A Non–Resolving Consolidation which was Caused by a Bronchial Foreign Body in an Adult: A Case Report
Gyanshankar Mishra1, Jasmin Mulani2
1 Assistant Professor, Department of Pulmonary Medicine, Government Medical College, Nagpur, India.
2 Chief Medical Officer, Central Prison Hospital, Nagpur, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Gyanshankar Mishra, Assistant Professor, Department of Pulmonary Medicine, Government Medical College, Nagpur, Maharashtra, India-440003.
Phone: 91-9850349074, Email: gpmishra81@gmail.com
A fifty year old female presented with cough, breathlessness and chest pain of eighteen months duration. She presented as a case of a non–resolving consolidation. Video bronchoscopy revealed a bronchial foreign body. This case is being reported here, to underline the role of bronchoscopy in a case of a non resolving consolidation.
Non–resolving consolidation, Bronchial foreign body, Video bronchoscopy, Betel nut, Adult bronchial foreign body, Bronchoscopic extraction of a tracheo bronchial foreign body
Case Report
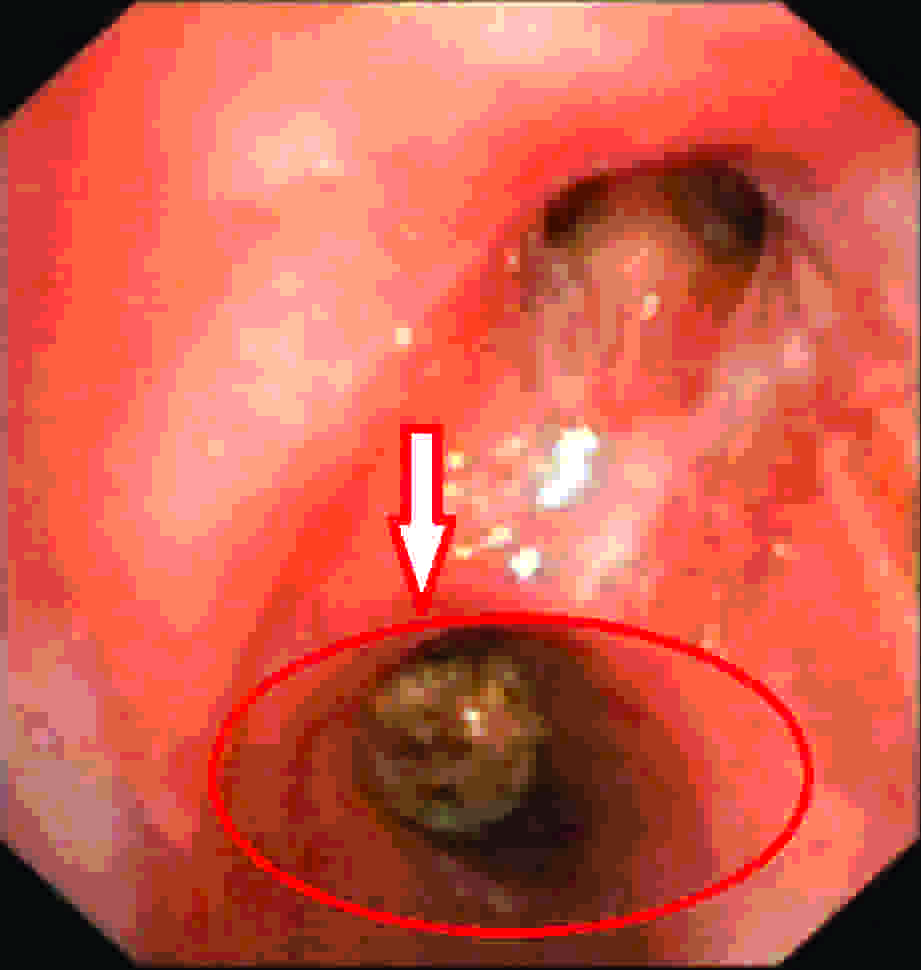
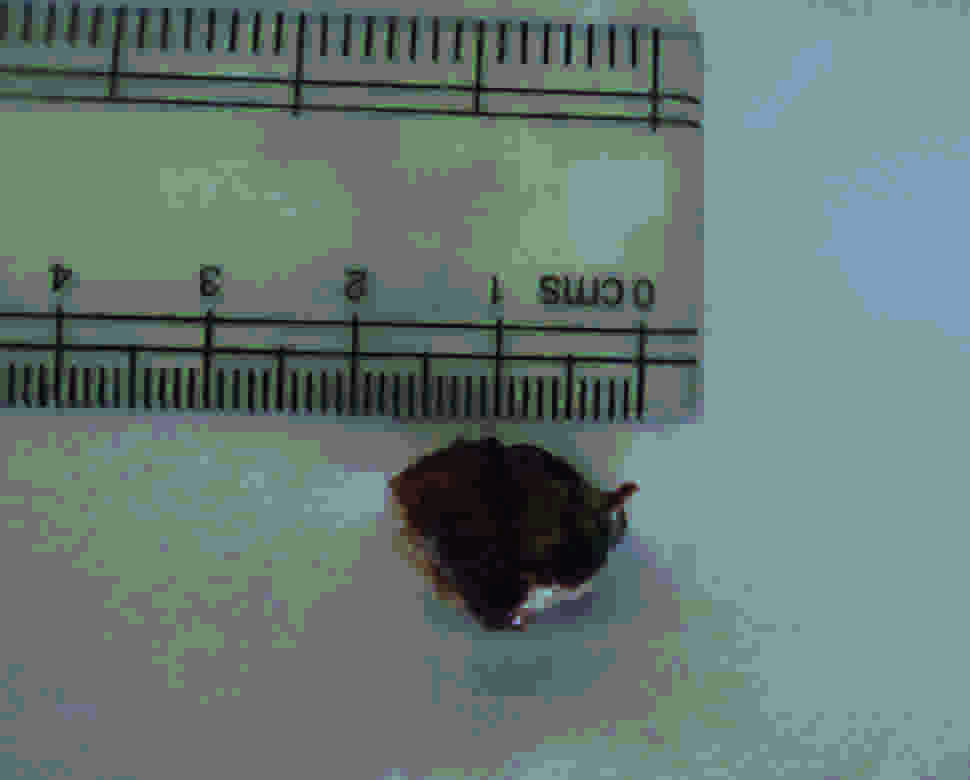
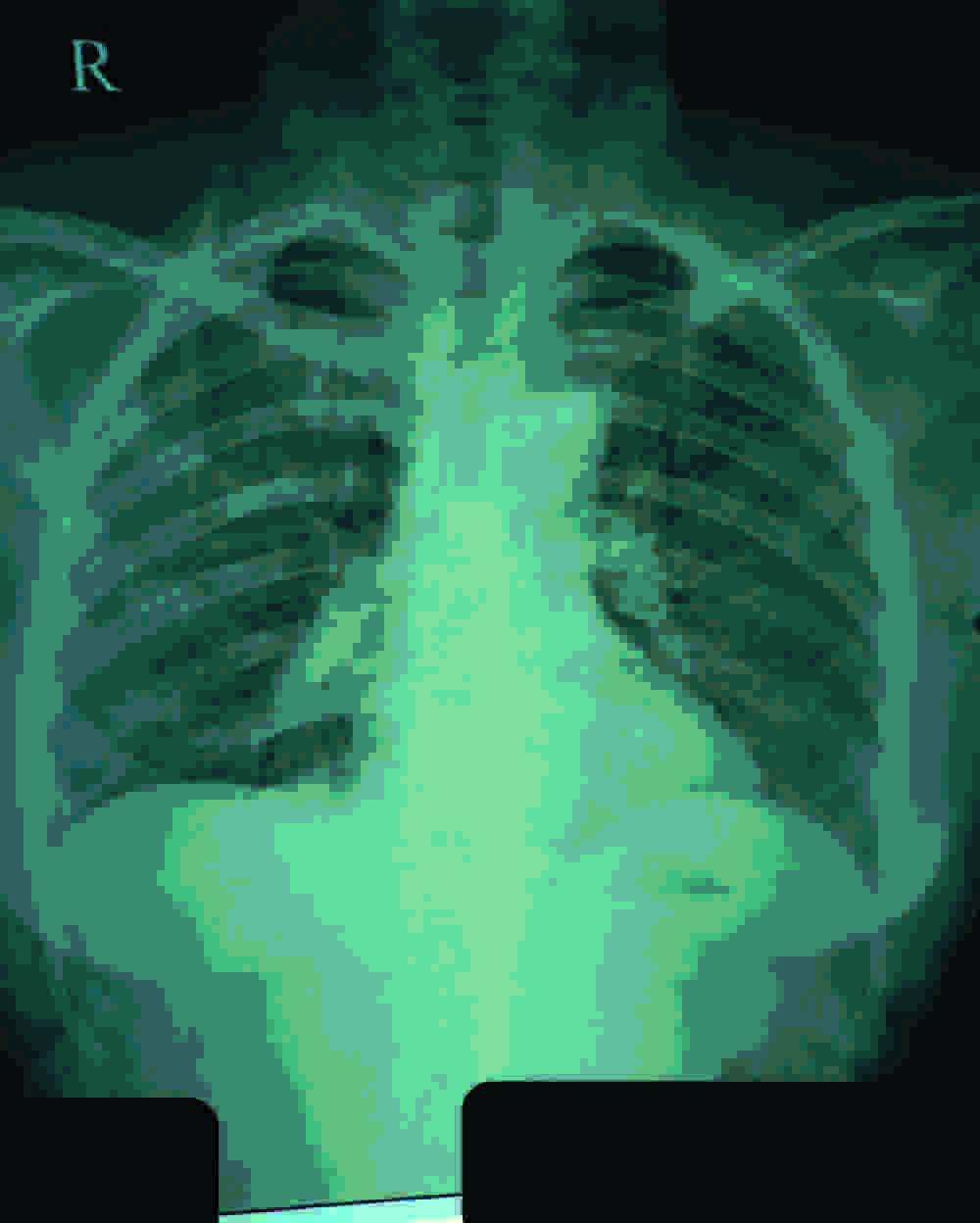
A fifty year old, married female who came from a rural household, presented to the outdoor patients department with the complaints of cough with a scanty white mucoid expectoration, exertional breathlessness and a right sided, dull aching, continuous chest pain of eighteen months duration. Also, there was associated fever on and off. There was no history of constitutional symptoms like anorexia or weight loss. There was no history of haemoptysis or wheezing episodes. There was a history of a violent bout of cough eighteen months back, after which the clinical complaints had followed. The patient had been evaluated by her family physician and she had received trials of antibiotics, to which she had not responded clinically. She was sputum AFB (Acid Fast Bacilli) smear negative and her chest radiograph had shown right lower zone reticular opacities at that point of time [Table/Fig-1]. Finally, based on her clinico-radiological profile and her non– response to antibiotics, she was started on daily anti–tubercular chemotherapy. After 5 months of taking the anti–tubercular chemotherapy, it was found that there was no improvement in the clinico-radiological profile of the patient. At this time, she was referred to our outdoor patients department in the Pulmonary Medicine Department. After a review of her history, she was subjected to a clinical examination, which revealed that she was haemodynamically stable (afebrile, pulse – 98/minute, blood pressure – 120/84 mm of Hg., respiratory rate – 22/minute and oxygen saturation at room air (SpO2) – 97%). Her oral hygiene was poor, with several teeth missing. Her respiratory system examination revealed decreased vesicular breath sounds in the right infra scapular and the infra axillary areas. The investigations that she underwent, showed the following: Total laeukocyte count: 8000/mm3 and Differential leukocyte count: neutrophils-60%, lymphocytes – 33%, eosinophils-4% and monocytes-3%. The platelets were adequate and no parasite was seen on her peripheral smears. Her liver function tests and renal function tests were normal. Her random blood sugar was 102 mg%. Her sputum AFB smear and culture, as well as gram staining and culture were negative. Her chest X-ray, at this stage, revealed right lower zone confluent opacities, with an elevated right hemidiaphragm [Table/Fig-2]. Plain and contrast HRCT (High Resolution Computed Tomography) scans of the thorax revealed confluent alveolar opacities in the right middle and the lower lobes, with pretracheal, subcarinal and right hilar lymphadenopathy [Table/Fig-3]. Thus, this seemed to be a case of a non–resolving consolidation and finally, a flexible video bronchoscopy was planned. The bronchoscopy revealed a brownish, mobile mass which was covered with thick mucus secretions in the right bronchus intermedius [Table/Fig-4]. The mucus secretions were aspirated and the bronchial washings were collected for investigations. The foreign body (1cm x 1.8 cm) was removed en block [Table/Fig-5] with the help of basket forceps [Table/Fig-6], at the distal end of the video bronchoscope. A check bronchoscopy was performed after the procedure and it showed patent airways distal to the right bronchus intermedius (the site of the removed foreign body) i.e. the right middle lobe bronchus and the right lower lobe bronchus. The histopathology of the removed foreign body was suggestive of vegetable matter. The bronchial wash was negative for the AFB staining and culture, as well as for gram staining and culture. The KOH mount did not show any fungal element. The bronchial wash cytology smear revealed acute inflammatory cells along with fibrinous and mucoid debris, which showed degenerative changes.
Chest X-ray showing right lower zone reticular opacities
Chest X-ray showing radiological deterioration & progression of right lower zone confluent radio opacities with elevated right hemi diaphragm
HRCT scan thorax – Confluent alveolar opacities in the right middle and lower lobes
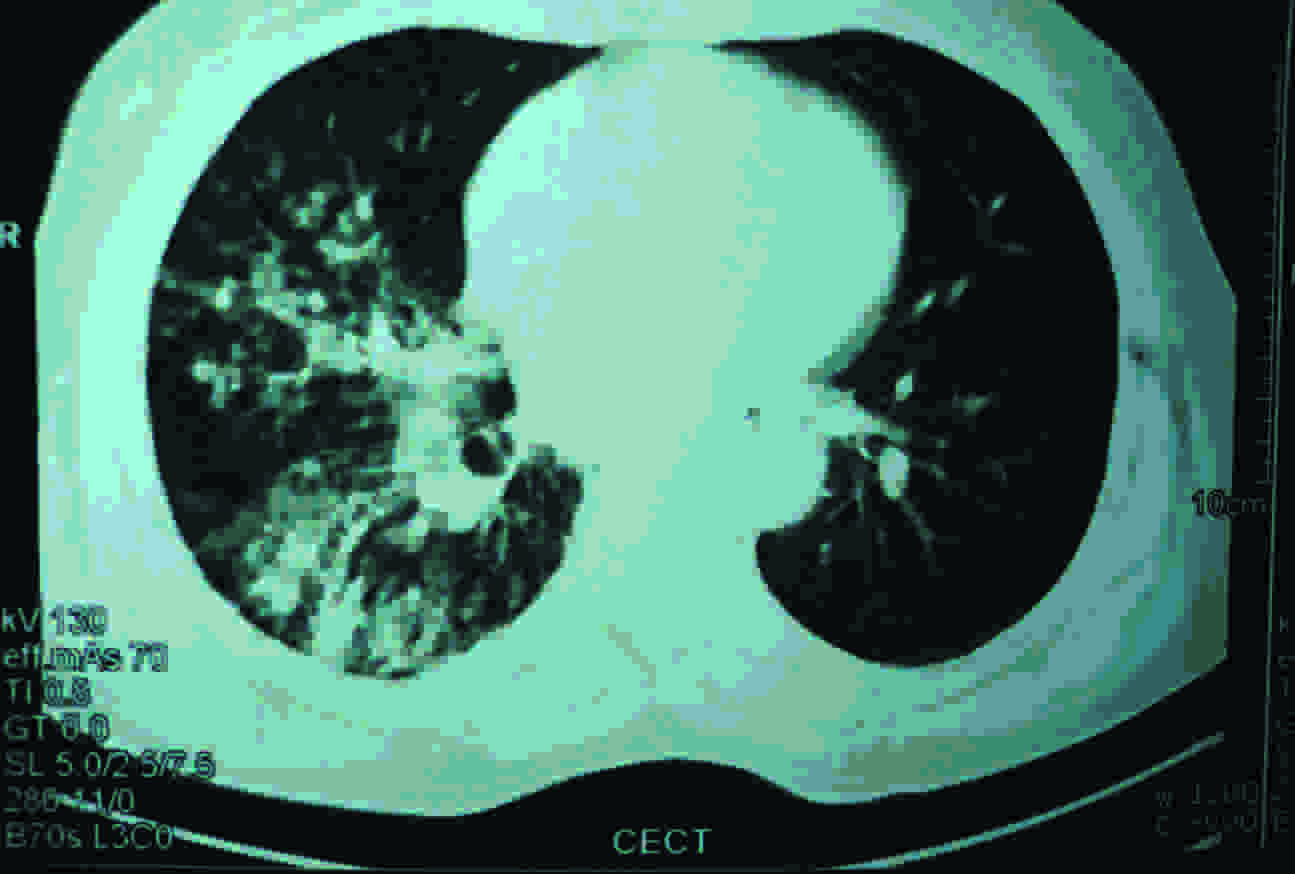
Image of Video Bronchoscopy - Foreign body in right bronchus intermedius
Bronchial foreign body removed via flexible video bronchoscope
Bronchoscopy basket forceps used for bronchial foreign body removal

In view of the bronchoscopy results, the patient was again questioned in detail regarding the history of a probable previous aspiration and she revealed that there was a probability of her having aspirated for removing a betel nut eighteen months back, since she had the habit of regular betel nut chewing.
The patient was administered a four week course of antibiotics and cough expectorants and she was advised chest physiotherapy after the procedure. A repeat chest X-ray, which was done four weeks after the procedure showed a significant radiological resolution of the right lower zone opacities [Table/Fig-7].
Chest X- ray after 1 month of foreign body removal showing radiological resolution of right lower zone radio opacities
Discussion
Although foreign bodies which are present in the tracheobronchial tree are rare in adults, clinicians must be aware of their likelihood. Long standing, retained and neglected foreign bodies which are present in the tracheo bronchial tree are uncommon. In such cases, one has to be careful, because of the possibility of complications like pulmonary infections, lung collapse, lung abscesses and malignant transformation [1].
Retrospectively, the points which favoured the diagnosis of a tracheobronchial foreign body in the present case, were as follows:
A history of a vigorous bout of coughing, following which the clinical symptoms were initiated.
No response to antibiotics or the anti-tubercular treatment.
Serial chest X-rays showed a progressive deterioration of the radiological shadows and later, the X-rays showed a raised, right hemidiaphragm, which gave a subtle clue that the pathology could be intra–bronchial, which had caused an incomplete collapse of the right middle and the lower lobes.
The foreign body was not radio opaque and hence, it was difficult to pick on the plain chest radiographs. However, the HRCT scan of the thorax showed impacted mucoid secretions in the right bronchus intermedius and the radiolucent spherical foreign body was visible in the right bronchus intermedius on retrospective analysis of the HRCT scan of the thorax.
On examination, the patient was found to have several missing teeth, which is a risk factor for aspiration.
The breath sounds were decreased at the right lung bases.
The diagnosis was finally confirmed on bronchoscopy, the indication being a case of a non–resolving consolidation.
One of the aspects of this case was starting with the anti-tubercular therapy empirically on a clinico-radiological basis. It is advocated that prior to the initiation of the anti-tubercular treatment in the sputum smear negative cases, the patient should be subjected to a diagnostic bronchoscopy for the diagnosis of tuberculosis, either through a broncho alveolar lavage or a trans-bronchial lung biopsy examination and cultures. If the patient had been referred at an earlier stage to the tertiary centre, then her condition could have been diagnosed at an earlier stage.
An empirical anti-tubercular treatment exposes the patient to potential adverse effects like drug induced hepatitis and drug induced gastritis [2]. This can be prevented at the outset itself, if an alternative diagnosis is confirmed, thereby abolishing the need to initiate an empirical anti-tubercular treatment.
Also, now-a-days, virtual bronchoscopy through 3D reconstruction algorithms, along with an HRCT scan of the thorax is useful in such cases of intrabronchial obstruction [3].
Traditionally, rigid bronchoscopy has been the preferred tool for the removal of tracheo bronchial foreign bodies. However, fiberoptic / video bronchoscopes have been utilized on occasions to remove them. In fact, Mise et al., in their study, have shown that tracheobronchial foreign bodies can be successfully and safely removed in a majority of the patients under local anaesthesia by using flexible bronchoscopes [4].
Thus, this case reiterates the importance of bronchoscopy in the cases of non–resolving consolidation. The patients of non–resolving consolidation need to be recognized at the primary healthcare level and an early referral of these patients for further evaluation at higher centres is recommended. Bronchoscopy is a very useful diagnostic as well as a therapeutic tool in such cases.
[1]. Vithalani P.D., Maniyar H., An Overlooked Bronchial Foreign Body In AdultIndian Journal of Otolaryngology and Head and Neck Surgery 10/2005 57(4):335-7.DOI:10.1007/BF02907705 [Google Scholar]
[2]. Kumar R, Empirical use of antituberculosis drugs should not be equated to their inappropriate and indiscriminate useIndian J Pharmacol 2011 43:363-4. [Google Scholar]
[3]. Allah MF, Hussein SR, El-Asmar AB, Zoair HM, Mohamed GA, Metwaly AM, Abboud MA, Shalan IM, Role of virtual bronchoscopy in the evaluation of bronchial lesionsJ Comput Assist Tomogr 2012 Jan-Feb 36(1):94-9. [Google Scholar]
[4]. Mise K, Jurcev Savicevic A, Pavlov N, Jankovic S, Removal of tracheobronchial foreign bodies in adults using flexible bronchoscopy: experience 1995-2006Surg Endosc 2009 Jun 23(6):1360-4.doi: 10.1007/s00464-008-0181-9 [Google Scholar]