The T- condylar fracture of the distal humerus is a very rare fracture in the adolescent age group, which accounts for less than 1% of the elbow fractures [1]. A paediatric T–Condylar fracture can sometimes be confused with an extension type supracondylar fracture of the humerus; therefore, good quality radiographs are necessary for making a proper diagnosis and for the treatment. The key to the differentiation between the two is a fracture line which extends into the intercondylar region of the distal humerus. The goal behind the treatment of such fractures is restoration of the articular anatomy of the distal end of the humerus. The treatment depends upon the amount of displacement and the extent of comminution of the articular surface. An open reduction is required when there is a fracture displacement and a marked articular displacement. A closed reduction and a percutaneus Kirchner wire fixation are thought to be sufficient when there is no or minimal displacement of the Condylar region and when the articular surfaces are fairy maintained. A rigid internal fixation with an early mobilization is recommended for the displaced paediatric intercondylar fractures of the humerus, as in adults. Our study presents the experience of closed reductions and percutaneous Kirchner (K) wire fixations, even in displaced intercondylar fractures of the distal humerus in children. As was highlighted by Kundel et al., the overall rate of the complications; like iatrogenic nerve palsies, heterotopic ossifications, deep infections, fixation failures which lead to nonunions/malunions, etc, following open reductions and internal fixations of the intercondylar fractures of the distal humerus can be as high as 22%. No such high rates of the same types of complications have been described in the clinical series in which similar fractures were treated by closed reductions and internal fixations with percutaneus ‘K’ wires.
Material and Methods
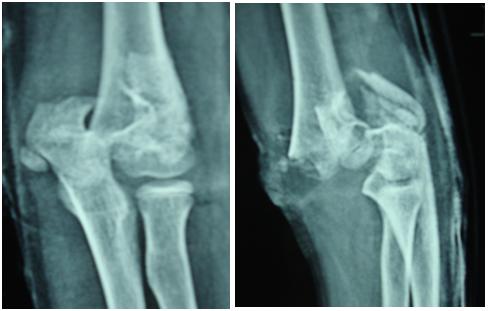
Between June 2008 to December 2011, seven patients (6 males and 1 female) with an average age of 14 years (range 12–16 years) who had intercondylar fracture of the distal humerus were treated at a tertiary health care centre. An institutional ethical committee clearance was obtained before actually starting the study. Patients were recruited in the study only after obtaining informed written consents from them. All the fractures presented within three (range 0–3 days) days of sustaining the injury. After the relevant history was taken, a thorough clinical examination was done, with particular emphasis on the distal neurovascular status. The fractures were the result of falls from a height over the ground, with the elbows flexed and the tips of the olecranons directly coming in contact with the ground. A non–dominant extremity was involved in six (85%) cases and a dominant extremity was injured in one (15%) patient All the patients were investigated by using plain X–rays of the injured elbows, which included the antero-posterior (AP) and the lateral views [Table/Fig-1a and1b]. A CT scan was not required in any case in the present study, due to the clear interpretation of the intercondylar fractures on the plain radiographs. There was a significant intra–articular gap in six cases; one patient had a minimally displaced T–Condylar fracture. The column integrity was assessed before labeling a fracture as an intercondylar fracture of the distal humerus.
Anteroposterior and lateral radiographs of elbow showing interondylar fracture of the humerus
All the patients were operated either under general or regional anaesthesia, depending upon the anaesthetist’s choice. The local part preparation was done just prior to the operation. All the patients were given an injectable broad spectrum antibiotic one hour prior to the surgery. Intraoperatively, no antibiotic was given, because the duration of the procedure was not more than one hour in any case. After adequate anaesthesia was given, the patients were mounted on plain orthopaedic tables in the supine position. No tourniquet was applied in any case. With the patients lying supine on plain operation tables, the limbs which had to be operated were supported on radiolucent side arm rests with a 90 degree abduction at the shoulder joints and flexion at the elbows.
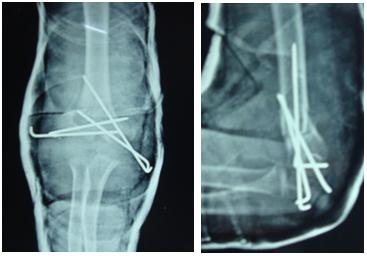
Thereafter, a closed reduction of the intercondylar parts of the fractures was obtained, keeping the elbows of the patients flexed and held with bone holding clamps; the reduction was checked under a C–arm. After the closed reduction, 2.0 mm Kirchner wires were passed horizontally, parallel to the elbow joints, starting from the lateral to the medial epicondyles, thereby converting the intercondylar fractures into two part supracondylar fractures. Two or more 2.0 mm Kirchner wires were passed through the medial and the lateral epicondyles of the humeri into the proximal fragment, to achieve the remaining fixation. While passing the wires from the medial epicondyles, the ulnar nerve was secured by identifying it through stab incision over the medial epicondyles. The final positions of the fractures after the closed reduction and the percutaneus ‘K’ wire fixation were checked under an image intensifier by using the standard radiological criteria. The average operation time was one hour. In all the cases,the ‘K’ wires were left protruding outside the skin at approximately 2 cm. The wires were bent outside. The ‘K’ wires crossed the opposite cortex and they were placed in a criss cross manner. Both a hand drill as well an electric drill were used to insert the ‘K’ wires. Following the surgeries, the elbows were immobilized in above elbow plaster of Paris (pop) splints.
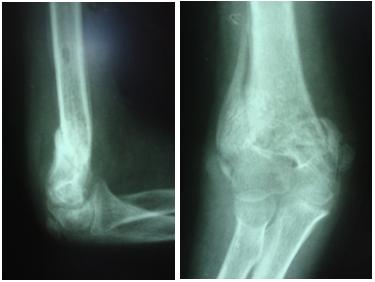
All the patients were discharged from the hospital after the first Check X–ray was taken on the second day after the surgery. Thereafter, the patients were called back at 1 week after the surgery for the first follw-up, to check the maintenance of the reduction by taking check X– rays of the operated elbows, which included the antero–posterior and the lateral views. The second Foolw-up was done at three weeks after the surgery and on the radiological attempts at callus formations [Table/Fig-2a and 2b], the pop splints were removed and cuff and collar slings were given to all the patients alongwith instructions to do gentle elbow exercises. The third follow up was done 5 weeks after the surgery and on a radiological evidence of bridging callus formations, the ‘K’ wires were removed [Table/Fig-3a and 3b].
Postoperative anteroposterior and lateral radiographs showing fixation with ‘k’ wires (3 weeks post-op.), showing radiological callus formation
Anteroposterior radiograph of the elbow showing union of the fracture ( 5weeks post-op.), showing bridging callus
Results
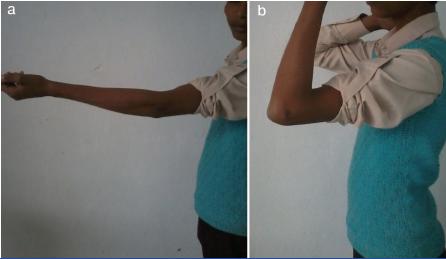
Union of the fracture: It is defined as a radiological evidence of the bridging callus formation, which was achieved in all of our patients, with the average time for the union being 6 weeks (range 5–7weeks). Mild elbow stiffness was seen in three (42%) patients at 5 weeks of follow–up, which was dealt with by planning vigorous physiotherapy schedules after the ‘K’ wire removal. A pin tract infection was seen in one (14%) patient, who was treated successfully conservatively. A consolidated fracture union was seen at an average interval of 3 months after the surgery [Table/Fig-4a and 4b]. At the end of the final follow–up, at 2 years after the surgery, all the patients had a satisfactory range of motion at the elbow joint [Table/Fig-5a and 5b]and they were able to return to their premorbid states. The average Mayo Elbow Performance Score (MEPS) for six patients was 85, which was rated as good; except in one (14%) patient who was lost to follow–up initially, who returned with a painful and a stiff elbow with an MEPS of 40 only [Table/Fig-6].
Anteroposterior and lateral radiograph of elbow 3months after surgery showing consolidated union.

Clinical photographs of the patient showing range of motion at the elbow joint.
Showing MEP score of individual patients
| Serial no. of patient/elbow score pint | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
|---|
| Pain | 30 | 45 | 30 | 30 | 45 | 30 | 15 |
| Motion | 20 | 15 | 15 | 20 | 15 | 20 | 05 |
| Stability | 10 | 10 | 10 | 10 | 10 | 10 | 10 |
| Function of elbow | 25 | 20 | 25 | 25 | 20 | 25 | 10 |
| Total score of individual patient | 85 | 90 | 80 | 85 | 90 | 85 | 40 |
There were no growth disturbances. There was no functional disability [Table/Fig-7].
Showing various complications in the patients
| Complication | No. of patients | % |
|---|
| Nonunion | 0 | 0 |
| Malunion | 0 | 0 |
| Deep infection/draining sinus | 0 | |
| Growth disturbance | 0 | 0 |
| Elbow instability | 0 | 0 |
| Nerve injury | 0 | 0 |
| Early Fixation failure | 0 | 0 |
| Mild elbow stiffness | 3 | 42 |
| Severe elbow stiffness | 1 | 14 |
| Heterotopic ossification | 0 | 0 |
There were no complications like an early fixation failure, an iatrogenic neurovascular injury, growth disturbances and instability at the elbow joint.
Discussion
No large report series are available for the exact treatment plans and the outcomes of paediatric T- condylar fractures of distal humerus. The ideal treatment for a paediatric T– Condylar fracture of the humerus is open reduction and internal fixation with plates and screws, to allow an early mobilization of elbow, to prevent elbow stiffness. However, the treatment options may vary, depending upon the amount of displacement of the Condylar pillars, the extent of the comminution and the integrity of the articular surfaces. Most of the surgeons agree that when the integrity of the columns is maintained, thus allowing a stable fracture pattern and when the articular surface is undisturbed, then such paediatric inter-condylar fractures can be simply treated conservatively with excellent results [2]. The difference of opinion mainly lies in the management of the increasingly displaced and the comminuted fractures [3]. Some authors say that even the displaced paediatric intercondylar fractures can be treated by closed reductions and percutaneus pinning, with satisfactory functional results [3,4]. Others say that the ideal treatment for a displaced intercondylar fracture is open surgical reduction and internal fixation with reconstruction plates, so as to allow an early elbow mobilization, to prevent elbow stiffness, as has been mentioned earlier [5–7]. But at the same time, an open surgical reduction leads to more injury to the surrounding soft tissues and it increases the risk of elbow stiffness [8–10]. In our study, the union rate was 100% and there was no need of carrying out a secondary surgical procedure for a failed implant/or to remove the ‘K’ wires from the elbow. In the study which was conducted by Kundel et al., who treated distal humeral intercondylar fractures by open reductions and internal fixations by using plates; only 52% cases were found to have good to excellent results. Kundel et al., observed iatrogenic nerve injuries in 16% cases, heterotopic bone formations in 49% cases, deep infections which included draining sinuses in 8% cases, and fixation failures which led to revision surgeries in 5% cases. In our study, there were no such complications and 85% of the patients had good functional results. The technique that we have chose was fairly simple and it can be done by the most average orthopaedic surgeon. With a closed reduction and a percutaneous pinning, there is no iatrogenic trauma to the surrounding soft tissues, particularly the extensor mechanism at the elbow joint, which could lead to subsequent elbow stiffness. There is no complication which is related to bulky hardware like impingement and pain in the soft tissues and skin necrosis. There is no need of carrying out another surgical procedure to remove the pins, because these can be removed very easily as an outdoor procedure, which decreases the risk of surgical and anaesthetic risks to the patient and it is also very cost effective. Moreover, the surgical time is very less as compared to that of the open surgical reduction of the fracture. The major limitation of the present study was that it was uncontrolled in nature and that it involved a smaller number of patients. The use of physician based assessment criteria was another limitation of the present study.
Conclusion
The present study concludes that even displaced paediatric intercondylar fractures of the distal humerus can be satisfactorily treated with closed reductions and percutaneous pinning.