Knowledge of the craniovertebral bony abnormalities and their morphology is essential for clinicoradiological studies [1]. Occipitocervical synostosis is one of the most frequent osseous anomalies of craniovertebral junction. Occipitocervical synostosis is defined as a congenital fusion of the atlas to the base of occiput. It was first described by Rokitansky in 1884. Later this anomaly was demonstrated Roentgengraphically by Schuller in 1911 [2,3]. Since then, number of terminologies has been given to it such as occipitalization of atlas, assimilation of atlas, fusion or ankylosis of the atlanto-occipital joint and atlanto-occipital fusion.
The occipitocervical synostosis can be complete or incomplete. The complete synostosis is more common than the partial one. Though it has been rarely reported that multiple variations of partial assimilation may involve any aspect of atlanto-occipital articulation. However, this variation may often go unnoticed but, incidentally found during radiological, operative procedures or during autopsy [3]. It represents the most cephalic ‘blocked’ vertebra encountered in the spine. The most probable cause of the occipitocervical synostosis is a congenital disorder. This condition is due to failure in segmentation and separation of the most caudal occipital sclerotome and first cervical sclerotome during the fourth week of intrauterine life [4].
Understanding the anatomical basis of occipitocervical synostosis is important for surgeons performing craniovertebral region surgeries. Hence the present study was undertaken to determine the incidence and describe the morphology of the occipitocervical synostosis.
Material and Methods
Two-hundred dry adult human skulls of Indian origin of unknown sex were randomly collected from Medical, Dental students and from the Department of Anatomy, M.S. Ramaiah Medical College, Bangalore, Karnataka, India were studied for a period of 2 years from 2010–2012. The skulls which were broken were excluded from the study. The base of skulls was observed for the presence of atlanto-occipital fusion. The skulls which showed atlanto-occipital fusion were studied in detail and their photographs were taken. In these skulls which showed the fusion, the anteroposterior diameter, transverse diameter of foramen magnum and inferior articular facets of atlas were measured using a Tesa Swiss Made digital vernier caliper accurate to 0.01mm. In order to prevent the intra–observer and inter–observer errors, the measurements of each particular diameter was performed by two different observers and the mean of the two taken.
Results
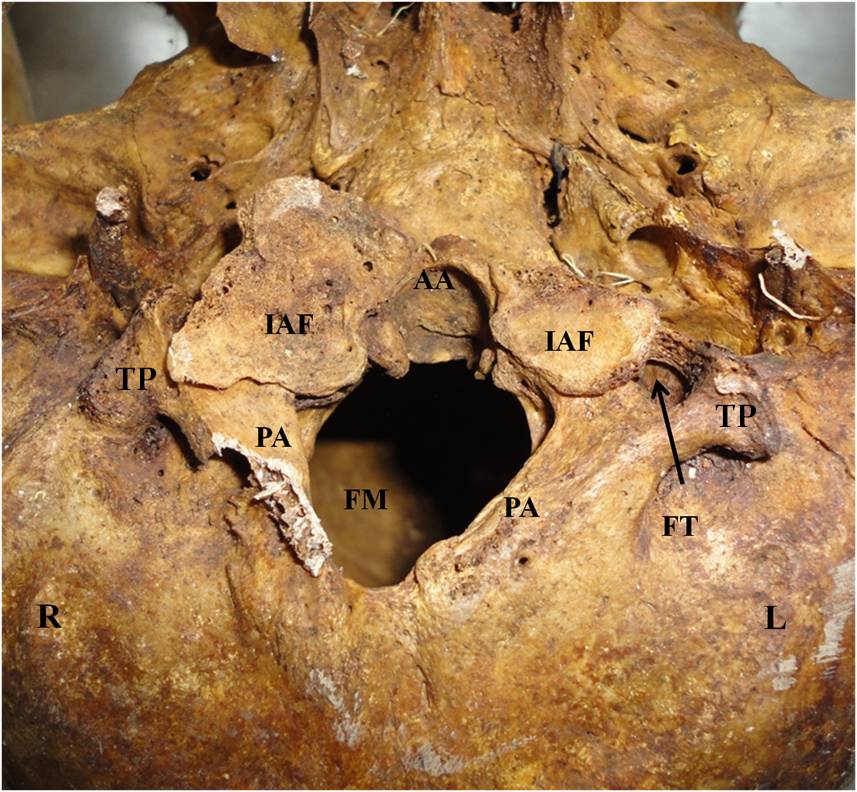
Out of the 200 adult human dry skulls studied, 2(1%) skulls showed occipitalization of atlas. In one skull [Table/Fig-1], the anterior arch, lateral masses and the transverse processes of the atlas were completely fused with the occipital bone. The posterior arch of the atlas was incomplete in the midline, right portion was probably slightly broken on handling and left portion was fused with occipital bone. The Anterior–Posterior Diameter (APD) and the Transverse Diameter (TD) of Foramen magnum were 25mm and 21mm respectively. Foramen magnum was irregular in shape. Both the left and right superior articular facets of the atlas were completely fused with the corresponding occipital condyles while the inferior articular facets of the atlas were asymmetrical. Left inferior articular facet was elliptical in shape; its APD and TD were measuring 21mm and 17mm respectively whereas APD and TD of the Right inferior articular facet were measuring 30mm and 21mm, moreover it was rough and irregular in shape.
Base of the skull with atlanto-occipital synostosis. The right posterior arch of the atlas was broken and left portion was completely fused with occipital bone. R-Right side, L-Left side, IAF-Inferior Articular Facet, PA-Posterior Arch, AA-Anterior Arch, FT-Foramen Transversarium, FM- Foramen Magnum
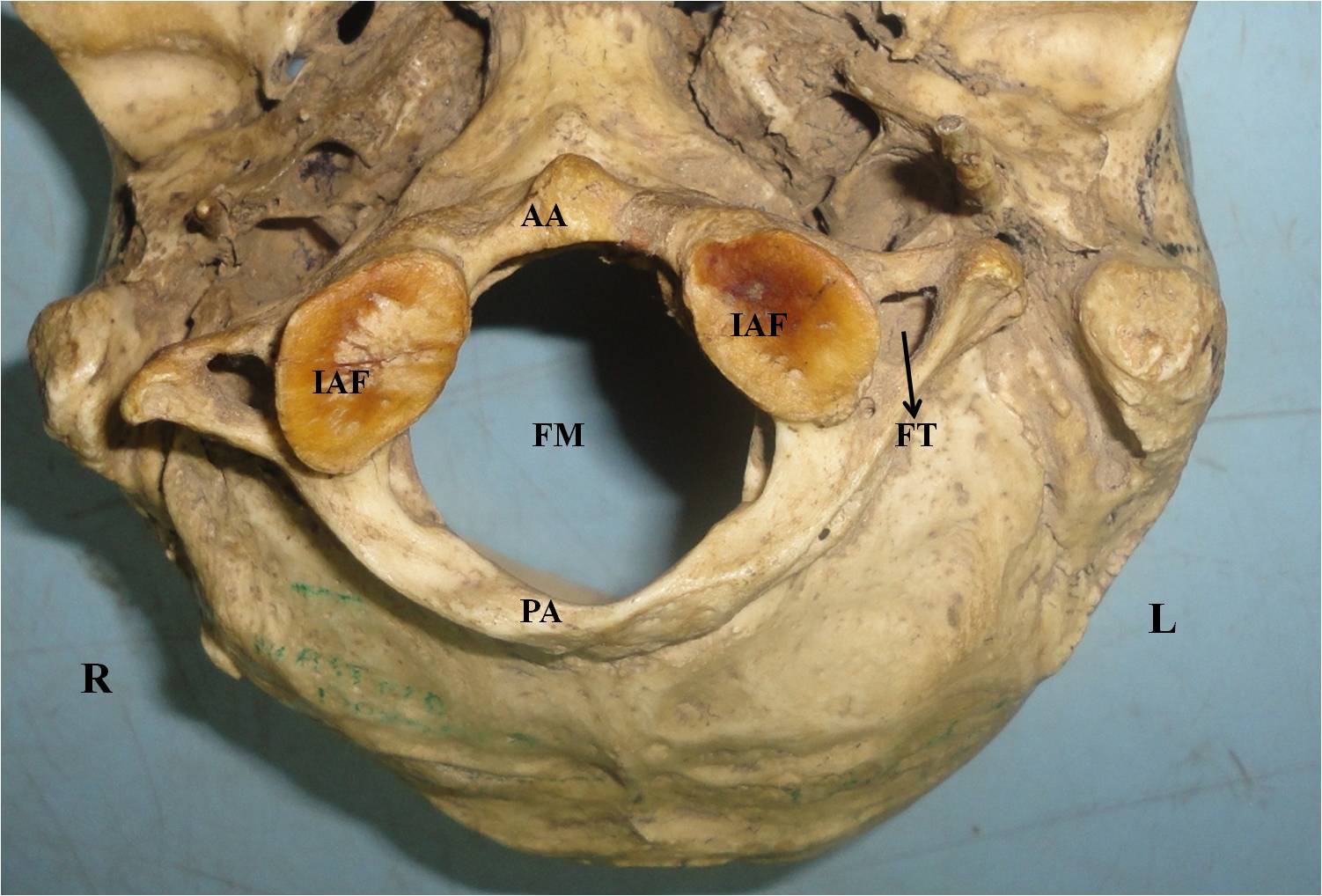
In another skull [Table/Fig-2], the anterior arch, posterior arch and lateral masses of the atlas were completely fused with the occipital bone. The transverse processes of the atlas were not fused to the occipital bone. The Anterior–Posterior Diameter (APD) and the Transverse Diameter (TD) of Foramen magnum were 26mm and 29mm respectively. Foramen magnum was oval in shape. Both the left and right superior articular facets of the atlas were completely fused with the corresponding occipital condyles while the inferior articular facets of the atlas were smooth and symmetrical. APD and TD of the left inferior articular facet were measuring 21mm and 17mm respectively, while APD and TD of the right inferior articular facet was measuring 20mm and 18mm respectively.
Base of the skull with atlanto-occipital synostosis. R-Right side, L-Left side, IAF-Inferior Articular Facet, PA-Posterior Arch, AA-Anterior Arch, FT-Foramen Transversarium, FM- Foramen Magnum
The remaining 198 skulls showed no anomalous fusion. The APD of foramen magnum of these skulls were ranging from 30mm to 40mm and the TD of foramen magnum was ranging from 26mm to 32mm.
Discussion
The Atlanto occipital joint is the pair of condyloid joints which is formed by the articulation of occipital condyles of the skull with the superior articular facets of the first cervical vertebra. This joint brings about flexion and extension of the head. Atlas can fuse with the occiput resulting in synostosis. Anatomy and surgery textbooks do not describe the complete morphology of these variations. Many such anomalies of the craniovertebral region can be encountered incidentally. Occipitocervical synostosis can range from the complete fusion of the atlas with the occiput to discrete osseous bridges between the atlas and occiput. The synostosis has been classified into four types based on the zones of atlas fused with occiput.
Zone 1–fusion involving the anterior arch of atlas in front of the lateral masses (20% in their series);
Zone 2–fusion involving primarily the lateral processes (17%);
Zone 3–fusion involving the posterior arch of atlas behind the lateral masses (13%) and
Combinations of zones– were seen in over 50% of patients.
In a majority of cases, the fusion occurs between the anterior arch of the atlas and the anterior margin of the foramen magnum [5]. In the present study, combinations of zones of atlanto-occipital fusion were seen.
Occipitocervical synostosis is associated with other skeletal malformations such as Spina bifida of atlas, occipital vertebra, basilar invagination, Klippel-Feil syndrome (fusion of the second and third cervical vertebrae), Arnold Chiari I malformation and cervical stenosis [6].
The Incidence of atlanto-occipital fusion in the present study is compared with the available data as per the literature [3, 7–10] [Table/Fig-3].
Incidence of Atlanto–occipital fusion
| Authors Name | Incidence = No. of cases/ Total no. of skulls studied | Percentage (%) |
|---|
| Hussain Saheb et al., [7] | 1/125 | 0.80 |
| Sharma et al., [8] | 2/70 | 2.85 |
| Seema et al., [9] | 2/100 | 2 |
| Kassim et al., [10] | 2/55 | 3.63 |
| Surekha et al., [3] | 1/150 | 0.67 |
| Present Study | 2/200 | 1 |
Occipitocervical synostosis result in the shift of the first mobile segment between the skull and spine to the C1–C2 junction. This causes stress and restricted range of movement due to which there may be “over-stretch” failure of the supporting myoligamentous structures. Occipitalization of the atlas results in stress of the ligaments, leading to gradual loosening of the atlantoaxial joint with progressive atlantoaxial subluxation. The clinical symptom of atlantoaxial subluxation is torticollis with inclination of the head to one side, rotation of neck to the contralateral side with slight flexion [11].
Embryological Significance:
The ventromedial portion of the somite forms sclerotome which surrounds the notochord and develops into the vertebral body. The dorsal portion surrounds the neural tube and develops into the posterior vertebral arch. The caudal half of each sclerotome combines with the cranial half of the sclerotome below it. The cranial half of the first cervical sclerotome combines with the caudal half of the last occipital sclerotome to form the base of the skull, while the caudal half of the first cervical sclerotome combines with the cranial half of the second cervical sclerotome to form the first cervical vertebra, the pattern continues in this fashion to form the rest of vertebrae. [12]. The body of first cervical vertebra is stolen by the body of second cervical vertebra to form the dens, thus the first cervical vertebrae (atlas) doesn’t have a body unlike other vertebrae. The body, posterior arch and transverse processes of second cervical vertebra (axis) is derived from second cervical sclerotome [13].
Occipitocervical synostosis arises as a result of failure of segmentation of the first cervical somite into its cranial and caudal components. Consequently, the atlas gets fused into the occipital region, because the fourth occipital somite has fused with the entire first cervical somite and also the cranial portion of the second cervical somite [14].
Inactivation of HOX D-3 gene expression in mice results in anterior homeotic transformation at the craniovertebral junction, due to which the atlas takes on an occipital identity and the head–neck transitional zone moves caudally to the atlanto-axial junction [15].
Clinical significance
Patients with occipitocervical synostosis do not develop the symptoms until the second decade of life. This can be due to the gradual increase in ligamentous laxity and instability with aging [3]. The most common course is a progressive one, but sudden onset or instant death has also been reported.
The standard sagittal diameter of Foramen Magnum range between 28-38 mm and its transverse diameters ranges between 25-40 mm. Spinal cord compressions never occur when the sagittal diameter of foramen magnum is 18 mm or more. It has been reported that the protruding mass in Foramen Magnum and border line reduced diameter might not have caused compression of Medulla Oblongata or spinal cord, but reduced diameter might compress vertebral vessels [2]. It was also reported that, spinal cord compression always occurs when the sagittal spinal canal diameter behind the odontoid process is less than or equal to 14 mm. Spinal cord compression occurs when the sagittal canal diameter is between 15 and 17 mm [8].
Compression of spinal cord or the brain stem due to occipitocervical synostosis can produce signs and symptoms, which vary from simple headache to a full blown neurological syndrome. The neurological complications could be the result of compression of spinal cord, nerves and vessels. The symptoms of neurological syndrome due to occipitocervical synostosis can be occipital headache, neck pain, numbness and pain in the limbs, weakness and abnormal head posture [8,16,17]. Cranial nerve findings include tinnitus, visual disturbances and lower cranial nerve palsies leading to dysphagia and dysarthria [17].
The anomalies pertaining to craniovertebral junction is of great importance because of the presence of vertebral artery and first cervical nerve on the superficial aspect of atlas. Compression of the vertebral artery can cause compromise blood flow to the brain. Similarly compression of first cervical nerve can cause neurological symptoms [3]. As the pathophysiology of both atlanto-occipital fusion and Arnold Chiari malformation is similar, their neurological symptoms and signs cannot be distinguished [18, 19]. It has been reported that patients with atlanto-occipital fusion can have tonic or clonic convulsions[17,18]. Thus head and neck surgeon should be aware of occipitocervical synostosis which may cause wide range of clinical features.
Conclusion
Occipitocervical synostosis can present without any typical symptoms. Restriction or absence of movement in the atlantooccipital joint may be the first sign which attracts the attention of surgeons regarding occipitocervical synostosis. Knowledge of the incidence and morphology of this abnormality is important for radiologists during diagnostic imaging studies. Awareness of this abnormality is a prerequisite for a neurosurgeon to perform a thorough preoperative clinical assessment and prevent complications during and after the upper cervical spinal manipulations.