Ganglioneuroma, Base of Tongue: A Rare Entity
Nidhi Mahajan1, Jyotsna Naresh Bharti2, Meeta Singh3, Swapnil Agarwal4, Nita Khurana5
1 Senior Resident, Department of Pathology, Maulana Azad Medical College, New Delhi, India.
2 Senior Resident, Department of Pathology, Maulana Azad Medical College, New Delhi, India.
3 Senior Resident, Department of Pathology, Maulana Azad Medical College, New Delhi, India.
4 Senior Resident, Department of Pathology, Maulana Azad Medical College, New Delhi, India.
5 Professor, Department of Pathology, Maulana Azad Medical College, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORESPONDING AUTHOR: Dr. Jyotsna Naresh Bharti, Senior Resident, Department of Pathology, Maulana Azad Medical College, New Delhi, India.
Phone: 09899047062,
E-mail: jyotsnamamc@gmail.com
We have discussed the case of a solitary polypoid ganglioneuroma in a 45–year–old male patient, at the base of tongue, which mimicked a malignancy. The interest of this case lay in the rarity of its incidence at the base of tongue and its gross resemblance to the more common malignant polypoidal growths at this site. The presence of neural elements and ganglion cells at this site makes it important for an inexperienced histopathologist to differentiate it from other neural lesions of the tongue, in order to avoid a misdiagnosis and this can prevent the clinician from administering an inappropriate treatment. Exhaustive search revealed only a very few case reports on the tongue.
Polypoidal, Tongue, Ganglion, Immunohistochemistry
Case History
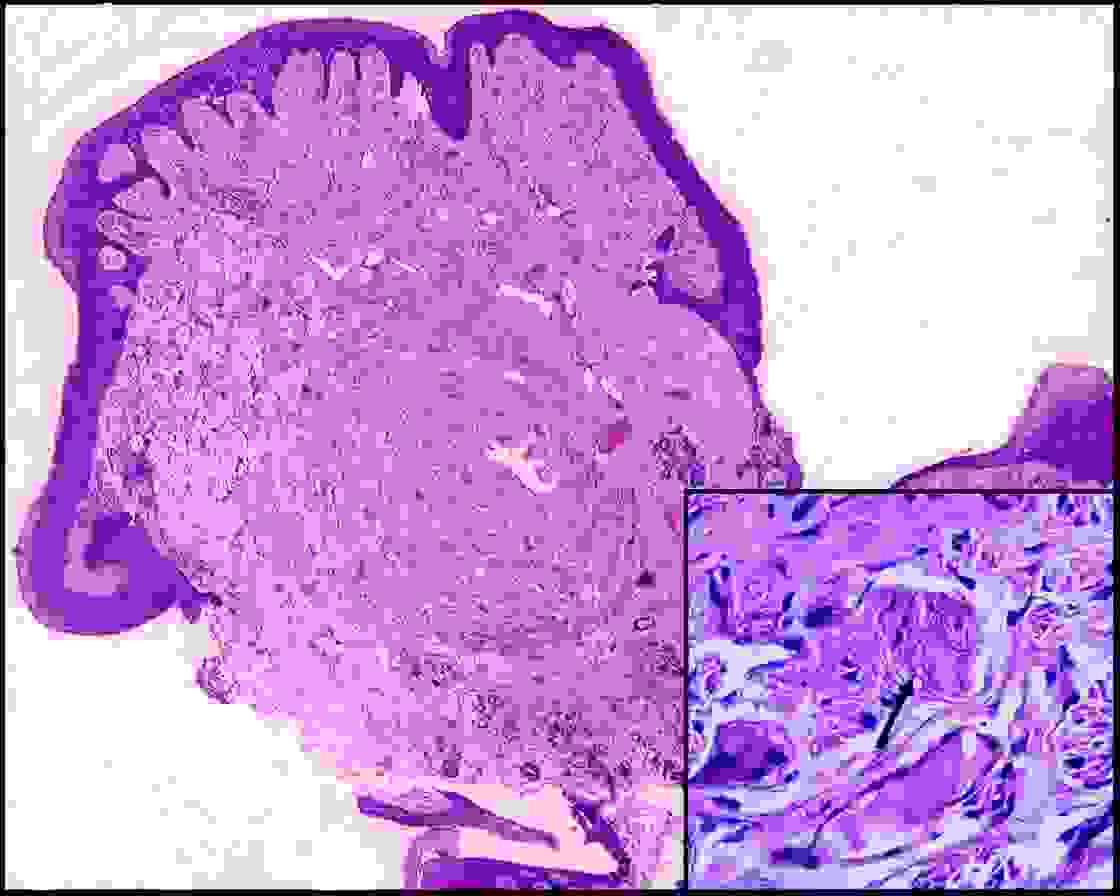
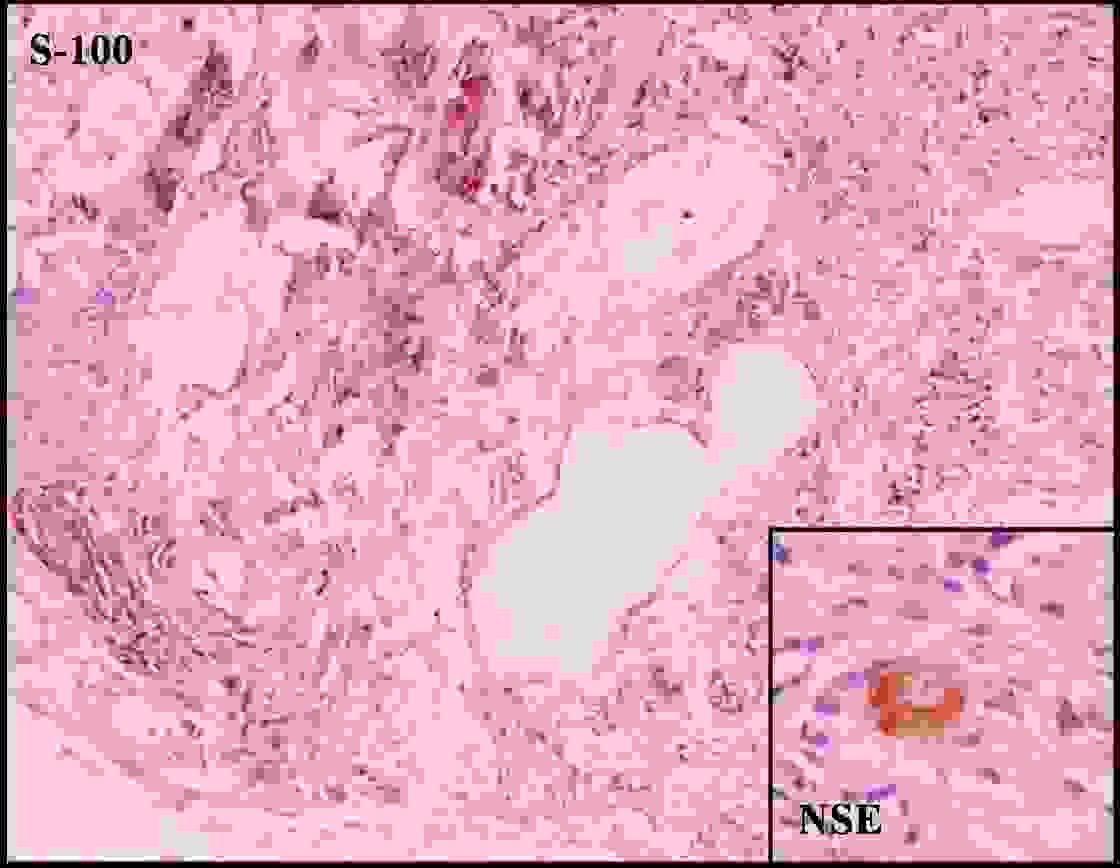
A 45 year old male, a chronic smoker, presented to the clinic with a difficulty in swallowing since the past three months. There was no pain, hoarseness of voice or cervical lymphadenopathy. Indirect laryngoscopy showed a congested submucosal lesion which measured 1.5 cm in diameter, at the base of tongue, on the right side. With a strong suspicion of malignancy, an excision biopsy was taken from this polypoidal growth. Histopathology revealed tissue fragments which were lined by stratified squamous epithelium, which showed mild hyperplasia at places. The subepithelium revealed a well circumscribed proliferation of myxoid neurofibromatous tissue, with interspersed mature ganglion cells [Table/Fig-1], inset shows ganglion cells. The mature ganglion cells varied in size. However, they were large, with abundant granular basophilic cytoplasm, eccentrically placed nuclei and prominent nucleoli. These cells were found to be interspersed throughout neural fibres, singly or in groups. No area of nuclear atypia, mitosis or necrosis was found in the spindle cell component. No immature neuroblastic cells were observed. Ganglion cells showed diffuse immunostaining for Neurone-Specific Enolase (NSE) [Table/Fig-2], inset) and CD56. S-100 protein highlighted the Schwannian element [Table/Fig-2]. Multiple serial sections failed to reveal any other pattern. Thus, a diagnosis of a ganglioneuroma was suggested; following which the patient was thoroughly investigated for similar lesions at other sites, to rule out possibility of MEN IIb, Cowden’s or Von Recklinghausen’s disease. No other cutaneous or visceral lesions were found, thus distinguishing it a solitary ganglioneuroma of the base of tongue.
Scanner view showing good circumscription of the lesion with overlying hyperplastic epithelium. (H&E stain, 40X) Inset: Ganglion cells clustered and interspersed in schwannian stroma. (H&E stain, 400X)
Immunohistochemistry- S-100 protein staining schwannian stroma. (Immunohistochemistry: Avidin-biotin method with DAB chromogen and hematoxylin counterstain, 100X). Inset: Immunohistochemistry – NSE staining the ganglion cell. (Immunohistochemistry: Avidin-biotin method with DAB chromogen and hematoxylin counterstain, 400X)
Discussion
Ganglioneuromas are rare benign neoplasms which are composed of mature autonomic ganglion cells and most of them arise at sites at which sympathetic ganglia are found, particularly in mediastinum, retroperitoneum, and pelvis [1]. Approximately 45% are thoracic, 35% are abdominal, and 20% are adrenal in location. Visceral involvement by a ganglioneuromatous process may be diffuse or localized. Rarely, have ganglioneuromas been observed in the tongue, prostate, skin, bone, spermatic cord, heart, and intestine [2,3]. Ganglioneuromas mainly occur in patients who are younger than 10 years of age, but they are also seen in adults [1]. A majority of symptoms are associated with mass effects, as it was in our case, but an endocrine function is known to occur in association with ganglioneuromas [1]. Ganglioneuromas are circumscribed and they appear to be encapsulated. Histologically, they consist of ganglion cells, axonal processes in large numbers, satellite cells and Schwann sheaths. Myelinization is absent. An immature ganglioneuroma, a distinctive variant, is characterized by a broad range of ganglion cell maturation, absence of or only rare neuroblasts, and often, abundant swaths of axonal processes which are unassociated with Schwann cells [1]. The International Neuroblastoma Pathology Classification has adopted a prognostic system which was modeled on one which was proposed by Shimada et al., [4] It is an age-linked classification dependent on the differentiation grade of the neuroblasts, their cellular turnover index, and the presence or absence of a Schwannian stromal development. Based on morphologic criteria which have been defined in this article, NTs were classified into four categories and their subtypes: 1) neuroblastoma (Schwannian stroma-poor): Undifferentiated type, Poorly differentiated type, and Differentiating type; 2) Ganglioneuroblastoma: Intermixed (Schwannian stroma-rich); 3) Ganglioneuroblastoma: Nodular (composite Schwannian stroma-rich/stroma-dominant and stroma-poor) and 4) ganglioneuroma (Schwannian stroma-dominant): Maturing and Mature. Specific features, such as the mitosis-karyorrhexis index, the mitotic rate, and calcification, were also included, to allow the prognostic significance of the classification which had to be tested [5].
Oropharynx, as a site of involvement, has not been noticed before and it does not mimic a malignancy, as was seen in our case. Interestingly, our patient was old, who presented with a submucosal nodular lesion at a site, which was a common differential diagnosis of a polypoidal lesion at this site, more so in India, where oropharyngeal carcinomas are common in male patients with histories of tobacco chewing.
Tongue is a common site for trauma which is caused by irregular dentures, pressure, previous surgical procedures and ischaemia; hence, traumatic neuromas are frequently observed at this site. They usually present as firm, tender nodules. Microscopically, they consist of a haphazard proliferation of nerve fascicles, which include axons, Schwann cells, and fibroblasts which are embedded in a background of collagen, and are sometimes associated with chronic inflammation [6]. Mature ganglion cells which represent the involvement of a pre-existing ganglion or involvement of a ganglionized nerve fibre can also be present, in which case, this lesion was termed as a pseudoganglioneuroma. The key differentiating features rely on the definite capsule, random distribution and multinucleation of ganglion cells in a true ganglioneuroma [7], as was seen in our case.
Ganglioneuroblastomas occur in infants and young children and histologically, they contain primitive neuroblasts, along with mature ganglion cells [2]. Subepithelial nerve plexuses also have similar histological appearances, with aggregates of nerve plexuses and ganglion cells, but these are usually seen in the lateral border of tongue, which clinically present as erythematous patches or ulcers. Microscopically, they have very few ganglion cells and are of extremely small sizes [7].
Deep rooted neurofibromas at this site also need to be considered. These tumours grow persistently, causing expansion and microscopically, the cells are arranged in short fascicles and whorls. In some patients with von Recklinghausen’s disease, scattered, solitary, or clustered mature ganglion cells are also observed within a plexiform neurofibroma [7].
Conclusion
We are hereby reporting a case of a ganglioneuroma at an unusual site and with an unusual clinical presentation, which mimicked a malignancy. The presence of neural elements and ganglion cells at this site makes it important for an inexperienced histopathologist to differentiate it from other neural lesions of the tongue, in order to avoid a misdiagnosis. An early and an appropriate recognition of such lesions can prevent the clinicians from administering inappropriate treatments. A thorough awareness on the uncommon neural lesions of the tongue can prevent any misdiagnoses and it can easily solve such diagnostic challenges.
[1]. Scheithauer BW, Woodruff JM, Spinner RJ, Peripheral Nerve Sheath Tumors. In: Perry A, Brat DJ editorsPractical surgical neuropathology a diagnostic approach 2010 1st editionPhiladelphiaChurchill Livingstone:269-71. [Google Scholar]
[2]. Kim SK, Jeong MY, Kang HK, Yoon W, Diffusion-Weighted Magnetic Resonance Imaging Findings in a Patient with Trigeminal GanglioneuromaKorean J Radiol 2013 14:118-21. [Google Scholar]
[3]. Lonergan GJ, Schwab CM, Suarez ES, Carlson CL, Neuroblastoma, ganglioneuroblastoma, and ganglioneuroma: radiologic-pathologic correlationRadiographics 2002 22:911-34. [Google Scholar]
[4]. Shimada H, Ambros IM, Dehner LP, Hata J, Joshi VV, Roald B, The International Neuroblastoma Pathology Classification (the Shimada system)Cancer 1999 86:364-72. [Google Scholar]
[5]. Shimada H, Ambros IM, Dehner LP, Hata J, Joshi VV, Roald B, Terminology and morphologic criteria of neuroblastic tumors: recommendations by the International Neuroblastoma Pathology CommitteeCancer 1999 86:349-63. [Google Scholar]
[6]. Vora AR, Loescher AR, Craig GT, Boissonade FM, Robinson PP, A light microscopical study on the structure of traumatic neuromas of the human lingual nerveOral surg oral Med Oral Pathol Oral Radiol Endod 2005 99(4):395-403. [Google Scholar]
[7]. Daneshvar A, Pharyngeal traumatic neuromas and traumatic neuromas with mature ganglion cells (pseudoganglioneuromas)Am J Surg Pathol 1990 14(6):565-70. [Google Scholar]