Management of Giant Cystic Lymphangioma in an Infant
Rajendra K. Ghritlaharey1
1 Associate Professor, Department of Paediatric Surgery, Gandhi Medical College and Associated, Kamla Nehru and Hamidia Hospitals, Bhopal, Madhya Pradesh-462 001, India.
NAME, ADRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Rajendra K. Ghritlaharey, Associate Professor, Department of Paediatric Surgery, Gandhi Medical College and Associated Kamla Nehru and Hamidia Hospitals Bhopal, Madhya Pradesh 462 001, India.
Phone: + 91-755 - 4050571(R), 4050261(O)
Lymphangiomas are benign lesions with a marked predilection for the head and neck region. Giant lymphangiomas of head and neck may occur and they may present with life threatening complications. The author is presenting here, a three month-old boy who presented with a giant cystic lymphangioma on left side of neck, which extended to the head as well. His clinical diagnosis of a cystic lymphangioma was confirmed on a Ultrasonography (USG) examination. Complete surgical excision of the lesion was achieved, without damaging any vital structures. His post-operative recovery was uneventful. A follow-up at two months after his surgery showed a cosmetically acceptable scar and no recurrence was noted.
Cystic hygroma, Cystic lymphangioma, Giant cystic hygroma
Case Report
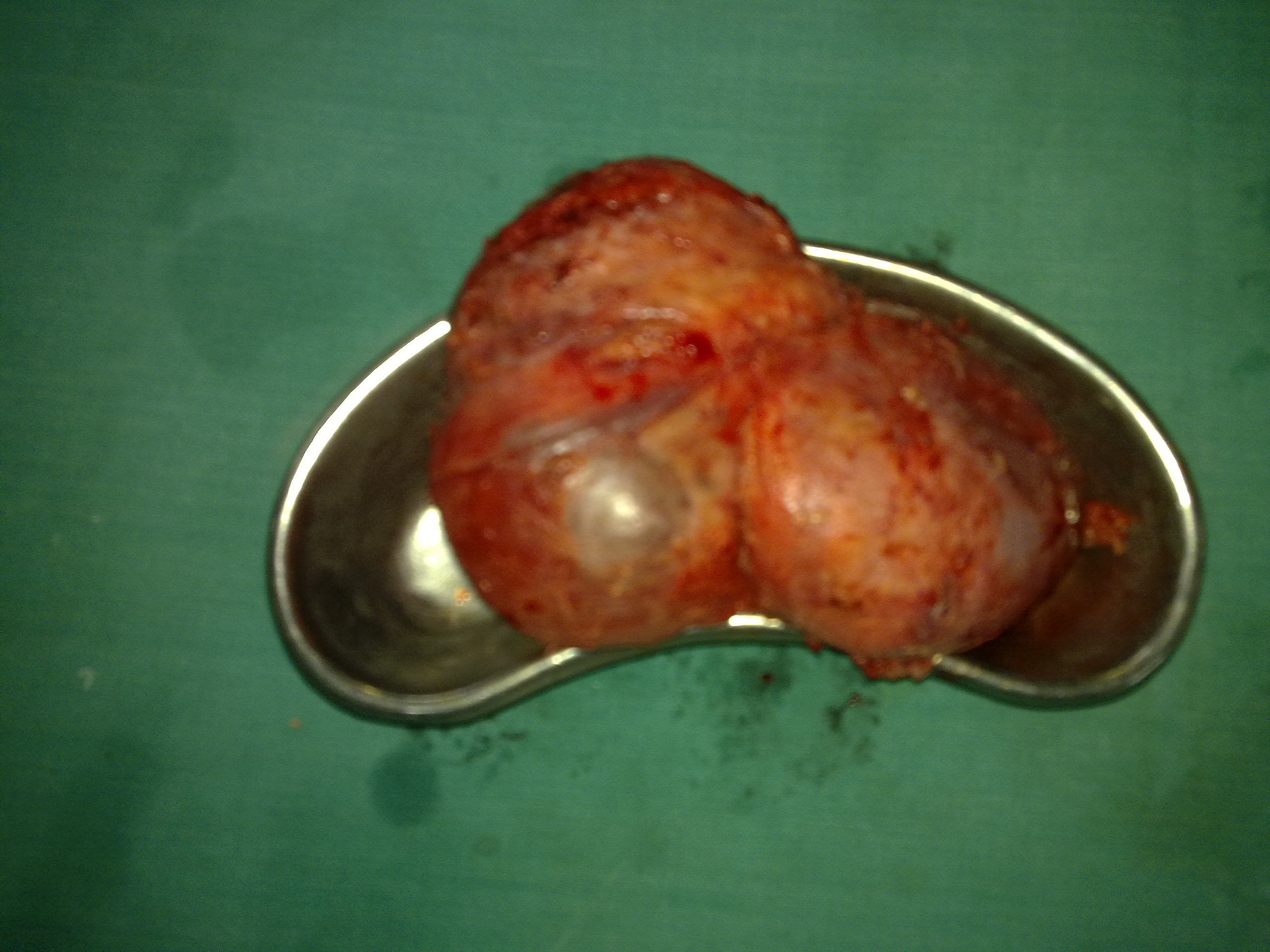
A three months – old, male child (full-term, normally delivered) was admitted with complaint of a progressive increasing swelling on left side of the neck and head, which was there since birth. His antenatal history showed nothing significant. There was no history of respiratory distress or dysphagia. Clinical examination of the swelling revealed a soft, cystic, tense, non-tender swelling which measured 15x12 cm, which occupied left side of the neck, extended to the head and involved back side of the left ear and part of the posterior occipital area [Tables/Figs-1a, 1b, and 1c]. It also displaced the left external ear upwards and interiorly. A trans-illumination test of the swelling which was done was positive. No other obvious congenital anomalies were detected. USG studies of the swelling reported a multi-cystic cystic hygroma. Other systemic examinations and routine laboratory investigations were within normal limits. Complete surgical excision of the cystic hygroma was achieved, without injury to the adjacent nerves and blood vessels [Table/Fig-2a, and 2b]. Redundant extra skin was excised and wound was closed with suction drainage in place and the external ear was also approximated well in place [Table/Fig-3]. His post–operative recovery was uneventful and he was discharged on 10th post–operative day. A histopathology examination of the excised tumour confirmed the diagnosis of a cystic lymphangioma /hygroma. A follow-up which was done at two-months after excision showed no recurrence and it showed only a cosmetically acceptable scar [Table/Fig-4].
Clinical photograph (front view) showing giant cystic hygroma involving head and neck

Clinical photograph showing giant cystic hygroma and displacement of the ear

Clinical photograph of patient after endotracheal intubation

Operative photograph showing surgical excision in progress

Excised specimen showing completely excised cystic hygroma
Operative photograph showing closure of the wound

Photograph showing cosmetically good acceptable scar

Discussion
Lymphangiomas are benign, hamatomatous, congenital malformations of lymphatic system [1]. Hygroma is a Greek word which means ‘water-containing tumour’ [2]. Lymphangiomas can manifest anywhere in the body, but are most commonly seen in cervico-facial regions (especially in posterior cervical triangle), axilla, mediastenum, groin and oral cavity [1–3]. More than 95% of lymphangiomas are situated in the head, neck, axilla and extremities [1–3]. Other sites which also include the abdomen have been found to be affected only in 5% of the cases [4,5]. Occasionally, cystic lymphangiomas may occur in the liver, spleen, kidney, intestine, and other rare sites [1, 2].
Lymphangiomas are usually classified as lymphangioma simplex (capillary), cavernous lymphangioma and cystic lymphangioma. Cystic lymphangioma is commonly referred to as cystic hygroma [1] Lymphangiomas may also be classified on the basis of sizes of their cysts as microcystic, macrocystic and mixed lymphangiomas. Microcystic lymphangiomas consist of cysts which measure less than 2 cm in size, macrocystic lymphangiomas consist of cysts which measure more than 2 cm in size, and in mixed lymphangiomas, the cysts are of variable sizes [2]. Cystic hygromas occur more frequently as compared to other types of lymphangiomas, and they may be composed of single or multiple macrocystic lesions [2].
Embryologically; lymphangiomas are believed to originate from sequestrations of lymphatic tissues / vessels that fail to establish a connection with normal draining vessels during intrauterine life [1,2]. More than two thirds of the lymphangiomas are apparent at birth, and most of them present by the end of the second year of life [1]. Clinically; cystic hygromas are large, soft, cystic, and non-tender masses. Transillumination is positive, unless it is complicated with haemorrhage or recurrent infections [1–4, 6]. Although lymphangiomas are benign lesions, they can compress and infiltrate the vital structures or they can exist with complications such as intracystic haemorrhages, cyst rupture or infections [1, 2]. Giant cystic hygromas of neck and oral cavity may present with respiratory distress and dysphagia [1–3,7].
The prenatal diagnosis of a cystic hygroma, which is made by using ultrasound, has been well documented in the literature [1,8]. Post-natally, the diagnosis of a cystic hygroma is usually obvious and it is made by doing a physical examination and it can be confirmed on USG of the swelling. In cases of cystic lymphangiomas which involve the deeper structures, computed tomography scans and magnetic resonance imaging may be used for a better understanding of the anatomy and adjacent vital structures [1,2,4,5].
Indications for the treatment of lymphangiomas include disfigurement, large sizes, leakage of lymphatic fluid (rupture), recurrent infections, etc [1,2,5,6]. Respiratory distress and dysphagia may be the reasons for seeking early/emergency treatment for lymphangiomas which involve neck and oral cavity [1,3,7]. The most preferred modality which is used for treating cystic lymphangiomas remains a complete surgical excision [1–7]. Other modalities which are used for treating lymphangiomas are; simple drainage, aspirations, steroids, sclerotherapy (OK-432, monoclonal antibody, bleomycin), radiation, laser excision, radio-frequency ablation and cauterization, which have their own merits and demerits [1,2]. Management of giant cystic lymphangiomas which involve head, neck, tongue and oral cavity is always done by surgical excisions [1,3,6,7]. As lymphangiomas are benign lesions, the vital structures should not be sacrificed during their surgical resections [1–3, 7]. Many times, it may not be possible to completely excise the lymphangiomas in a single sitting and it may require more additional operations [1,7]. Recurrences are also reported to occur in 5-15% of the cases and additional operations may be required for the excisions of the recurrent lymphangiomatous cysts [1,7]. In present case, it was possible to completely excise the lymphangioma during first operation, without sacrificing any vital structures. A follow-up at two months after operation showed no recurrence and there was only a good post-operative scar that was cosmetically acceptable to the parents of the child.
Giant cystic lymphangiomas of neck, head and oral cavity can be successfully managed by surgery, with satisfactory results, although extreme precaution must be undertaken during complete excisions [1,3,7].
[1]. Fonkalsrud EW, Lymphatic disorders. In: Grosfeld Jay L, O’Neill JA, Fonkalsrud EW, Coran AG (eds)Pediatric Surgery. Chapter 133 2006 2Ed 6thMosby Inc.:2137-46. [Google Scholar]
[2]. Mirza B, Ijaz L, Saleem M, Sharif M, Sheikh A, Cystic hygroma: An overviewJ Cutan Aesthet Surg 2010 3:139-44. [Google Scholar]
[3]. Liu DK, Ma YC, Guo XN, Zhu XS, Dong CX, Surgical treatment of cervical giant cystic lymphangioma in childrenZhonghua Zheng Xing Wai Ke Za Zhi 2011 27:415-17. [Google Scholar]
[4]. Kushwaha AS, Ghritlaharey RK, Budhwani KS, Chanchlani R, Nanda M, Giant retroperitoneal cystic lymphangioma in a seven-months-old girlJ Indian Assoc Paediatr Surg 2007 12:161-6. [Google Scholar]
[5]. Rani DV, Srilakshmi R, Malathi S, Raghupathy V, Bagdi RK, Unusual presentation of a retroperitoneal lymphangiomaIndian J Paediatr 2006 73:617-18. [Google Scholar]
[6]. Kaur N, Gupta A, Amratash Singh N, Giant cystic hygroma of the neck with spontaneous ruptureJ Indian Assoc Paediatr Surg 2007 12:154-55. [Google Scholar]
[7]. Seashore JH, Gardiner LJ, Ariyan S, Management of giant cystic hygromas in infantsAm J Surg 1985 149:459-65. [Google Scholar]
[8]. Benacerraf BR, Nyberg DA, The face and Neck. In: Nyberg DA, McGahan JP, Pretorius DH, Pilu G (eds)Diagnostic imaging of fetal anomalies. Chapter 8 2003 Lippincott Williams and Wilkins:335-80. [Google Scholar]