Intertrochanteric fractures with severe displacement and comminution are common in elderly patients. These patients have a poor bone quality and the fractures are often associated with complications such as non union, metal failure and femoral head perforation [1,2]. The primary treatment goal is a stable fixation and an immediate full-weight-bearing mobilization [3]. Stable intertrochanteric fractures can easily be treated by osteosynthesis, with predictable good results, whereas the management of unstable intertrochanteric fractures is challenging, because of a poor bone quality, osteoporosis and other underlying diseases.
Excessive collapse, loss of fixation, and cut-out of the lag screw, which result in poor function, remain problems which are associated with the internal fixation of unstable intertrochanteric fractures in elderly patients with osteoporotic bones. To allow an earlier postoperative weight-bearing and a rapid rehabilitation and to avoid excessive collapse at the fracture site, some surgeons have recommended prosthetic replacements for the treatment of unstable intertrochanteric fractures [4–6]. The literature on hemiarthroplasties for unstable intertrochanteric fractures is sparse.
The purpose of this prospective study was to evaluate the functional and clinical outcomes of cemented bipolar hemiarthroplasty as a primary treatment for unstable intertrochanteric fractures in elderly patients.
Material and Methods
Between June 2010 and May 2011, a series of 20 patients who underwent bipolar hemiarthroplasties for unstable intertrochanteric fractures were followed up prospectively. These patients were all above 65 years of age and they had been independently mobile before they had sustained the fractures. Exclusion criteria were patients with compound intertrochanteric fractures, polytrauma patients, patients who were < 65yrs of age and patients who were unfit for surgery.
Preoperative data included: Age, sex, side, fracture type and mode of injury. Post operative data included time to full weight bearing, average hospital stay and complications. This study was approved by the institutional ethics committee. All the patients provided written informed consents.
All surgical procedures were performed by the same surgical team as soon as the conditions of the patients were stabilized, usually within forty-eight hours after their admissions. Preoperative templating of radiographs of the fractured side and contralateral side was performed to determine the approximate size and position of the stem and the approximate femoral neck offset.
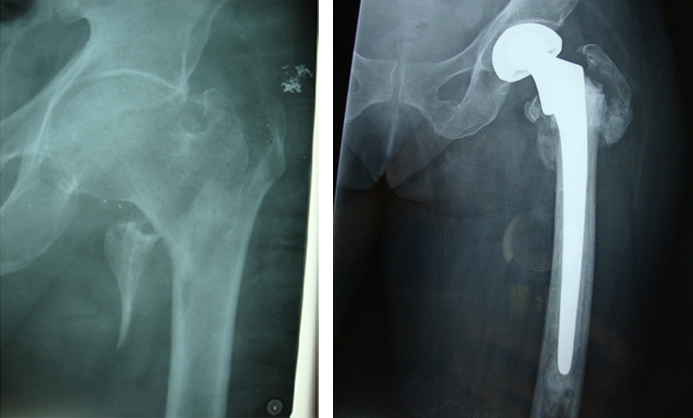
The operation was performed by using Moore’s approach, with the patients in the lateral decubitus position. The femoral head and neck was removed. Meticulous care was taken to preserve the integrity of the greater trochanter, abductor muscles, and all the vascularized bone fragments. The femoral medullary canal was then reamed to the appropriate stem size and diameter. Trial reductions were performed to determine the exact length that would provide the desired tension and tissue balancing of the abductor muscles and an equal leg length. Careful restoration of neck length, offset and version to maximize stability of the hip joint, was also performed during trial. The definitive femoral stem was cemented into the femoral canal with the use of so-called second-generation techniques (medullary lavage, use of an intramedullary cement plug, hand-mixing of cement, use of a cement gun to deliver the cement in a doughy state in a retrograde fashion and to insert antibiotic-impregnated cement in all patients). The lesser trochanter was not removed. Any protrusion of cement between reduced bone fragments was cleaned out. The greater trochanter was reduced and stabilized by using the tension band wiring technique after hip reduction or it was just sutured near the prosthesis. The gluteus medius muscle and vastuslateralis muscle were sutured to their anatomical locations by using anchor sutures, if necessary. Fascia lata was tightly closed over a suction drain. Post-operative radiographs were obtained [Table/Fig-1a and 1b].The sutures were removed on day 12 and the patients were discharged, with printed instruction sheets of dos and don’ts.
Radiographs of right hip of 74 year old male (a) An unstable intertrochanteric fracture. (b) Treated with bipolar hemiarthroplasty
Patients were ambulated full weight bearing on the first post-operative day. They were followed up at 6 weeks, 3 months, 6 months and 12 months. Clinical evaluation was done according to Harris Hip score. Anteroposterior radiographs of the hip were analyzed at each follow up to note any evidence of loosening.
Results
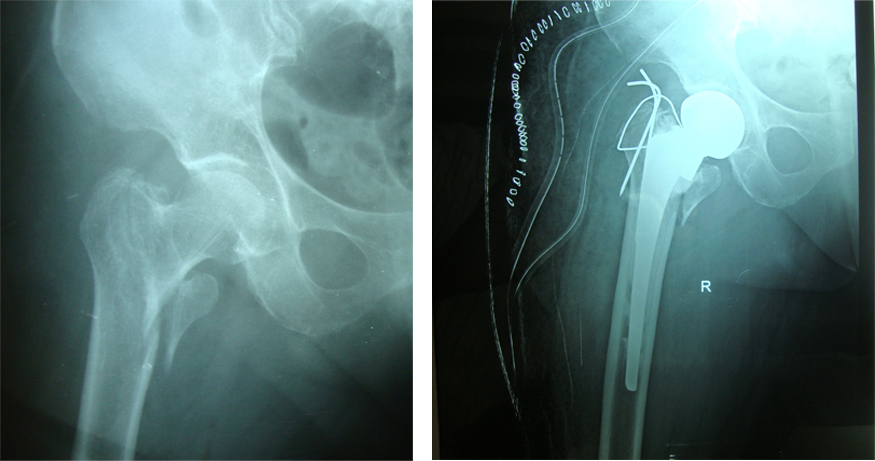
Twenty patients were enrolled in this study. 15 sustained fractures after falls from a standing height, while 5 patients sustained road traffic accidents. The average age at surgery was 72.4 years (range, 65-95). There were 11 men and 9 women. The male to female ration was 1.2:1(55%-45%). 14 patients had type II fractures, 3 had type III fractures, 2 had type I fractures and one had a type IV fracture (Boyd and Griffin’s Classification). Singh’s index (grades of osteoporosis) was grade III in 12 patients and it was grade II in 8 patients. The mean operative time was 116±14 minutes. Greater trochanter was reconstructed in 10 cases (50%) [Table/Fig-2a and 2b].There was one case of a superficial infection and one case of a deep infection.
(a) Pre-operative radiographs (b) treated with bipolar hemiarthroplasty and encirlage wiring for greater trochanter
The mean day for full weight bearing was the 5.4th day. Excellent to fair results were obtained at the final follow-up in 18 (90 %) cases and in 2 (10%) cases, results were poor. Post operatively, 4 patients (20%) had a shortening of less than 2 cm and 2 patients (10%), had a shortening of more than 2 cm. One patient had a lengthening of 1.5cm (5%).
Two patients (10%) had fixed external rotations of the operated limbs, of less than 20 degrees. Two patients (10%) had flexion deformities of than 20 degrees. There was no incidence of postoperative dislocations of the prosthesis in the study. Patients were discharged from the hospital at a mean, on the 13.3th day. Patients were followed up at 6 weeks, 3 months, 6 months and 12 months. The mean time of follow up was 9 months. The mean Harris hip score was 75 points at final follow up, at the end of 12 months . A majority of the patients had a pain free mobile hip with a full range of flexion, abduction and adequate amount of rotations and adduction.
In our study, there was no incidence of loosening of the prosthesis or an acetabular erosion radiologically on follow up. There was no incidence of revision surgeries.
In our study, the final functional results were fair to good according to the Harris hip scoring system, with a mean score of 75%.
Discussion
Complexity of intertrochanteric fractures in elderly osteoporotic patients poses challenging problems, with an added risk of increased morbidity and mortality. Although union rates as high as 100% have been reported in association with well-reduced, stable fractures that were treated with ideal implant placements, failure rates of as high as 56% have been noted in association with unstable fractures, comminutions, suboptimal fracture fixations, or poor bone qualities in elderly patients [7,8]. Although the internal fixation of such fractures may reduce the morbidity of pain, it does not permit an early mobilization with a fear of failure of fixation and thus, indirectly, the morbidity of fracture remains same. Early ambulations following surgeries are important, for preventing complications that can be caused by long term bed rests in elderly patients with poor general conditions.
The poor mechanical properties of the weak and osteoporotic bones in elderly patients do not provide a good purchase for the screws, which subsequently lead to an early biomechanical failure. This leads to a collapse, with migration of the femoral head into the varus and retroversion, resulting in limping, which is caused by shortening and a decreased abductor muscle lever arm [9]. Another complication of internal fixation is that the implant can be cut out from the femoral head, which can lead to profound functional disabilities.
Hemiarthroplasty is a frequently employed alternative, as it gives stability and allows immediate full weigh bearing. Many of the complications of internal fixations can be avoided by performing hemiarthroplasties [10]. Bipolar hemiarthroplasty was introduced to address the complications of unipolar implants like acetabular wear, protrusion, loosening and dislocation. The concept of dual bearing surfaces in prosthesis, offers considerable advantages. It results in sharing of the motion at the two surfaces and hence, it reduces the net wear at either surface, thus reducing erosion at the acetabular joint interface. In addition, the total range of motions at the joint is increased. Stems were designed, more in lines with total hip replacement designs, to lessen component loosening. Cemented fixation is advantageous for achieving the initial implant stability and a rapid rehabilitation.
Tronzo was the first to use long, straight –stemmed prostheses for the primary treatment of intertrochanteric fractures [11]. Following this, other workers also reported good results with the use of the Leinbach prostheses [12]. Liang et al., in their study which was done on unstable intertrochanteric fractures, concluded that hemiarthroplasty was an effective and a safe method for treating unstable intertrochanteric fractures in elderly. It leads to a decrease in complications and mortality [13]. Grimsrud et al., studied 39 consecutive patients with unstable intertrochanteric fractures which were treated with cemented bipolar hemiarthroplasty. Their conclusion was that these fractures could be treated with a standard femoral stem and cerclage cabling of the trochanters [14]. This technique allows a safe and early weight bearing on the injured hip and it has a relatively low rate of complications.
In our series, patients were ambulated full weight bearing on the first post-operative day, so there were no recumbency related complications (eg- bedsores, chest complications, etc) in our patients. Rodop et al., in their study which was done on the use of bipolar hemiarthroplasty for intertrochanteric fractures, obtained 17 45% excellent and 37% good results after a follow up of 12 months, according to Harris hip scoring system. A total of 18 (90%) out of 20 patients in our study had excellent to fair outcomes. Thus, the results of this modality of treatment look promising, especially in view of the variable results of osteosynthesis in this group [15].
Kim and co-workers 15 reviewed 178 inter-trochanteric fractures which were treated by DHS fixation. They used Singh’s index for evaluating degree of osteoporosis and Evans’ classification for assessing stability of fractures. They found failure of fixation in the form of a varus angulation of >100°, perforation of femoral head, more than 20 mm of extrusion of a lag screw or metal failure, in 49 (27%) cases. Among these, 2 fractures were stable, and 47 were unstable. Thus, the conclusion was unstable fractures with osteoporosis had failure ratewa of >50% and that in such cases, dynamic hip screws should not be the first choice of treatment [16].
Reconstruction of greater trochanter is an important step of surgery, for maintaining the stability of hip joint and in this series, encirclage wiring was done in 50% of the patients.
Primary hemiarthroplasty offers a modality of treatment that provides adequate fixation and early mobilization in these patients, thus preventing postoperative complications such as pressure sores, pneumonia, atelectasis, and pseudo arthrosis. Delays in the surgeries are one of the most important predictor of mortality in patients with intertrochanteric fractures and also of the postoperative morbidity. The cornerstone of management of such fractures is early surgery, followed by mobilization. Early mobilization is very essential, particularly in patients with other medical co-morbidities and also to prevent post-operative complications.
Limitations
Due to the small sample size and short follow up, it was not possible to do an analysis on mortality in the current study. However, most of the complications after hemiarthroplasties are rare. This study also had too few patients for doing analyses on rare adverse effects such as infections, dislocations, periprosthetic fractures and loosening of the prostheses. A larger prospective randomized study which compares the use of intramedullary devices against primary hemiarthroplasty for unstable osteoporotic fractures, is needed, to study these concerns.
Conclusion
Osteosynthesis with dynamic hip screw fixations or intramedullary fixations are the most commonly performed operations for intertrochanteric fractures of hip. These fractures are better treated with cemented hemi-arthroplasty than with internal fixation. It has advantage of an early ambulation and less hospital stay. Cemented hemi-arthroplasty also provides stable and mobile hips and revision surgeries is hardly needed in elderly patients.