Multiple Hepatic Inflammatory Pseudotumours Diagnosed after Laparoscopic Excisional Biopsy
Andre Costa–pinho1, Renato Bessa Melo2, Luis Graca3, Jose Manuel Lopes4, J. Costa–Maia5
1 HBP Unit, Department of General Surgery, S. Joao Medical Center, Faculty of Medicine of Porto University, Portugal.
2 HBP Unit, Department of General Surgery, S. Joao Medical Center, Faculty of Medicine of Porto University, Portugal.
3 HBP Unit, Department of General Surgery, S. Joao Medical Center, Portugal.
4 Department of Pathology, S. Joao Medical Center, Faculty of Medicine of Porto University, Portugal.
5 HBP Unit, Department of General Surgery, S. Joao Medical Center, Portugal.
NAME, ADDRESS, E-MAIL ID OF THE CORESPONDING AUTHOR: Dr. Andre Costa Pinho, Rua Dr. Eduardo Santos Silva 26B 1° Frente Esq, 4200-282 Porto, Portugal.
E-mail: andrecostapinho@gmail.com
Inflammatory pseudotumours (IPTs) may occur in almost every organ of the human body, the liver being the second most frequent organ which is affected. Inflammatory pseudotumours of the liver are rare benign lesions of unknown aetiology, which usually present as solitary liver masses of variable sizes. The differential diagnoses of malignant liver tumours are challenging and they usually require biopsies and histologic examinations. We are presenting the case of a patient with multiple hepatic lesions which mimicked liver metastases. Two percutaneous biopsies were inconclusive. The definitive diagnosis of multiple hepatic inflammatory pseudotumours was made after a laparoscopic exploration with an excisional biopsy of liver lesions and their pathologic evaluation. All lesions disappeared after several months, without any further treatments.
Inflammatory pseudotumour, Liver, Biopsy
Case Report
We are presenting the case of a 67–year–old male patient who had a history of colonic diverticular disease and oesophageal hiatus hernia, which was usually medicated with omeprazole. He had no history or risk factors for liver disease.
The patient was referred due to multiple focal liver lesions which were associated with fever and abdominal discomfort, with 1 month of evolution. His abdomen was not tender and no masses were palpable. Laboratory data on admission showed WBCs–11.620/mm3 with 55% neutrophils, CRP–22.5 mg/L, and gamma–GT–108U/L without other alterations. Blood and urine cultures were negative. The patient was negative for hepatitis C virus, hepatitis B virus and HIV. Subsequent analysis showed no significant elevation of inflammatory markers or other relevant changes. The patient maintained low–grade fever.
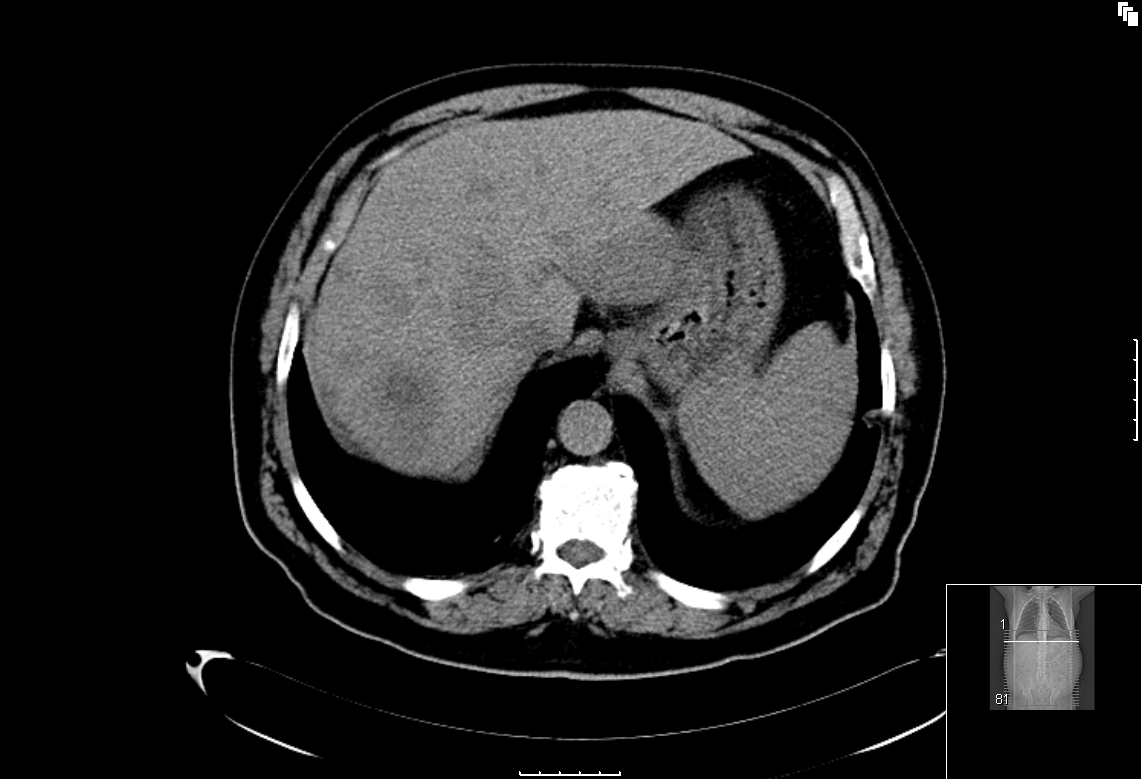
A contrast–enhanced abdomino–pelvic Computed Tomography (CT) scan showed multiple focal liver lesions with a delayed enhancement, which was suggestive of secondary lesions without any other abnormalities [Table/Fig-1]. The upper and lower endoscopies disclosed no suspicious lesions; tumour markers were all within the normal reference range. Two percutaneous liver biopsies were inconclusive.
Abdomino-pelvic CT scan showing multiple focal liver lesions
For diagnostic purposes, the patient underwent an exploratory laparoscopy which revealed bilateral hepatic lesions with no other abdominal abnormalities, namely in the gastrointestinal tract. An intra–operative liver ultrasonography (IOUS) showed multiple (>10) liver lesions which were smaller than 4cm, which were scattered throughout the liver parenchyma. Resections of 3 superficial lesions from segment III were performed.
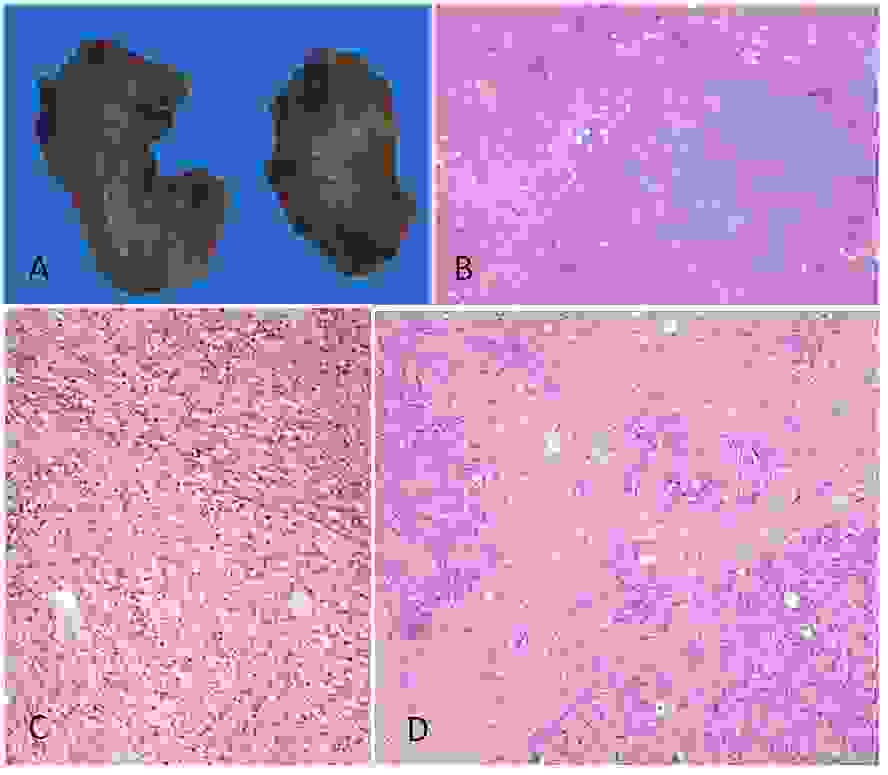
The tumour specimens consisted of liver fragments (2.0 to 3.5cm) which were occupied by solid, whitish and well-circumscribed nodular lesions [Table/Fig-2A,B,C,D]. Microscopically, lesions disclosed similar features: they were well defined, expansive and highly cellular, they were composed of oval to spindle cells, with a slight pleomorphism and a low mitotic index and they were intermixed with varying numbers of plasma cells and fat–laden foamy macrophages. The spindle cells were arranged in interlacing fascicles, with a moderate amount of intercellular collagen. In the imunohistochemistry study, the spindle cells expressed vimentin, focally actin, and CD68, namely, in the macrophage component; the lesion did not express keratins, S100 protein, ALK and desmin. Histochemistry stains (which included PAS and Ziehl Neelsen) were negative. These features were consistent with the diagnosis of multiple inflammatory pseudotumours (IPT) of the liver.
Liver pseudotumour features disclosing: A – solid macroscopic lesions (specimen sections); B – well circumscribed nodular growth pattern surrounded by liver parenchyma; C – spindle cells admixed with inflammatory mononuclear cells and some macrophage lipid rich cells; D –variable extensive collagenous intercellular stroma
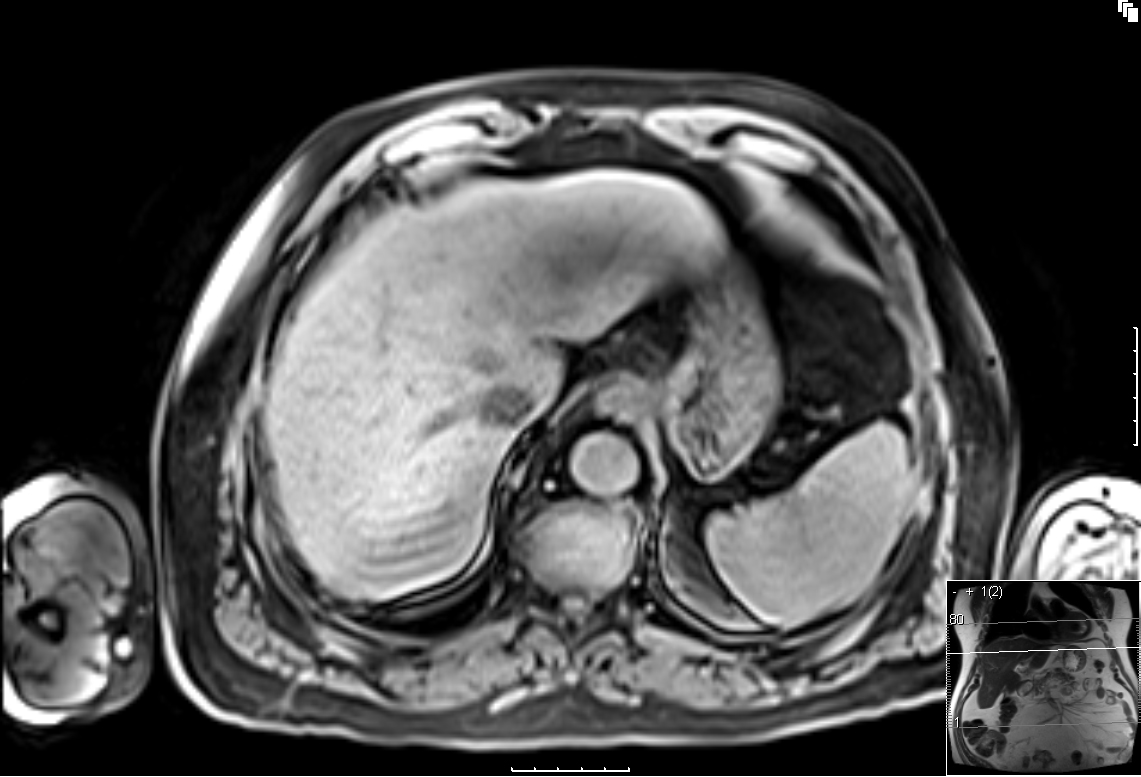
The patient had an uneventful post-operative course, with discharge at day 4. No further treatment was taken. He remained asymptomatic and a CT–scan which was done 6 months after surgery, showed reduction in the size and number of the remaining lesions. After 18 months, complete remission of the lesions was observed on control Magnetic Resonance Imaging [Table/Fig-3].
Complete remission after 18 months on control abdomino–pelvic MRI
Discussion
The differential diagnosis of a middle–aged patient with multiple focal liver lesions and low–grade fever includes liver malignancies (primary or secondary) and abscesses (pyogenic or parasitic). Investigation requires a detailed clinical history, a physical examination and analytical and imaging studies, which establish the correct diagnosis in a majority of cases.
This patient presented no risk factors for hepatocellular carcinoma or intrahepatic cholangiocarcinoma. A contrast enhanced CT–scan was suggestive of liver metastasis. However, endoscopic studies of the digestive tract and the abdomino–pelvic CT–scan showed no suspicious lesions, and tumour markers were within normal range. Infectious causes were ruled out by a negative serology and cultures.
IPT of the liver is a rare disease of unknown aetiology. Some authors have proposed that this condition might be associated with infectious agents [1], genetic abnormalities [2] and autoimmune diseases [3]. IPTs may develop in several organs, which may suggest systemic abnormalities. Nevertheless, it is unusual to find multiple lesions in the same organ, as was observed in our patient.
The clinical presentation of an IPT is variable and it is related to its location; general symptoms (fever, fatigue, anorexia and weight loss) are present in 5%–30% of cases [4]. IPTs of the liver may cause only abdominal discomfort or mild fever, and they rarely produce symptoms of biliary obstruction, portal hypertension or liver failure.
Radiological findings of hepatic IPTs have been reported as non–specific: a delayed enhancement on a contrast–enhanced CT–scan is usual, but a radiological appearance might be related to the duration of the disease process, the amount of fibrous tissue and the degree of cellular infiltration [5]. Diagnosis frequently requires invasive procedures, as a malignancy is otherwise difficult to rule out.
There are few reports [4,6,7] on IPTs of the liver which were diagnosed by needle biopsies – in our patient, two percutaneous liver biopsies were inconclusive. In this setting of a diagnostic uncertainty, an abdominal exploration and an excisional biopsy of the tumour were required. Laparoscopy has obvious advantages over laparotomy, such as an improved recovery with an early mobilisation, less pain and less ileus. The combination with IOUS improves liver exploration and detection of lesions, which are not shown by conventional imaging techniques [8]. In our case, this approach led to the correct diagnosis in a difficult clinical setting by using a minimally invasive technique.
IPTs of the liver are considered as benign lesions with eventual regressions, either spontaneously or after anti–inflammatory treatments, but there are reports on insidious progressions with local recurrences and even neoplastic transformations [9]. The optimal treatment is controversial, but a liver resection is usually not indicated.
In conclusion, multiple IPTs of the liver are a rare condition. Differential diagnosis of liver malignancies is difficult and invasive diagnostic procedures are usually required. In this setting, a laparoscopic approach is a safe and useful tool that allows a definitive pathologic diagnosis of an IPT.
[1]. Arber DA, Weiss LM, Chang KL, Detection of Epstein-Barr Virus in inflammatory pseudotumorSemin Diagn Pathol 1998 15(2):155-60. [Google Scholar]
[2]. Cessna MH, Zhou H, Sanger WG, Expression of ALK1 and p80 in inflammatory myofibroblastic tumor and its mesenchymal mimics: a study of 135 casesMod Pathol 2002 15(9):931-38. [Google Scholar]
[3]. Kojima M, Nakamura S, Itoh H, Inflammatory pseudotumor of the submandibular gland: report of a case presenting with autoimmune disease-like clinical manifestationsArch Pathol Lab Med 2001 125(8):1095-97. [Google Scholar]
[4]. Sari A, Tunakan M, Unsal B, Inflammatory pseudotumor of the liver diagnosed by needle biopsy: report of three cases (one with neuroendocrine tumor of the rectum and lung)Turk J Gastroenterol 2010 21(3):308-12. [Google Scholar]
[5]. Yoon KH, Ha HK, Lee JS, Inflammatory pseudotumor of the liver in patients with recurrent pyogenic cholangitis: CT-histopathologic correlationRadiology 1999 211(2):373-79. [Google Scholar]
[6]. Rosa B, Moutinho-Ribeiro P, Pereira JM, Ghost tumor: an inflammatory pseudotumor of the liverGastroenterol Hepatol 2012 8(9):630-3. [Google Scholar]
[7]. Yoshida T, Nishimori I, Kumon M, Inflammatory pseudotumor of the liver: report of a case diagnosed by needle biopsyHepatol. Res 2003 27(1):83-86. [Google Scholar]
[8]. Santambrogio R, Opocher E, Ceretti AP, Impact of intraoperative ultrasonography in laparoscopic liver surgerySurg Endosc 2007 21(2):181-88. [Google Scholar]
[9]. Horiuchi R, Uchida T, Kojima T, Inflammatory pseudotumor of the liver. Clinicopathologic study and review of the literatureCancer 1990 65(7):1583-90. [Google Scholar]