Isolated Cutaneous Sarcoidosis: A New Insight into the Old Entity
Sharath Kumar H K.1, Gayathri M N.2, Bharathi M.3, Ravikumar T.4
1 Associate Professor, Department of Pathology,
2 Assistant Professor, Department of Pathology,
3 Professor, Department of Pathology,
4 PG Student, Department of Pathology, Mysore Medical College & Research Institute.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sharath Kumar H.K., Associate Professor, Department of Pathology, Mysore Medical College & Research Institute.
Phone: 09743813949,
E-mail: sharath_hk@hotmail.com
Cutaneous lesions are a part of common manifestation in multi–systemic sarcoidosis and skin involvement occurs in 20% to 35% of the patients with systemic disease. An exclusive cutaneous involvement is rare and it is reported in about 4%-5% of the patients of sarcoidosis. These lesions have been classified into specific and non–specific, depending on the presence of non- caseating granulomas, on histopathologic studies. In the present study, we are reporting two cases of isolated cutaneous sarcoidosis without systemic manifestations, which is a rare presentation. Sarcoidosis will continue to challenge even the most experienced clinicians with respect to a high degree of suspicion and further investigations for diagnosing and treating this disorder.
Cutaneous, Sarcoidosis, Non-Caseating granulomas
Case Report One
A 57–years–old male presented with a raised erythematous lesion which measured 1.5x1.5 cm over the forehead. The lesion started as a papule and gradually progressed to the present size. There was no history of dyspnoea, prolonged fever or other systemic complaints. There was no significant family history which included that of tuberculosis. The haematological and biochemical investigations including angiotensin converting enzyme (ACE) levels, ESR, CRP, ANA and serum calcium showed normal values. The ophthalmological assessment was normal.
Case Report Two
A 38 year old male presented with a lesion which measured 2 x 1.5 cm over the elbow region, which was provisionally diagnosed as a neurofibroma. The biopsy showed well formed non caseating granulomas with asterioid bodies and Langhans giant cells and a histopathological diagnosis of sarcoidosis was offered. Further evaluation showed no organ involvement and no hilar lymphadenopathy.The patient showed no ocular involvement on ophthalmological assessment and other investigations were normal, including sputum for AFB culture. ACE levels were on higher side of the normal range.
Discussion
Prevalence of cutaneous sarcoidosis in India is not exactly known, because of a paucity of records [1]. No single lab test is diagnostic of Sarcoidosis. The diagnosis is confirmed on the demonstration of a typical non caseating granuloma on biopsy. In the absence of systemic manifestations, isolated cutaneous lesions such as these are misdiagnosed. The cutaneous lesions of Sarcoidosis assume a vast array of morphologies [2] and they are therefore considered as great mimickers in the dermatology practice. The specific types of lesions are lupus pernio, small and large nodules, small and large plaques and scar infiltrations. Lupus pernio is the most characteristic among the sarcoid skin lesions and it is seen as a chronic, persistent, bluish, indurated plaque with a predilection for nose and cheek, with nasal, mucosal and septal involvements [3].
The typical granulomas are noncaseating and they comprise few or no inflammatory cells and thus are referred to as “naked granulomas”. In the histopathology lupus vulgaris, tuberculoid leprosy, foreign body reactions and granuloma annulare may pose difficulties. Increased ESR, anaemia, leucopenia and hypercalcemia are the common laboratory abnormalities which were absent in our patients. The serum level of ACE is found to be elevated only in 50% of the cases and thus, it is not very reliable. Chest radiographs may reveal bilateral hilar lymphadenopathy. One of our cases, after 6 months, showed mild hilar densities on chestX ray. Thus, the diagnosis of sarcoidosis is confirmed by demonstrating a typical non caseating epithelioid cell granuloma on biopsy. Diagnosis of sarcoidosis is delayed, where tuberculosis still remains the first diagnostic possibility. In many cases, it is difficult to differentiate between Sarcoidosis and tuberculosis of the skin on histopathology [4].
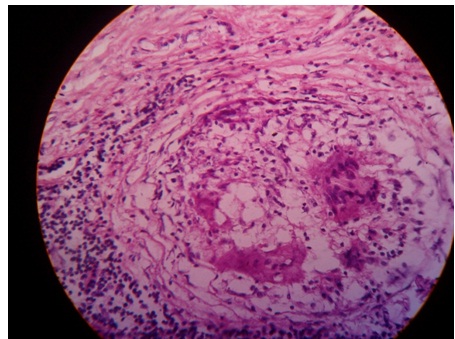
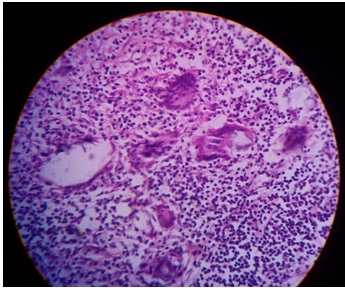
The infiltrate of Sarcoidosis lies scattered throughout the dermis, [Table/Fig-1] whereas the infiltrate in lupus vulgaris is located close to the epidermis. Sarcoidosis shows only few lymphoid cells at the periphery of the granulomas, [Table/Fig-2] giving the appearance of naked epithelioid cell tubercles, whereas lupus vulgaris shows a marked lymphocytic infiltrate around and between the granulomas [4]. The granulomas of sarcoidosis show minimal central necrosis as compared to those of lupus vulgaris. Cutaneous sarcoidosis with multisystem involvement is treated with topical steroids or systemic corticosteroids [5]. Asymptomatic patients with isolated lesions may not need systemic corticosteroids and they are followed up [6].
(H & E; 40x.) Non–necrotizing granulomas in sarcoidosis
(H &E;40x.) The giant cells containSchaumann’s bodies and Asteroid bodies
Conclusion
Isolated cutaneous Sarcoidosis is a rare presentation in any age group, the diagnosis of which is likely to be missed. The diagnosis should not be overlooked. Lesions of skin are reportedly associated with some form of systemic involvement. Therefore, patients who present with confination of the disease to the skin alone, should be followed up regularly for the probable risk of developing systemic manifestations at a later date.
[1]. Chiba T, Takahara M, Nakahara T, Fukagawa S, Takei K, Cutaneous Sarcoidosis clinically mimicking necrobiosis lipoidica in a patient with systemic SarcoidosisAnnals of Dermatology 2012 24(1):74-76. [Google Scholar]
[2]. Bargotra R, Suri J, Gupta Y, Cutaneous Sarcoidosis. JK ScienceJournal of Medical Education and Research Year: 2010 12(3):145-46. [Google Scholar]
[3]. Mishra RS, Indira C, Saxena U, Mukherjee A, Cutaneous SarcoidosisIndian J Dermatol Venereol Leprol 1993 59:190-93. [Google Scholar]
[4]. Juan R, Skin Dermatosis Tumour and tumour like conditionsIn: Rosai and Ackerman’s Surgical Pathology 2004 St Louis, MissouriMosby:93-245. [Google Scholar]
[5]. Singh G, Sangolli P, Dash K Grove, Cutaneous Sarcoidosis without systemic involvementIndian J Dermatol Venereol Leprol 2000 66:43-44. [Google Scholar]
[6]. Jung YJ, Roh MR, Clinical and histopathological analysis of specific lesions of cutaneous Sarcoidosis in Korean patientsJ Dermatolog Treat 2011 Feb 22(1):11-17. [Google Scholar]