulae). A classification which is based on these variables was described first by Niemeier in 1934 [7] [Table/Fig-5].
In 1934 Neimeir’s classified Perforations of the gallbladder into three groups
| Type I | (Acute) is associated with generalized biliary Peritonitis |
| Type II | (Sub acute) consists of the localization of fluid at the site of perforation, pericholecystic abscess and localized Peritonitis |
| Type III | (Chronic) comprises the formation of internal or External fistulae |
With regards to histologically proven chronic-nonspecific cholecystitis and the development of an intrahepatic abscess, this case can be classified as a Type II perforation.
The clinical presentation of an acute gallbladder perforation may occur as right upper quadrant pain, fever or a palpable right upper quadrant mass with tenderness. Elevated liver enzymes, especially raised alkaline phosphatase levels, are commonly observed [8].
It is important to undertake a careful history taking and a physical examination.The chest and abdominal X-ray findings of a right pleural effusion and mottled gas or a localized ileus in the right upper quadrant may be suggestive of a gallbladder perforation. USG may show a gallbladder wall thickening which is of a size of more than 3 mm, a gallbladder distention (largest diameter being >3.5–4.0 cm) and visualization of perforation as a “HOLE SIGN” in which a defect in gallbladder which is visualized is only reliable sign of a gallbladder perforation [6]. CT scans are needed in case of discrepancies between clinical symptoms and sonography findings, and if an ultrasound examination fails in establishing the diagnosis, as well as for a better preoperative planning, subsequent to the sonographically proven perforation, as it was in our case. A CT scan is more sensitive than an ultrasonogram in the diagnosis of a perforation [9]. Biliary imaging, either by doing an per–cutaneous transhepatic cholangiogram or ERCP or a diamethyl iminodiacetic acid (HIDA) scan, may play a significant role in the diagnosis of a gallbladder perforation.
Cholecystectomy, drainage of abscess if it is present and abdominal lavage are usually sufficient for treating Type I gallbladder perforations. A laparoscopic cholecystectomy can be performed after the infection has been relieved by a US guided percutaneous drainage in Type II gallbladder perforations. The intra–hepatic nature of the gallbladder perforation can often lead to a difficulty in laparoscopic cholecystectomy, with a high rate of its conversion to an open cholecystectomy. A cholecystectomy may be difficult in Type III gallbladder perforations and additional surgical procedures such as repair of the fistula may be required.
Conclusion
Perforations of the gallbladder, which lead to liver abscesses, are a rare complication of acute and chronic gallbladder disease, and their intra–hepatic perforations are even rarer. The present experience has shown that gallbladder ruptures must be considered even in patients who present with only mild abdominal symptoms. An early diagnosis of a gallbladder perforation and an immediate surgical intervention are of prime importance in decreasing the morbidity and mortality which are associated with this condition. In these patients, Ultrasound and CT scans are reliable tools for diagnosing gallbladder perforations and for preventing a delay in diagnosis and treatment. The treatment of choice is early surgery in those who are stable enough to tolerate the procedure.
[1]. Stefanidis D, Sirinek KR, Bingener J, Gall bladder perforation: Risk factors and outcomeJ Surg Res 2006 131:204-08. [Google Scholar]
[2]. Kochara K, Kevin V, George M, Vijay J, Intra–hepatic perforation of the gall bladder presenting as liver abscess: case report, review of literature and Niemeier’s classificationEuropean Journal of Gastroenterology and Hepatology 2008 20:240-44. [Google Scholar]
[3]. Singla SL, Garg P, Tahlan RN, Gall bladder carcinoma presenting as liver abscessIndian J Gastroenterol 1998 Apr 17(2):68 [Google Scholar]
[4]. Bhatwal Aaditya S, Deolekar S R, Karandikar Sangram S, An Unusual Presentation of Gall Bladder Perforation with Hepatic Subcapsular CollectionIndian journal of surgery 2012 July DOI 10.1007/s12262-012-0581-x [Google Scholar]
[5]. Naduthottam Palaniswami Kamalesh, Kaniyarakal Pramil, Kurumboor Prakash, Intrahepatic rupture of empyma gallbladder IndianJ Gastroenterol September–October 2012 31(5):280 [Google Scholar]
[6]. Derici H, Kara C, Bozdag AD, Diagnosis and treatment of gallbladder perforationWorld J Gastroenterol 2006 12(48):7832-36. [Google Scholar]
[7]. Niemeier OW, Acute Free Perforation of the Gall-BladderAnn Surg 1934 Jun 99(6):922-24. [Google Scholar]
[8]. Peer A, Witz E, Manor H, Strauss S, Intrahepatic abscess due to gallbladder perforationAbdom Imaging 1995 20:452-55. [Google Scholar]
[9]. Morris BS, Balpande PR, Morani AC, The CT appearances of gallbladder perforationBritish Journal of Radiology 2007 80:898-901. [Google Scholar]