To analyse the clinical presentation, operative findings, surgical procedures, post–operative complications, morbidity and mortality associated with intestinal perforation due to typhoid fever in a tertiary care center and to study changing trends in mortality in typhoid intestinal perforation.
Material and Methods
This study included 40 patients, diagnosed with typhoid intestinal perforation admitted and treated in the Department of General Surgery from February 2011 to January 2012. Retrospectively the cases were analyzed by reviewing the patient records after approval from the ethical committee. The cases were evaluated with regard to age, gender, clinical features, investigations, intra–operative findings, type of surgery, morbidity and mortality. All patients initially presented to the emergency department because of acute abdomen. They were subjected to erect X–ray abdomen, chest X–ray PA view, complete blood count, urine analysis, renal function test, serum electrolytes, ultrasound abdomen. All patients underwent surgery after pre–operative resuscitation within 6 hours of admission. All were given 3rd generation Cephalosporins (preferably Ceftriaxone) with Metronidazole, with or without Amikacin.
Statistical Analysis
Descriptive statistics comprising of percentage (proportion) and mean (± standard deviation) were used to describe the patient characteristics and morbidity/mortality profile.
Results
Out of the 40 patients, 32 (80%) were male. The youngest was 14 years old and oldest was 65 years with mean age of 35.75 years.
Twenty three (57.5%) patients presented with intestinal perforation within seven days of onset of fever [Table/Fig-1]. The most common presentation was pain abdomen seen in 38 patients with mean duration of 2.95 days. Twenty one patients had history of pain abdomen less than 2 days. Bowel disturbances were present in seventeen (42.5%) patients, Out of whom 8 patients had constipation, 7 patients had loose stools and 2 patients had vomiting. Comorbidities were also present in two patients. One patient had hypertension and another patient had diabetes. Eleven patients were diagnosed to have typhoid fever and received antibiotics prior to hospitalisation for perforation.
Distribution of duration of fever of patients studied
| Duration of fever (days) | Number of patients | % |
|---|
| Nil | 4 | 10.0 |
| <7 | 23 | 57.5 |
| 7-14 | 3 | 7.5 |
| 14-21 | 7 | 17.5 |
| >21 | 3 | 7.5 |
| Total | 40 | 100.0 |
(Mean ± SD: 8.46±7.76)
On examination 30 (75%) patients had diffuse peritonitis, eight (20%) patients had localised peritonitis whereas 2 (5%) patients had no peritonitis. Twenty three (57.5%) patients had leukocytosis (>11000cells/cumm), and only one patient had leukocyte count less than 4000cells/cumm. Neutrophils were more than 80% in 24 (60%) patients. A simple erect chest X–ray demonstrated gas under diaphragm in 34 (85%) patients. Remaining patients were subjected to ultrasound/CT scan for diagnosis.
All the patients underwent midline laparotomy. Single perforation of ileum was noted in 31(77.5%) patients, 5(12.5%) patients had 2 perforations and more than 2 perforations were present in 4(10%). Size of perforation varied from 0.5cm to 2cm. Location of perforation was within 20cm from ileocaecal junction in 29(72.5%) patients, 20–40cm from ileocaecal junction in 9(22.5%) patients and 2(5%) patients had perforation beyond 40cm from ileocaecal junction. Peritoneal collection was purulent in 20(50%) patients, feculent in 13(32.5%) patients and bile stained in 5(12.5%) patients. Length of inflamed bowel was less than 20cm from ileocaecal junction in 31(77.5%) patients, 20–40cm in 6(15%) patients and 3(7.5%) patients had bowel inflammation more than 40cm from ileocaecal junction.
The choice of surgical procedure was depended on patient’s general condition, peritoneal contamination, inflamed bowel, location and number of perforation. Primary closure of perforation was done in 30(75%) patients out of 31 patients with single perforation. One patient with single perforation had extensive bowel inflammation and feculent collection underwent resection anastomosis and ileostomy. Eight patients who had 2 and more perforations underwent resection and anastomosis with loop ileostomy. One patient who had multiple perforations at ileocaecal junction underwent right hemi colectomy and ileocolic anastomosis.
Post–operative recovery was uneventful in 23(57.5%) patients.Seventeen (42.5%) patients had complications as shown in [Table/Fig-2]. One patient underwent ultrasound guided aspiration for intra–abdominal collection. One patient developed enterocutaneous fistula which was managed conservatively. Three patients required mechanical ventilation in post–operative period. Culture revealed E coli as the main organism in 13 (32.5%) patients [Table/Fig-3], Widal test was positive in 32 (80%) patients. Typhidot was done in 11 patients. It was positive in 7 patients.
Distribution of post-operative complications in patients studied
| Complications | Number of patients (n=40) | % |
|---|
| Nil | 23 | 57.5 |
| Present | 17 | 42.5 |
| • Surgical site infections | 9 | 22.5 |
| • Chest complication | 6 | 15.0 |
| • Enterocutaneous fistula | 1 | 2.5 |
| • Intra-abdominal abscess | 1 | 2.5 |
Distribution of organisms isolated on culture of peritoneal collection
| C/S | Number of patients | % |
|---|
| 1. E coli | 13 | 32.5 |
| 2. Enterococcus | 5 | 12.5 |
| 3. ESBL (E-coli) | 1 | 2.5 |
| 4. Klebsiella | 4 | 10.0 |
| 5. None | 17 | 42.5 |
| Total | 40 | 100.0 |
Thirteen (32.5%) patients were discharged within 10 days. Twenty five (62.5%) patients were discharged between 10 to 30 days and only 2 (5%) patients stayed in the hospital for more than a month.
Discussion
Typhoid perforation usually occurs in 2nd to 3rd week of fever [1,3]. However in developing countries cases are reported early within the first week of illness [5]. In this study duration of fever was less than 7 days in 57.5% of cases. The reason observed behind this though unproven could be because of low immunity, change in the virulence of the bacteria, hypersensitivity of Peyer’s patches to bacteria [1]. The patients who perforated during the first two weeks of the illness appear to have a better prognosis [6]. This may also be because of the compromised nutritional status in patients who had been ill for more than two weeks and perforate.
Typhoid intestinal perforation is seen during the second and third decades of life [3,7]. In this series mean age was 35.75 years.In a study by Atamanalp et al., [8], mean age was 36.3 years and in a study by Sumer et al., [3] mean age was 37 years. It has been found that being male is an independent risk factor for intestinal perforation [9]. Khan et al., reported typhoid perforation more common in males than females [10].
The most common symptoms are pain abdomen and fever [11]. In these series 38 patients presented with pain abdomen. Other features are abdominal distension, constipation, vomiting and loose stools. Guarding has been reported as the most common physical finding [3].
In this study 85% patients had pneumoperitoneum demonstrated on chest X–ray and erect X–ray abdomen. This is consistent with study by Chalya et al., [1]. Leukopenia is the feature of typhoid fever. In our series 57.5% had leucocytosis. 2.5% had leukopenia, rest had normal total leukocyte count. A study by Santillana et al., leucocytosis was recorded in 59.5% of patients [12]. Leucocytosis in typhoid fever suggests increased severity of typhoid perforation [9].
Widal test has been used in developing countries for diagnosing typhoid fever but it has low sensitivity, specificity and positive predictive value which changes with the geographical areas [13]. Typhidot is an immunochromatographic test which is easy and rapid to perform and turn around time is one hour [14]. The gold standard blood culture takes 2 to 4 days. In this study Widal was positive in 32 patients (80%). In a study by Rahman et al., Widal was positive in 75.90% of cases [15]. Typhidot was done in 15 patients and in seven patients it was positive. Five patients who were widal negative showed typhidot positive.
Typhoid perforation mainly affects the terminal 40 cm of the ileum in 72%–78% of cases; the jejunum, caecum, colon and gallbladder to lesser degree [16]. Rare case of appendicular perforation due to typhoid has been reported in literature [17]. In this study 38 patients had perforation in terminal 40 cm of ileum. Only two patients had perforation proximally, at mid ileal level. Pathological changes are not just restricted to perforation sites. The diseased gut is characterised by diffuse non–specific enterocolitis with hypertrophy, necrosis and ulceration of intestinal and mesenteric lymphatic tissue. This is the reason for the gut in patients suffering from typhoid fever, mainly terminal 60 cm to be oedematous and friable [2]. In this study the diseased bowel was less than 20 cm in 31 (77.5%) patients. This may be because our patients had perforation in early course of disease. Once perforation occurs peritoneal contamination depends on duration of perforation and number of perforations. In this study majority (77.5%) had single perforation. It has been reported that multiple perforations have significantly high mortality compared to those with single perforation [1].
Early surgery is the optimal treatment in typhoid perforations despite appropriate antibiotics. It ceases the source of further faecal contamination of peritoneal cavity [18]. In this study surgical intervention was done within 6 hours of admission. Several surgical procedures have been described in the form of simple closure, wedge excision with simple closure of perforation, bowel resection and anastomosis with or without ileostomy. Laparoscopic perforation closure has been reported by Ramachandran et al., [19] and Sinha et al., [20]. In this study primary closure was done in 75% patients. 25% had an extensive procedure. Beniwal et al., [21] suggested primary closure is the choice of treatment. Shah et al., founded resection anastomosis and copious peritoneal lavage is the best surgical option [22]. Malik et al., showed primary ileostomy to be the successful procedure [18]. Husain et al., suggested closure of ileal perforation with omental patch technique prevents the leak [23].
The main organism grown in peritoneal fluid culture was E coli 13 (32.5%) patients. This is consistent with the study by Sitaram et al., [24]. Most common complication in this study was surgical site infection which is similar to a study by Ansari et al., [25]. Enterocutaneous fistula was found in 1 (2.5%) patient similar to study by Sumer et al., [3]. This was managed conservatively. Fistula closed spontaneously. In a study by Ansari et al., fistula was found in 13.4% patients [25] Major cause of post–operative morbidity in perforation peritonitis according to Jhobta et al., is respiratory complication [26]. In this study 6 patients (15%) developed respiratory complication and 3 patients needed mechanical ventilation in the post–operative period.
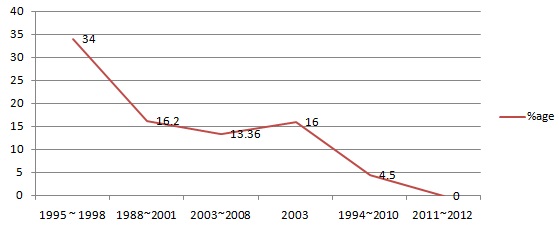
In developing countries mortality rates from typhoid perforation have been reported to range from 9–22%[1].There was no mortality in our series as compared to other studies [Table/Fig-4 and 5]. Agbakwuru et al., who reported mortality rate of 16.2% [27] where in the patients were operated 24 to 48 hours after diagnosis. Ansari et al., reported mortality of 13.36% [25] where the patient presented with mean duration of pain abdomen of 5.6 days. In their study 4 out of 6 deaths were due to development of faecal fistula. In our series, most of our patients (57.5%) presented within the first week of fever and the mean duration of pain abdomen was 2.95 days. Koume et al., reported high mortality due to complications related to ileostomy [28]. Saxe et al., attributes mortality in his study to persistent sepsis which he says could have been prevented by using broad spectrum antibiotics [29]. There was no mortality in our study probably due to early and appropriate surgical intervention, effective pre and peri-operative resuscitation, post-operative intensive care procedures, good ileostomy care and delivery of broad spectrum antibiotics. Sumer et al., reported low mortality attributed to similar reasons [3].
Comparison of mortality in different studies
| Sl No. | Study [References] | Year | No of Patients Studied | Number of Mortality (%) |
|---|
| 1 | Kouame et al., [29] | 1995-1998 | 64 | 22 (34%) |
| 2 | Agbakwuru et al., [27] | 1988-2001 | 105 | 17 (16.2%) |
| 3 | Ansari et al., [25] | 2003-2008 | 44 | 6 (13.36)% |
| 4 | Saxe et al., [29] | 2003 | 112 | 18 (16%) |
| 5 | Sumer et al., [3] | 1994-2010 | 22 | 1 (4.5%) |
| 6 | Our study | 2011-2012 | 40 | nil |
Decline in mortality in typhoid perforation
Conclusion
Typhoid intestinal perforation is a major surgical health problem in tropical countries particularly in those where, standard of living is low which leads to unhygienic environment. Early recognition, timely surgical intervention, appropriate antibiotics and surgical technique and peri–operative care play key role in reducing mortality in typhoid intestinal perforation. However, this is a retrospective observational study. This has all the limitations of retrospective study, to come to any opinion. This warrants a prospective study to come to a definitive conclusion.
(Mean ± SD: 8.46±7.76)