Cholelithiasis is the most common biliary pathology. The incidence of choledocholithiasis in patients with cholelithiasis varies between 5 to 15 percent, out of which 5% are asymptomatic [1]. Although common bile duct (CBD) stones may be silent, the development of complications such as cholangitis and acute pancreatitis is associated with major morbidity and mortality. Therefore, the detection and treatment of common bile duct stones is mandatory.
Usually, the diagnosis of choledocholithiasis is based on a combination of clinical suspicion (biliary colic, jaundice and cholangitis), bio-chemical analysis (raised conjugated bilirubin and alkaline phosphatase levels) and imaging findings. Unfortunately, all of these individually have varying diagnostic accuracies and none is a completely reliable method for identifying bile duct stones [2]. Intra-operative Cholangiography (IOC) is standard procedure during open cholecystectomy which can detect CBD stones with a sensitivity of 98% and a specificity of 100%. It is an invasive investigation with intra-operative and post-operative morbidities of 6.3 % and 15.9% respectively. Its routine use is associated with increased costs and increased operating times [3].
Endoscopic Retrograde Cholangio-Pancreatography (ERCP) is able to detect common bile duct stones with high accuracy in patients with suspected stones [1]. ERCP can be applied both as a diagnostic and a therapeutic tool. It also allows direct visualisation of duct anatomy. However, ERCP has a significant mortality and morbidity of 1% and 7%, respectively [1]. A ductal cannulation is difficult or impossible in patients who had undergone previous surgeries, which include a Billroth Type-II gastrectomy and a hepatico-enterostomy.
In many institutions, Magnetic Resonance Cholangio–Pancreatography (MRCP) is replacing ERCP as a diagnostic procedure in the investigation of benign biliary obstructions and chronic pancreatitis. MRCP has an advantage because of its technical versatility, multiplanar capability and superior soft tissue resolution. Unlike ERCP, MRCP is non-invasive, it can be performed rapidly and it does not expose the patients to ionised radiations or iodinated contrast material. The present study was conducted to evaluate the role of MRCP in detection of CBD stones in patients with suspected choledocholithiasis.
Material and Methods
This prospective study was conducted on 30 patients, from July 2006 to January 2009, after obtaining permission from the institutional ethics committee. Informed consents for the study were taken from all patients. The procedures were in accordance with the guidelines of Ethical Committee on Human Experimentation of the institution in which the study was done, which were in accordance with the guidelines of Helsinki Declaration of 1975 which were revised in 2008. The study included 30 patients who were suspected of having choledocholithiasis on the basis of any of the following criteria:-
1. A history or presence of any of the following:
Intermittent jaundice Cholangitis which was defined as the presence of fever (> 37.30C), chills, colicky right upper quadrant pain and leucocytosis.
Status of post biliary pancreatitis which was defined according to a history of biliary pancreatitis of not more than 2 months duration prior to admission, with subsided pancreatitis at the time of admission.
Post cholecystectomy syndrome.
2. Total bilirubin which was > 1.2 mg / dL
ALP which was > 220 IU/L
3. A CBD diameter of > 7 mm at sonography or CBD stones which were suspected / diagnosed at sonography.
All cases of obstructive jaundice where the cause proved to be other than CBD stones (e.g. carcinoma head of pancreas, periampullary carcinoma, CBD strictures, cholangiocarcinoma, etc.) were excluded from the study.
The patients were initially evaluated by taking their detailed histories, by doing thorough physical examinations, by checking complete blood counts and by doing liver function tests. Ultrasound was done on GE RT 3200/Toshiba core-vision pro-diagnostic ultrasound system SSA -350 machine with a transducer of 3.5 MHz or 5 MHz frequency. Study was done after the patients had undergone an overnight fast for 8 to 12 hours. Scans were done in longitudinal, transverse and oblique planes.
MRCP was performed for all patients on a 1.5-Tesla Magnetom Avanto system (Siemens, Erlangen, Germany). The patients fasted for 6 hours before MRCP. All patients were imaged with a body phased-array receive coil. 5 mm thick sections were taken from right dome of diaphragm to lower edge of liver. Following are the sequences which were used after the localiser: T2 HASTE AXIAL free breath, T2 HASTE FS AXIAL free breath, T1 FLASH AXIAL breath hold, T2 HASTE CORONAL free breath, 3D MRCP free breath (PACE), Single shot HASTE MRCP and single shot HASTE different angle. A 3D reconstruction was performed by MIP post processing. MIP image and thick angled coronal sections provided views of pancreatico - biliary tree which were similar to those which were seen on conventional ERCP.
All cases with choledocholithiasis which were suspected on clinical evaluation or during biochemical or radiological investigations were subjected to open surgeries. All patients with dilated CBDs of sizes of more than 7 mm (which were measured by vernier callipers) or with palpable CBD stones underwent CBD explorations. Demonstration of CBD stones intra-operatively was considered the ‘gold standard’ for detecting their presence, which included visualization, extraction or an attempt which was made towards extraction of stones during surgical CBD explorations.
All patient data was prospectively collected and it was entered into a database. Radiographic studies were interpreted by a radiologist. All patients were followed up for their complications and outcomes.
Results
This study included 30 patients with clinical, biochemical or radiological suspicions of choledocholithiasis. Their ages ranged from 25 years to 80 years, with a mean age of 54 years. A majority of the patients (63.3%) were above 50 years of age. Out of 30 patients, 17 (56.67%) were females and 13 (43.33%) were males. The female to male ratio was 1.3:1 [Table/Fig-1].
Age-Sex distribution of study population
| Age(Years) | Male | Female | Total |
|---|
| <30 | 2 | 3 | 5 |
| 30-50 | 2 | 4 | 6 |
| >50 | 9 | 10 | 19 |
| Total | 13 | 17 | 30 |
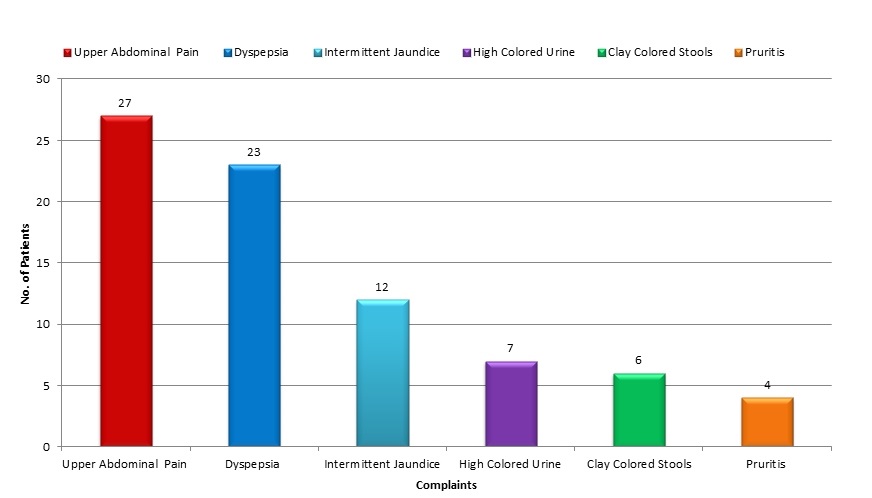
The most common presenting complaint was upper abdominal pain, which was present in 27(90%) patients. The next common complaint was dyspepsia which was present in 23 (76.67%) patients. 12 (40%) patients had complaints of intermittent jaundice and highly coloured urine. 7 (23.33%) patients complained of clay coloured stools and 6 (20%) patients had pruritis. Fever with chills were present in only 4 (13.33%) patients [Table/Fig-2]. 3 (10%) patients had a past history of cholecystectomy. 6(20%) patients had a past history of cholangitis. Presenting complaint of jaundice had a sensitivity, specificity and positive and negative predictive values of 45%, 70%, 75% and 38.89% respectively in the diagnosis of CBD stones.
Chief complaints in the study population
The total leukocyte count (TLC) was raised in 7(23.33%) out of 30 patients and it ranged from 11000 to 14950/mm3. The most common biochemical abnormality was a raised serum alkaline phosphatase level, which was raised in 22 (73.33%) patients and it ranged from 235 to 2291 IU/L. Total serum bilirubin was elevated in 10(33.33%) patients, which ranged from 4.6 to 17.2 mg%. Serum ALT and AST were elevated in 16 (53.33%) and 18(60%) patients respectively and serum amylase was raised in only 3(10%) patients [Table/Fig-3].
The Pattern of Biochemical Abnormalities
| Biochemical Parameters (Normal Range) | No. of Patients with Abnormal Values of Biochemical Parameters (Range) | Percent (n=30) |
|---|
| TLC (4000-11000/mm3) | 7(11000-14950) | 23.33 |
| Serum Bilirubin (0.1-1.2 mg%) | 10(4.6-17.2) | 33.33 |
| Serum ALP (20-230 IU/L) | 22(235-2291) | 73.33 |
| Serum ALT (10-43 IU/L) | 16(46-232) | 53.33 |
| Serum AST (10-36 IU/L) | 18(40-247) | 60 |
| Serum Amylase (0-175 IU/L) | 3(199-589) | 10 |
On ultrasonography, cholelithiasis was diagnosed in 19 (63.3%) patients and choledocholithiasis was diagnosed in 13 (43.3%) patients. USG showed dilated CBD stones (> 7 mm) in 23 (76.7%) patients [Table/Fig-3]. MRCP diagnosed cholelithiasis in 20 (66.7%) patients and choledocholithiasis in 19 (63.3%) patients. Dilated CBD stones were diagnosed in 25 (83.3%) patients [Table/Fig-4].
Percentage of Cholelithiasis and Choledolithiasis in Ultrasound and MRCP in the Study Population
| Investigations | Normal n(%) | Cholelithiasis n(%) | Choledocholithiasis n(%) | Dilated CBD n(%) |
|---|
| Ultrasound |
| Male | 3 | 7 | 5 | 10 |
| Female | 4 | 12 | 8 | 13 |
| Total | 7 (23.3%) | 19 (63.3%) | 13 (43.3%) | 23 (76.7%) |
| Mrcp |
| Male | 2 | 8 | 8 | 11 |
| Female | 3 | 12 | 11 | 14 |
| Total | 5 (16.7%) | 20 (66.7%) | 19 (63.3%) | 25 (83.3%) |
Intra-operatively, 21 (70%) out of 30 patients had cholelithiasis. 26 (86.7%) out of 30 patients had dilated CBD stones intra–operatively. In 20 (66.7%) out of 30 patients, choledocholithiasis was detected intra-operatively [Table/Fig-5]. Cholelithiasis and choledocholithiasis were most commonly seen in patients who were above 50 years of age [Table/Fig-6]. The most commonly performed operative procedure in these 20 patients was cholecystectomy with choledocholithotomy, with a T tube drainage, which was performed in 14 patients. In 3 patients, cholecystectomy with choledochoduodenostomy was performed due to the presence of multiple small calculi. In 3 post-cholecystectomy patients with choledocholithiasis, 2 underwent choledochoduodenostomies for multiple small calculi and 1 patient underwent a choledocholithotomy with primary closure. In the remaining 10 patients without choledocholithiasis, CBD explorations were performed in all, due to presence of dilated CBD stones intra-operatively. All these 10 patients underwent cholecystectomy with choledochotomy, with a T tube drainage or a primary closure.
| Age | Normal n(%) | Cholelithiasis n(%) | Choledocholithiasis n(%) | Dilated CBD n(%) |
|---|
| <30 | 1 | 3 | 2 | 4 |
| 30-50 | 1 | 3 | 3 | 5 |
| >50 | 2 | 15 | 15 | 17 |
| Total | 4 (13.3%) | 21 (70%) | 20 (66.7%) | 26 (86.7%) |
Correlation of clinical, biochemical, and imaging findings with intraoperative findings
| Clinical features and Investigations | Intraoperative findings (N = Total number of patients with positive intraoperative findings) |
|---|
| Cholelithiasis Number of patients (%) | Choledocholithiasis Number of patients (%) | Dilated CBD Number of patients (%) |
|---|
| Clinical features |
| Pain | 20 (95.2%) | 17 (85%) | 24 (92.3%) |
| Jaundice | 4 (19.1%) | 9 (45%) | 11 (42.3%) |
| Biochemical |
| Serum alkaline phosphatase >220 IU/L | 12 (57.2%) | 13 (65%) | 19 (73.1%) |
| Imaging |
| USG | 19 (90.5%) | 13 (65%) | 23 (88.5%) |
| MRCP | 20 (95.2%) | 19 (95%) | 25 (96.1%) |
The correlation between various clinical, biochemical and imaging findings and intra-operative findings was studied and recorded. [Table/Fig-7]. Among the 20 patients with choledocholithiasis, 9(45%) patients presented with a history of jaundice and 17(85%) presented with a history of upper abdominal pain. Serum alkaline phosphatase had the highest sensitivity (65%) in the diagnosis of choledocholithiasis among the biochemical parameters which were studied. Ultrasonography could diagnose choledocholithiasis in 13 (65%) out of 20 patients with choledocholithiasis. MRCP demonstrated CBD stones in 19 (95%) out of 20 patients who were found to have choledocholithiasis intraoperatively [Table/Fig-7].
USG abdomen showing dilated CBD (black arrow), measuring 16.4 mm with single echogenic focus at its lower end (colored arrow)
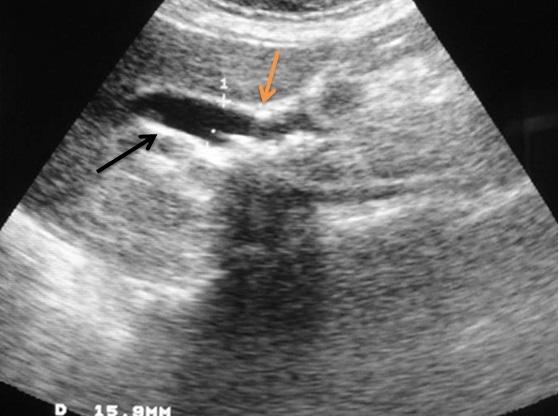
Ultrasonography could diagnose choledocholithiasis in only 13(65%) out of 20 patients with choledocholithiasis, which was found per operatively, giving a sensitivity of 65% [Table/Fig-8]. USG correctly diagnosed absence of choledocholithiasis in 6 out of 10 patients, i.e. the specificity of USG for choledocholithiasis in the present study was 60%. The positive predictive value of USG in detection of choledocholithiasis in the present study was 76.47% and negative predictive value was 46.15% [Table/Fig-8]. MRCP diagnosed choledocholithiasis in 19(95%) out of 20 patients with a sensitivity of 95% [Table/Fig-9]. MRCP correctly diagnosed absence of choledocholithiasis in 9 out of 10 patients without choledocholithiasis. The specificity of MRCP in diagnosing choledocholithiasis in the present study was 90%. The positive predictive value of MRCP in diagnosing choledocholithiasis in the present study was 95% and negative predictive value was 90%. [Table/Fig-8].
Sensitivity, specificity, and predictive values for MRCP and USG in the detection of choledocholithiasis
| Imaging tests of choledocholithiasis | Intraoperative choledocholithiasis |
|---|
| MRCP | Present | Absent | Total |
|---|
| Present | 19 | 1 | 20 |
| Absent | 1 | 9 | 10 |
| Total | 20 | 10 | 30 |
| Ultrasound |
| Present | 13 | 4 | 17 |
| Absent | 7 | 6 | 13 |
| Total | 20 | 10 | 30 |
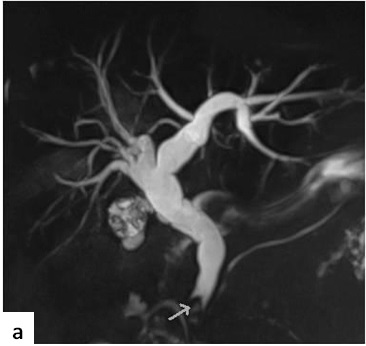
Coronal MRCP projectional image showing dilated IHBR and CBD till lower end with a meniscus sign in its distal end suggestive of choledocholithiasis,
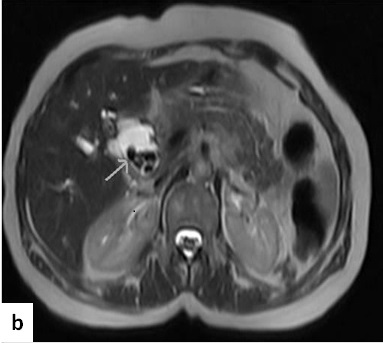
Axial HASTE MRCP image, showing dilated CBD with multiple signal voids within it, suggestive of choledocholithiasis
Discussion
Although MRCP has been shown to provide an accurate diagnosis of CBD stones, only a few investigators have evaluated the utility of MRCP in the preoperative evaluation of symptomatic gallstones and accordingly, the precise role of MRCP in this regards has yet to be determined. Some authors have recommended MRCP for patients with a moderate risk of CBD stones and they have recommended ERCP before any other imaging examination for patients who are at high risk [4, 5], while others have recommended MRCP for patients with a high or moderate risk for CBD stones and they have recommended ERCP for patients in whom stones had been depicted by other imaging modalities [6].
In our study, all the clinical predictors of CBD stones individually had varying diagnostic accuracies and none was completely reliable in identifying bile duct stones [Table/Fig-7]. An age of above 50 years, as a predictor of choledocholithiasis, had a sensitivity, specificity and positive and negative predictive values of 55%, 80%, 84.62% and 47.06% respectively in predicting CBD stones. Female sex as a predictor of choledocholithiasis, had a sensitivity, specificity and positive and negative predictive values of 60%, 50%, 70.59% and 38.46% respectively. In part, this lack of accuracy may have stemmed from the inability in forecasting the rates at which gallstones passed from the gallbladder and poor understanding on how long stones resided in the CBD and on how they passed from the CBD into the duodenum, either with or without symptoms or other evidences of cholestasis. The natural history of CBD stones is still largely unknown [7].
Serum alkaline phosphatase had the highest sensitivity (65%) in the diagnosis of choledocholithiasis among the biochemical parameters which were studied. It had a specificity and positive and negative predictive values of 40%, 59.9% and 42.5% respectively. Total bilirubin had the highest specificity of 70% among the biochemical parameters which were studied. The sensitivity and positive and negative predictive values of total bilirubin were 35%, 70% and 35% respectively Hepato-biliary alkaline phosphatase is secreted by biliary ductular epithelium. The increased serum levels which are found in acute biliary obstruction result from back diffusion [8]. Literature suggests that high serum levels of this enzyme more accurately predict the likelihood of choledocholithiasis, while at the same time, it has also been reported that elevated serum bilirubin was more significant.
In the study which was conducted by Saltzstein et al., alkaline phosphatase was found to be a better indicator of common duct stones than bilirubin and the authors reported that higher the level of alkaline phosphatase, greater was its predictive value [9]. In the study of JC Pereira-Lima et al., alkaline phosphatase had a sensitivity of 74.7%, total bilirubin had a sensitivity of 73.6% and the least sensitive biochemical parameter was aspartate aminotransferase (AST) [10]. In a study which was done by Yang et al., alkaline phosphatase had a higher sensitivity than total bilirubin, total bilirubin had the highest specificity (87.5%) and both alkaline phosphatase and total bilirubin were found to be independent predictors of CBD stones [11].
Ultrasonography is the initial imaging test which is used in the evaluation of patients with suspected bile duct stones. The sensitivity of trans-abdominal ultrasound in the detection of choledocholithiasis is operator dependent and it varies between 20 and 80% [12–15]. The stone detection rate is also influenced by patient factors such as the number, size and site of stones, patient’s body habitus and presence of overlying bowel gas. The sensitivity, specificity and positive and negative predictive values of ultrasonography in detecting CBD stones in the present study were 65%, 60%, 76.47% and 46.15% respectively.
Two possible explanations account for the comparative poor detection of common bile duct stones by ultrasound. First, in both dilated and non–dilated ducts, the distal area of the common bile duct, where impacted stones usually lie, is often obscured by overlying gas from the duodenum or colon. Occasionally, in dilated ducts, one can still visualise the stone by placing the patient in the Trendelenburg position and by observing the stone floating cephalad towards the liver. Secondly, the lack of bile pools in the dilated and non-dilated distal ducts preludes detection of obstructing stone. This situation is compounded with a non-dilated system. In fact, it is probable that the stone that was detected sonographically in a dilated system was not the stone that was obstructing the distal duct, but that it was a more proximal stone [12].
MRCP has recently been developed as a non-invasive but yet a highly sensitive method for diagnosing diseases of the biliary tract. MRCP is usually performed by a radiologist with training in MRCP techniques in a hospital setting. An MRI scanner is needed, with the software which is necessary to perform an MRCP. Such MRI scanners are usually less than 8 years old, although it is possible to upgrade scanners so that MRCPs can be performed. Periodic software upgrades are undertaken on MRI scanners. Some mobile scanning units are able to perform MRCPs. MRCP, like ERCP, is an elective procedure. An MRCP investigation takes approximately 15 minutes of room time, and the sequences take seconds to minutes. The number of MRCP scans which are undertaken may be strongly influenced by the amount of time which is allocated to the MRI scanner to undertake such investigations.
In our study, MRCP had a sensitivity of 95% (19 of 20 patients) in the demonstration of common duct stones and a specificity of 90% (9 of 10 patients). The positive predictive value of MRCP was 95% (19 of 20), whereas the negative predictive value was 90% (9 of 10 patients). There was one false positive and one false negative in the MRCP diagnosis of choledocholithiasis. The cause of the false positive finding on MRCP was mistaking a prominent ampullary sphincter for a lower bile duct stone. The false negative diagnosis had occurred, as multiple, small intrahepatic duct stones were missed out on MRCP. Stones were probably missed because of the lack of contrast between the stones and surrounding liver, with no high signal bile outlining the stones.
Even with current imaging techniques, the accuracy of MRCP in diagnosing CBD stones varies widely. Most of the large series have reported sensitivities which ranged from 81-100%, specificities which ranged from 85-100% and diagnostic accuracies which ranged from 89-100% in the MRCP diagnosis of choledocholithiasis [16–20]. In the studies in which an MR cholangiography was performed with a two-dimensional fast or turbo spin-echo sequence and a standard body coil, the sensitivity of MR cholangiography in the detection of CBD stones was reported to range from 57% to 92%. A previous study in which patients with small stones comprised more than half of the study population, produced the lowest sensitivity (57.7%) in the detection of CBD stones [6]. However, motion artifacts and blurring which are associated with the long acquisition times in the non-breath hold technique which is used would make the detection of small stones difficult and small stones may also move during MRCP when long acquisition times are required. An improved MR cholangiographic performance was achieved by using the breath-hold single-shot half-Fourier sequence with a phased array coil. With this technique, the reported sensitivity was 92%-100% [18]. In the present study, a single-shot half-Fourier sequence and a phased-array coil were used in all patients, and results were similar to those of other studies in which a similar technique was used. Calculi which are missed out on MRCP (MIP images) were most of the times, picked up by the source images and conventional cross sectional imaging, as small filling defects within the bile filled dilated common duct.
The small sample size was one of the limitations of our study. There are several other limitations which are associated with MRCP. Smaller CBD stones can be missed on MRCP [21]. However, usually, stones of sizes of up to 2–3 mm are visible. Papilla can only be seen in about 40% of patients who have MRCP [21]. There may also be a difficulty in depicting minor narrowing of the cystic and pancreatic ducts [22]. Another problem which is associated with MRCP is that maximum intensity projection (MIP) reconstructed images may completely obscure small filling defects and that they may demonstrate respiratory motion artefacts. Source images should always be interrogated, so that in practice, this is not an issue. The major problem with a multislice MRCP (for MIP) is a respiratory misregistration. Another issue is T2 weighting, which may vary with different MRI sequences and influence the findings. It should be noted that MRCP is only a diagnostic procedure. The impact of this is that if an ERCP was necessary afterwards as a therapeutic intervention, an MRCP could have been avoided and patients would have been able to proceed immediately for treatment.
This study shows that MRCP has a diagnostic accuracy which is similar to that of direct cholangiography, in the diagnosis of choledocholithiasis. It provides images which are similar to those of ERCP without the use of a contrast agent or sedation, it is non–invasive, it can be performed rapidly and it avoids the complications which are associated with ERCP.It has the potential to replace ERCP in the diagnosis of bile duct stones. Good quality studies, particularly randomised controlled trials, are needed for comparing MRCP with diagnostic ERCP, which state inclusion/exclusion criteria and relevant patient characteristics. More research is also needed in the area of patient satisfaction and on ways for reducing problems with claustrophobia.
Conclusion
MRCP is an excellent primary tool for detecting or excluding CBD stones before cholecystectomy. In the present study, use of MRCP permitted a purely non-invasive negative diagnosis for 9 (90%) of 10 patients in whom probability of CBD stones was high. Use of MRCP could therefore spare these patients from invasive preoperative endoscopic procedures and it can also most likely reduce overall surgical costs. However, the potential application of MRCP in detection of CBD stones is limited by the expense and availability of technology, due to its high cost and lack of available expertise in operating the machine. We propose MRCP as the method of choice for the diagnostic imaging of bile duct calculi. Ultrasonography should be used as the initial imaging test in the screening of patients with suspected bile duct stones.