Haemolymphangioma of Epiglottis
S. Sundarapandian1, Hafida K. Mohamed2, S. Murugesan3, Aberna V.4
1 Assistant Professor, Department of ENT, Sree Balaji Medical College & Hospital, Chennai, Tamil Nadu, India.
2 Senior PG Resident, Department of ENT, Sree Balaji Medical College & Hospital, Chennai, Tamil Nadu, India.
3 Professor, Department of ENT, Sree Balaji Medical College & Hospital, Chennai, Tamil Nadu, India.
4 Junior PG Resident, Department of ENT, Sree Balaji Medical College & Hospital, Chennai, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORESPONDING AUTHOR: Dr. S. Sundarapandian, 2-Nagarathinammal Street, Janaki Nagar, Valasaravakkam, Chennai, Tamil Nadu, India-600087.
Phone: 9043331545,
E-mail: drsundarapandian@gmail.com
Lymphangiomas are congenital lesions of the lymphatic system which are most commonly found in the head and neck, with over 90 % of lesions manifesting in children who are less than 2 years of age. Haemolymphangiomas are rare variant of lymphangioma, with the presence of red blood cells within the lymphatic channels. Laryngeal sites are usually in continuity with foci of disease in the neck. In general, symptoms are non–specific and they vary with the site and size of the mass. Usually, they occur before 2 years of age. Isolated cases of lymphangiomas with involvement of epiglottis are rare and only a few cases have been reported so far. We are reporting the case of a six-year-old girl who presented with a mass in the epiglottis.
Haemolymphangioma, Epiglottis
Case Report
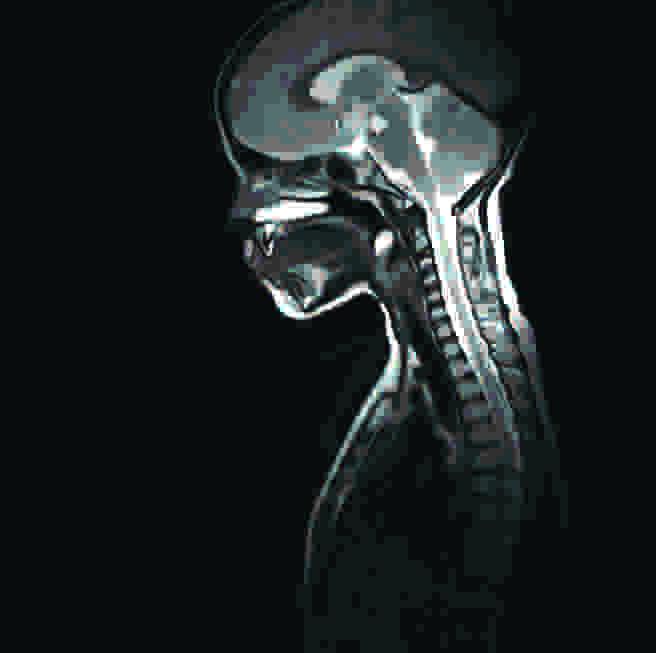
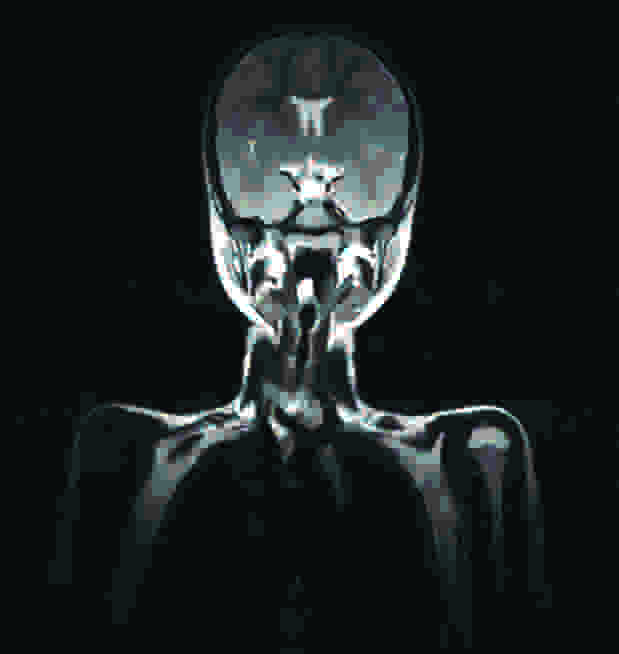
A six-year-old girl presented to the outpatient department with the complaints of a foreign body sensation in the throat, and a mild difficulty in swallowing, of 3 months duration. It was not associated with any breathing difficulties. Her parents gave a history of ingestion of a fish bone, which was manually expelled by them, when the child was one year of age. The patient was not symptomatic at that time and nature of injury was not known. On examination of the girl, her voice was found to be normal and there was no stridor. No foreign body was visualized. The neck, nose and oropharyngeal examinations were normal. On indirect laryngoscopy and video laryngoscopic examinations, it was found that there was a smooth globular pinkish mass which was about 2 cm in diameter, at the right side of epiglottis, with a broad base attachment to the lingual surface of the epiglottis. The other parts of larynx and hypopharynx were found to be normal. MRI of the neck was done and it showed a T2 hyper intense lesion at the level of epiglottis, with no invasion into surrounding structures, which was suggestive of an epiglottic cyst with a protenacious content.
Image of Video Laryngoscopy showing globular pinkish mass on the right side of epiglottis with broad based attachement to lingual surface of epiglottis.

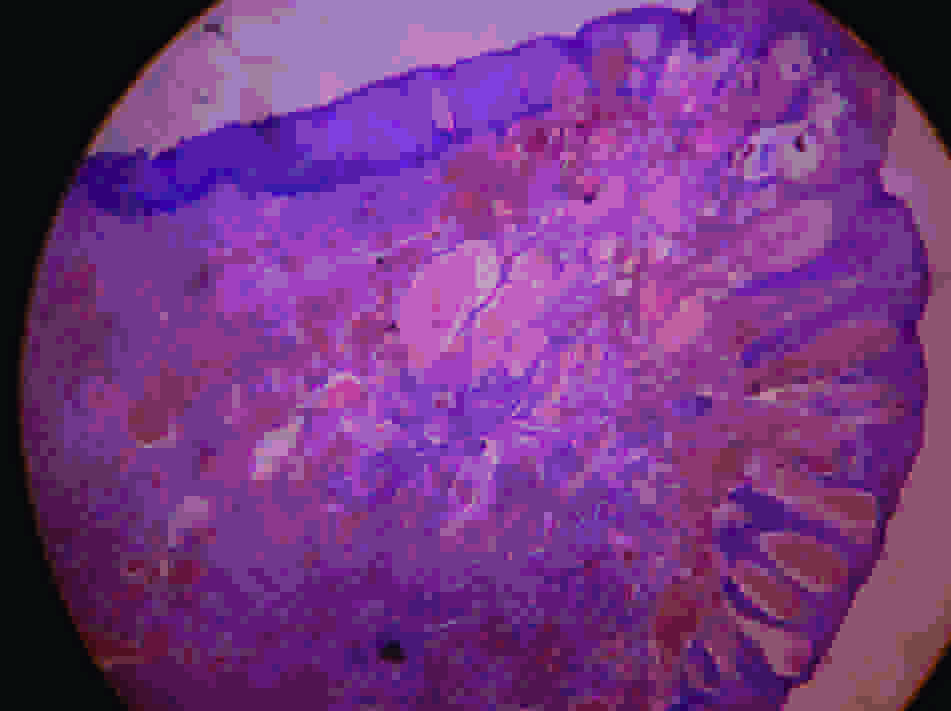
Under GA, by using a nasal intubation, patient was put in the tonsillectomy position with a Boyles Davis mouth gag and under an endoscopic visualization, the base was infiltrated with 2% xylocaine and the mass was completely excised by microscissors and cup forceps, while preserving the epiglottic cartilage, with minimal blood loss. In microscopic sections with hematoxylin-eosin staining, the sections showed a stratified squamous epithelium which overlay a subepithelium which contained ectatic vascular channels of varying sizes, some of which contained erythrocytes and others which contained pale eosinophilic material. The intervening stroma showed lymphoid infiltrates and red blood cells within the lymphatic spaces. The impression was consistent with that of a haemolymphangioma of epiglottis lesion [Table/Fig-1,Table/Fig-2,Table/Fig-3,Table/Fig4].
The section shows stratified squamous epithelium overlying a subepithelium which contained ectatic vascular channels of varying size, some of which contained erythrocytes and others pale eosinophilic material. The intervening stroma showed some lymphoid infiltrates, red blood cells within the lymphatic spaces. The impression was consistent with a haemolymphangioma ,right epiglottic lesion.
MRI neck: t2 sagittal section showing hyperintense lesion at the level of epiglottis, well defined homogenous lesion. No compression of sorrounding structures.
MRI neck: t2 coronal cut showing hyperintense lesion at the level of epiglottis, well defined homogenous lesion. No compression of sorrounding structures.
Discussion
A haemolymphangioma is the fouth variant of a lymphangioma [1].Lymphangiomas are uncommon, benign tumours of the lymphatic system. Some authors consider lympangiomas to be vascular anomalies and not true neoplasms [2]. About 90% of them manifest by 2 years of age.
Age at presentation: 60 % at birth, 75% present by 1 year of age and 90% present by 2 years of age. However, some may present themselves much later in life [3]. Traditionally, they are classified as capillary, cavernous and cystic types on the basis of the size of the lymphatic spaces. Generally, these three types coexist within a single lesion [4].
Cavernous lymphangiomas are more common than capillary types. Common sites are the region of head and neck or axilla. A large cystic variety which is called cystic hygroma occurs in the neck, which produces gross deformities in the neck.
Cohen and Thompson [5], in their extensive review on paediatric lymphangiomas in 160 patients, found involvement of the larynx in ten patients.
Lymphangiomas which involve the larynx are either extensions of the cervicofacial lesions or they extend to involve the neck and other areas. . Isolated laryngeal lymphangioma is a rare form of the lesion [5,6] with only a few cases being reported in the literature.Kenton et al., [7] reported the case of a neonate with lymphangioma of the larynx, who presented with stridor and a progressive respiratory failure. They gave a review of seven cases of laryngeal lymphangiomas, which have been reported so far in the literature. Only two of these seven cases were young adults. The remainder were all less than 2 years of age. However, haemolymphangiomas in epiglottis have not been reported so far. In our case, age of the child was 6 years at the time of presentation. It could have been an acquired lymphangioma which was caused by an inflammatory response to the trauma which was caused by a foreign body.
Lymphangiomas present with symptoms, depending upon the site of involvement and the size of the mass. Cystic hygroma of the neck may at times be so extensive, so as to lead to symptoms of airway obstruction. Lymphangiomas which are localized to the larynx, present with symptoms which are similar to those of other benign tumours of the larynx, such as a change in voice, airway obstruction and stridor, if it is an extensive disease. In our case, the patient presented with only a foreign body sensation in throat and a mild difficulty in swallowing. She was not in stridor.
Lymphangiomas are diagnosed on the basis of history, examination findings and radiological investigations. Magnetic resonance imaging can demarcate the mass from the surrounding tissues and it can give the extent of the lesion.
Various treatment options of haemolymphangiomas, namely surgical excision; laser debulking, sclerotherapy and corticosteroids, have been outlined [8]. It has been suggested that the desire for a complete excision must be weighed against the need to keep vital structures intact. 75% of the patients in a series of sixty seven children with lymphangiomas of the head and neck [8] underwent surgical excisions. It was found that lesions which involved the lip, hypopharynx and/or larynx, tongue and floor of mouth had high rates of recurrent or persistent disease. If the larynx was involved, a tracheotomy was almost always required [5]. The surgical laser is considered to be particularly suitable for a lesion in the larynx, because it allows precise ablation and recontouring of the tissue, so that the functions can be preserved [6]. Sclerosing agents are under investigation for laryngeal lymphangiomas, but since they act by causing inflammatory reactions, their use can result in a damage to adjacent structures. Radiotherapy is not effective in treatment of these lesions [9].
As there have been no controlled trials which have compared the various treatment modalities, the management should be decided on the basis of the extent of the lesion and the site of the lesion. Even with complete excisions, the recurrence rates of these lesions are high. The predicted prognosis is poor, if there is extensive infiltration of upper airway and oesophageal structures, as was seen by Hartl et al., [10]. In our case, we were able to excise the lesion without causing any damage to surrounding vital anatomical structures of the larynx, by using an endoscopic approach.
Conclusion
We reported this case because of the unusual site of involvement; and unusual age of presentation. Although it is rare in occurrence, the otolaryngologists should keep in mind the diagnosis of a haemolymphangioma in the larynx amongst other benign lesions, so that it is detected at an early stage, bearing in mind the further consequences of this disease, if it gets infected or becomes bigger in size.
[1]. Giguère CM, Bauman NM, Smith RJ, New treatment options for lymphangioma in infants and childrenThe Annals of Otology, Rhinology, and Laryngology December 2002 111(12 Pt 1):1066-75.PMID 12498366 [Google Scholar]
[2]. Holinger PH, Johonston KC, Benign tumors of the larynxAnn Otol Rhinol Laryngol 1951 60:496-509. [Google Scholar]
[3]. Naito K, Iwata S, Nishimura T, Yagisawa M, Sakurai K, Laryngeal lymphangioma Auris Nasus Laryx 1985 12:111-16. [Google Scholar]
[4]. Bill AH Jr, Sumner DS, A unified concept of lymphangioma and cystic hygromaSurg Gynaecol Obstet 1965 120:79-86. [Google Scholar]
[5]. Cohen SR, Thompson JW, Lymphangiomas of the larynx in infants and children: a survey of pediatric lymphangiomaAnn Otol Rhinol Laryngol 1986 95(suppl 127):1-20.[PubMed] [Google Scholar]
[6]. Papsin BC, Evans JNG, Isolated laryngeal lymphangioma: a rare cause of airway obstruction in infantsJ Laryngol Otol 1996 110:969-72.[PubMed] [Google Scholar]
[7]. Kenton A, Duncan N, Bhakta K, Fernandes CJ, Laryngeal lymphatic malformation in a newbornJ Perinatol 2003 23:567-71.doi: 10.1038/sj.jp.7210942. [PubMed]. [Cross Ref] [Google Scholar]
[8]. Orvidas LJ, Kasperbauer JL, Paediatric lymphangiomas of the head and neckAnn Otol Rhinol Laryngol 2000 109(4):411-21.[PubMed] [Google Scholar]
[9]. Sobol SE, Manoukian JJ, Acute airway obstruction from a laryngeal lymphangioma in a childInt J Pediatr Otorhinolaryngol 2001 58:255-57.doi: 10.1016/S0165-5876(01)00433-5. [PubMed][Cross Ref] [Google Scholar]
[10]. Hartl DM, Roger G, Denoyelle F, Nicollas R, Triglia JM, Garabedian EN, Extensive lymphangioma presenting with upper airway obstructionArch Otolaryngol Head Neck Surg 2000 126:1378-82.[PubMed] [Google Scholar]