Neoplastic (solid) Calcifying Ghost Cell Tumor, Intraosseous Variant: Report of A Rare Case and Review of Literature
Jyotsna Wader1, Neha Gajbi2
1 Associate Professor, Department of Pathology, Krishna Institute of Medical Sciences, Karad, Maharashtra, India.
2 PG Resident, Department of Pathology, Krishna Institute of Medical Sciences, Karad, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORESPONDING AUTHOR: Dr. Neha Gajbi, PG Resident, Department of Pathology, Krishna Institute of Medical Sciences, Karad, Maharashtra, India.
Phone: 9404215297,
E-mail: dr.komalgajbi@gmail.com
A neoplastic (solid), calcifying ghost cell tumour is a rare subtype of Calcifying Odontogenic Cyst. The most important features of this pathologic entity are histopathological features, which include a proliferating cystic lining which demonstrates characteristic “Ghost” epithelial cells which have a propensity to calcify. We are reporting a case of a 61–year–old male with a painful swelling in the lower right jaw. Radiology showed a bilocular, well circumscribed, radiolucent lesion in the mandible, which measured 2x1 cm, with radiopaque structures within it. Tooth extraction was done, with enucleation of the lesion, which histopathologically revealed features of a solid, calcifying ghost cell tumour, with an intraosseous variant. The case has been presented, with a brief review of literature.
Neoplastic (solid) Calcifying Ghost Cell Tumor, Intraosseous Variant
Introduction
A calcifying odontogenic cyst is a heterogeneous group of lesions which exist either as cystic or a solid variant and is a relatively uncommon odontogenic lesion which is characterised by varied clinical and radiographical features and biological behaviours [1]. Some of the cysts represent non–neoplastic cysts, while some others with solid components are regarded as neoplasms. They are variously designated as dentinogenic ghost cell tumours or epithelial odontogenic ghost cell tumours. A neoplastic (solid), calcifying, odontogenic cyst is rare and less commonly, such cysts are multilocular.
Case Report
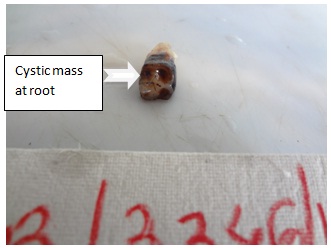
A 61–year–old male presented with a painful swelling in the lower right jaw. On evaluation, asymmetry of lower right and left sides was observed, along with cervical lymphadenopathy. Radiology showed a bilocular, well circumscribed, radiolucent lesion, with a key feature of radiopacities within the lesion, which corresponded to mineralisation within the ghost cells. Tooth extraction was done, with enucleation of the lesion, which was in agreement with the principle of clinically treating small cystic lesions of jaw. Specimen which was sent to pathology department consisted of a tooth with a mass at the root, which measured 2x1 cm, cut section of which revealed partly solid and partly cystic appearances.
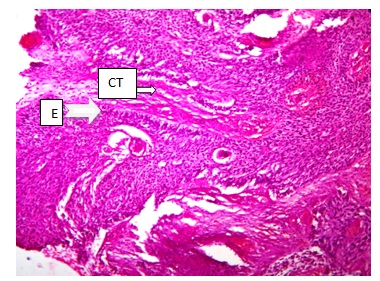
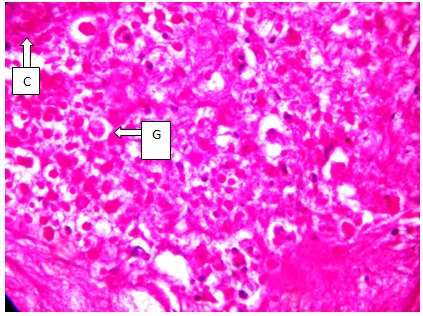
Microscopically, it revealed a tumour which consisted of ameloblastoma like strands and islands of proliferating odontogenic epithelium in a mature connective tissue stroma. Some of the cells within the proliferating epithelium revealed ghost cell keratinization. In some areas, focal calcification was seen. Diagnosis of a neoplastic (solid), calcifying ghost cell tumour with an intraosseous variant was made [Table/Fig-1, 2 and 3].
Gross photo of the tooth with cystic mass at the root
(H&E stained, 100X) - solid tumor consisting of ameloblastoma like strands and islands of proliferating odontogenic epithelium (E) in a mature connective tissue(CT) stroma
(H&E stained, 400X) - solid tumor consisting of ghost cell keratinisation(G) and focal calcification(C)
Discussion
Calcifying Odontogenic Cysts (COCs) account for 0.37% to 2.1% of all odontogenic tumours and neoplastic subtype is seen in 2% to 16% of COCs. A calcifying odontogenic cyst is an uncommon lesion that demonstrates considerable histopathologic diversity and variable clinical behaviours. Many variants have been noted and a proper categorisation of the cases is needed, for a better understanding of the pathogenesis of each variant.
Epithelial-lined cysts rarely occur in skeletal bones, because embryonic epithelial rests are normally not found in them. However, they may occur in the jaws where the majorities are lined by epithelium which is derived from remnants of the odontogenic apparatus [2].
In 1992, the World Health Organization (WHO) classified a calcifying odontogenic cyst as a neoplasm rather than a cyst, but it confirmed that most of the cases were nonneoplastic, with very few being of neoplastic variety, as was our case. Initially, Gorlin et al., and Gold described these as keratinizing and calcifying odontogenic cysts. Kurt Thoma and Henry Goldman considered the lesions to be odontogenic tumours of ectodermal and mesodermal origin. Other names which were suggested were ‘calcifying ghost cell odontogenic tumour’ by Fejerskow and Krogh and ‘cystic calcifying odontogenic tumour’ by Freedman and his associates. ‘Dentinogenic ghost cell tumour’ is another name which is used, but dentine formation is unusual and the name implies a mesenchymal rather than an epithelial neoplasm [3, 4].
These clinically more aggressive lesions seem to occur more commonly in the mandibles of men. They present in an older but still overlapping age group than their cystic counterparts, usually in those who are over 50 years. The intraosseous variant presents as an asymptomatic, hard swelling of the jaw, that produces an expansion than an erosion of bone. Pain indicates a secondary infection. Our patient had a painful swelling which was accompanied by lymphadenopathy, which was suggestive of a secondary infection.The cysts are usually discovered as an incidental radiographic finding. Early in their development, they will appear to be completely radiolucent. As they mature, they develop calcifications that produce a well-circumscribed, mixed radiolucent-radiopaque appearance.
In our case report, radiology showed a bilocular, well circumscribed radiolucency with radiopaque structures within it. The intra and extraosseous extent of lesions are accurately determined by radiologic studies. The definitive diagnosis is usually made histopathologically, due to the lesion’s lack of characteristic clinical and radiological features, as well as its variable biological behaviour.
Presence of ghost cells within the proliferative odontogenic epithelium is an essential characteristic for the diagnosis. Ghost cell keritinisation alone may be observed in odontomas and it may be associated with other odontogenic tumours such as adenomatoid odontogenic tumours, ameloblastic fibro-odontomas, ameloblastic fibromas, and ameloblastomas. The histopathological features of a calcifying odontogenic cyst are characteristic of the condition.
The treatment of a cystic lesion involves a surgical excision [5] with a long-term follow up. Recurrence depends on completeness of cyst removal. Prognosis is less certain for neoplastic lesions [2]. It may be associated with other odontogenic tumours, where the treatment and prognosis of such cases are based on the associated tumours.
Conclusion
We reported the case because of its rare occurrence. A proper categorisation as a ‘neoplastic (solid) subtype’ of a calcifying odontogenic cyst is based on histopathological features and it is needed for a better understanding of the pathogenesis and biology of the lesion.
[1]. Thinakaran Meera, Calcifying ghost cell odontogenic cystA review on terminologies and classifications 2012 16(3):450-53. [Google Scholar]
[2]. Sonone Archana, Calcifying Ghost Cell Odontogenic CystCase Reports in Dentistry 2011 10:5 [Google Scholar]
[3]. Tomich CE, Calcifying odontogenic cyst and dentinogenic ghost cell tumorOral and Maxillofacial Surgery Clinics of North America 2004 16(3):391-397. [Google Scholar]
[4]. Bouquot Neville Damm Allen, Oral and Maxillofacial Pathology 2004 2nd edition:604-07., chap 4 [Google Scholar]
[5]. Shafer’s Textbook of Oral Pathology, Cysts and Tumors of Odontogenic Origin 2006 5th edition:380-400.chap. 4, [Google Scholar]