Fibrosarcoma of the Mandible: A Diagnostic Dilemma
Kanwar Deep Singh Nanda1, Anurag Mehta2, Jasmine Nanda3
1 Senior Lecturer, Department of Oral and Maxillofacial Pathology, SGT Dental and Medical College, Gurgaon, India.
2 Head of Pathology, Department of Pathology, Rajiv Gandhi Cancer Institute and Research Institute, Rohini, India.
3 Post Graduate Student, ITS Dental College, Muradabad, Uttar Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Kanwar Deep Singh Nanda, 18/15 West Patel Nagar, New Delhi-110008, India. Phone- 011+91+9650122662,
E-mail: kdsnanda@gmail.com
Fibrosarcoma is a malignant mesenchymal neoplasm of fibroblasts that rarely affects oral cavity and can cause local recurrences or metastasis. The aetiologic factors are still unknown, but many authors have reported the radiation therapy history as an important aetiological factor, followed by trauma and underlying conditions like Paget’s disease, fibrous dysplasia or chronic osteomyelitis. Fibrosarcoma of mandible is rare, with an incidence which ranges from 0-6.1% of all primary fibrosarcomas of the bone. This paper has described a case of a swelling in the mandible of a 17-years old female who had a radiolucency in association with crown of an impacted tooth and foci of radiopacity, which led to a misdiagnosis of either an odontogenic lesion or a bone tumour, but proved to be a fibrosarcoma on histopathological and immunohistochemistry investigations.
Fibrosarcoma, Mandible, Vimentin, Spindle cell tumour, Misdiagnosis, Oral cavity
Case Report
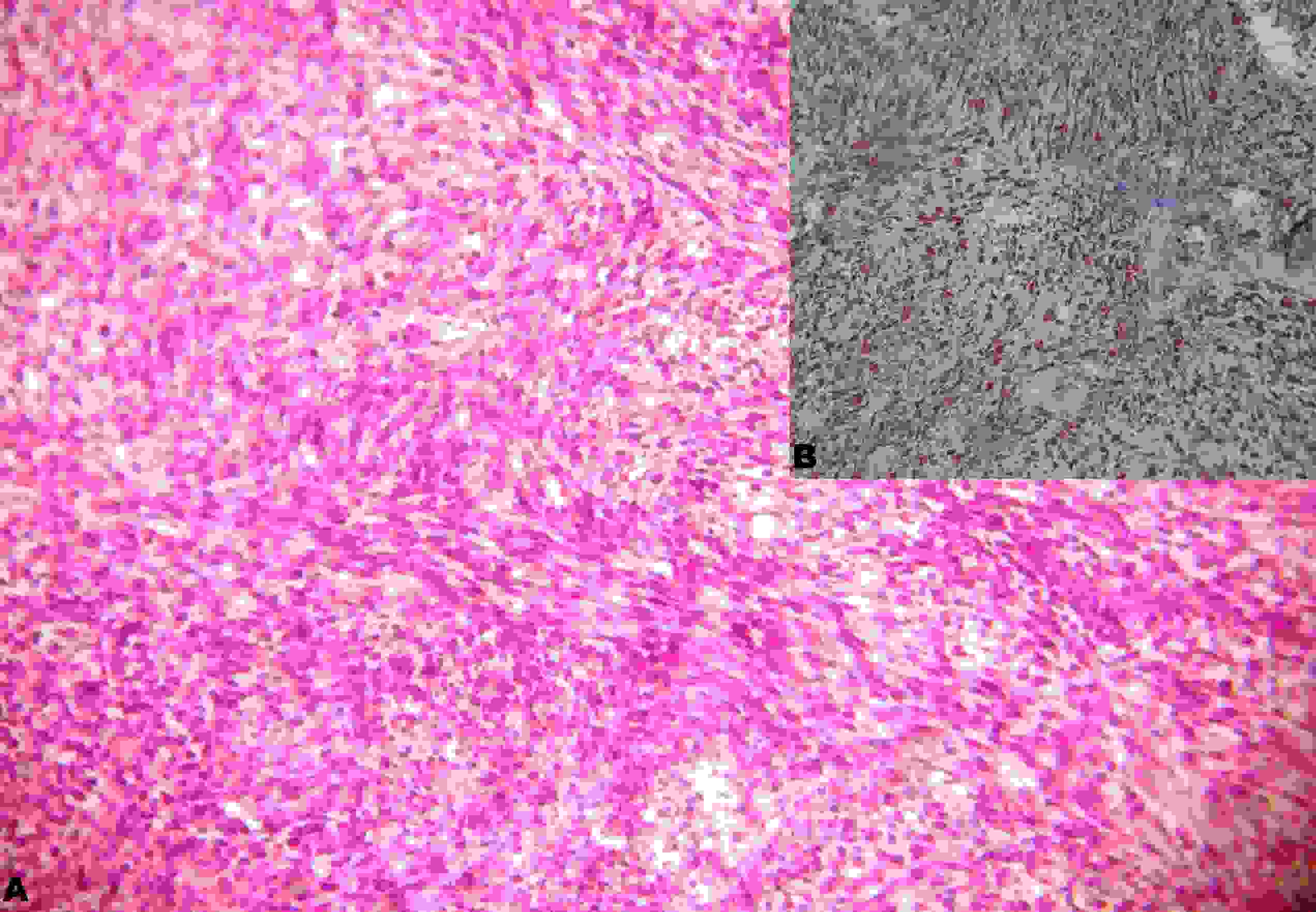
A 17-years old female was referred to Department of Pathology with a painful swelling on the right side of face [Table/Fig-1a]. No history of any systemic illness or trauma to the present area was present. She gave a history of pain in the right posterior mandibular region of 1 month duration, which was associated with a difficulty in chewing food and a limited mouth opening. Extra-orally, the swelling was irregular in shape, with ill defined borders, which extended superiorinferiorly from ala tragus line to inferior border of the mandible and anterioposteriorly from right corner of the mouth to preauricular region [Table/Fig-1b]. The swelling was firm in consistency and painful on palpation. The right submandibular lymph node was palpable and non-tender. Intraorally, the swelling appeared to arise from buccal mucosa. An Orthopantomograph (OPG) revealed osteolytic areas in the right mandibular angle and ramus, with ill defined borders, in association with an impacted mandibular right third molar. In addition, there were foci of calcification at the ramus of the mandible [Table/Fig -2]. A radiolucency which involved the impacted #48 tooth led to the provisional diagnosis of an odontogenic tumour or cyst, but the presence of a calcification at the ramus of the mandible suggested mimicking of an osteosarcoma or a chondrosarcoma. To determine the nature of the oral mass, an incisional biopsy was performed under local anaesthesia. The haematoxylin and eosin stained section showed a non-encapsulated tumour tissue which was made of collagenous stroma, with fascicles of spindle shaped cells. The cells exhibited hyperchromatic nuclei and an increased nuclear cytoplasmic ratio. In few areas, there was presence of a herring bone pattern, which was characteristic of a fibrosarcoma [Table/Fig-3a]. A histopathological diagnosis of a fibrosarcoma was made. Further, an immunohistochemical analysis showed a positive reaction for vimentin and negative ones for pan cytokeratin, desmin, actin and S-100 protein, which confirmed it as fibrosarcoma [Table/Fig-3b]. Patient was referred for a surgical excision, for further treatment. The patient did not report for follow up.
A and B: Swelling in the right posterior mandibular region

Orthopantomograph (OPG) showing osteolytic areas in the right mandibular angle and ramus. Foci of calcifications at the ramus of the mandible illustrated with arrows

A: (HE Staining, Magnification10x) Collagenous stroma with fascicles of spindle shaped cells exhibiting hyperchromatic nuclei and increased nuclear cytoplasmic ratio with presence of herring bone pattern. B: (Immunohistochemistry for Vimentin, Magnification 10x) Neoplastic cells showing immunoreactivity for vimentin
Discussion
A fibrosarcoma is a malignant tumour that arises from fibroblasts. Fibrosarcomas can arise in soft tissues or within bones. Intra-osseous fibrosarcomas may develop endosteally or possibly periosteally, the latter affecting bones by spread from adjacent soft tissues [1]. The mean age for the occurrence of fibrosarcomas is between the 2nd and 6th decades of life, with equal gender distribution. In the head and neck region, only 0.05 % cases have been reported, with mandible as a rare site of occurrence [2].
Clinically, the tumour presents with a swelling which is associated with pain and paresthaesia and occasionally with loss of teeth and ulceration of the overlying mucosa [3,4]. Radiological imaging of fibrosarcomas has revealed radiolucent lesions with a geographical, moth eaten or a permeative pattern of bone destruction [5]. The change of appearance in radiographic imaging in the present case was striking. The radiograph showed an impacted #48 with a radiolucency around the tooth, which gave an appearance of an odontogenic cyst or a tumour. In contrast, there were foci of calcification at the ramus of the mandible, which mimicked a chondrosarcoma or an osteosarcoma. Further histopathological and immunohistological investigations are necessary for making a final diagnosis.
Microscopically, low grade fibrosarcoma has been characterized as uniform spindle shaped cells which are arranged in fascicles, having a herring bone growth pattern. There are mild degrees of nuclear pleomorphism and rare mitoses. High grade lesions show intense nuclear pleomorphism, a greater cellularity and atypical mitoses [4]. In the present case, pleomorphic spindle shaped cells were arranged in a herring bone pattern, which were associated with collagen and mild mitosis which are characteristic of fibrosarcoma characteristic of a fibrosarcoma. The histological appearance of a fibrosarcoma is similar to that of fibromatosis, fibroblastic odontogenic sarcoma, malignant fibrous histocytoma, liposarcoma and synovial sarcoma. In fibromatosis, mitosis is absent and the grade of cellular atypia is very low. Odontogenic sarcomas shows odontogenic tissues which are absent in fibrosarcoma. To rule out a fibrous histiocytoma, a liposarcoma or a synovial sarcoma from a fibrosarcoma, an Immunohistochemical (IHC) study was carried out for the following markers: vimentin, pan cytokeratin, desmin, actin and S-100 protein. IHC showed vimentin positive cells, while the other immunomarkers showed negativity. A fibrosarcoma is essentially a diagnosis of exclusion and by definition, there should be no expression of actin, cytokeratin, S-100 and desmin [6].
The treatment choice of fibrosarcomas is radical surgery [1,6]. Radiation therapy and chemotherapy can be used for inoperable cases or as a palliative treatment, as their role in treatment is still unclear. They are given for high grade tumours, as these tumours may present with subclinical or microscopic metastases. Prognosis of the tumour is dependent on histological grade, tumour size and adequate surgical treatment with disease free margins. The five year survival rate for this disease is poor, ranging from 20 to 35% [3,6].
Conclusion
The present case is unique in sense that clinical and radiographic imagings were misleading. They suggested an odontogenic and a bone tumour. In the delineation of differential entities, the clinical, radiological and histological findings are very important in the diagnostic evaluation of the lesion, and they must be considered along with the immunohistochemical findings. Hence, in cases of rapidly growing lesions in oral cavity, fibrosarcomas must be included, as there is still a paucity of reports on fibrosarcomas in the head and neck region.
[1]. Lo Muzio L, Mignogna MD, Pannone G, Staibano S, Testa NF, A rare case of fibrosarcoma of the jaws in a 4-year-old maleOral Oncol 1998 34:383-86. [Google Scholar]
[2]. McKenna WG, Barnes MM, Kinsella TJ, Rosenberg SA, Lack EE, Combined modality treatment of adult soft tissue sarcomas of the head and neckInt J Radiat Oncol Biol Phys 1987 13:1127-33. [Google Scholar]
[3]. Pereira CM, Jorge J Jr, Di Hipólito O Jr, Kowalski LP, Lopes MA, Primary intra-osseous fibrosarcoma of jawInt J Oral Maxillofac Surg 2005 34:579-81. [Google Scholar]
[4]. Orhan K, Orhan AI, Oz U, Pekiner FN, Delilbasi C, Misdiagnosed fibrosarcoma of the mandible mimicking temporomandibular disorder: a rare conditionOral Surg Oral Med Oral Pathol Oral Radiol Endod 2007 104:e26-29. [Google Scholar]
[5]. Theodorou DJ, Theodorou SJ, Sartoris DJ, Primary non-odontogenic tumours of the jawbones: an overview of essential radiographic findingsClin Imaging 2003 27:59-70. [Google Scholar]
[6]. Yamaguchi S, Nagasawa H, Suzuki T, Fujii E, Iwaki H, Sarcomas of the oral and maxillofacial region: a review of 32 cases in 25 yearsClin Oral Investig 2004 8:52-55. [Google Scholar]