Hyponatraemia is one of the most common electrolyte disorders which are encountered with carcinoma [1]. It occurs at presentation in approximately 15% of the patients with small cell lung cancer and in 1% of the patients with non-small cell lung cancer [2]. The principle cause of hyponatraemia in malignancy is the syndrome of inappropriate anti-diuretic hormone secretion (SIADH). An early recognition and a prompt treatment of the electrolytic imbalance can prevent a serious neurologic sequel [3]. The degree of hyponatraemia and its normalization can modify the median survival and thus, it can serve as a relevant prognostic marker of the survival in lung cancer [4–6]. The Eastern Co-operative Oncology Group (ECOG) score correlated with the duration of the patient survival and the response to treatment, as well as their quality of life and co-morbidity [7–10]. To the best of our knowledge, only limited studies have been conducted in India, which have estimated the incidence of hyponatraemia in lung cancer and it’s effect on the ECOG performance status. We conducted this study to estimate the incidence of hyponatraemia among the patients of lung cancer and to check for the effect on their ECOG performance statuses.
Material and Methods
This cross-sectional, observational study was conducted in our medical college during the period from November 2011 to October 2012. The study population was selected from among 116 consecutive patients of lung cancer, who attended our Chest Medicine Department. The aim of our study was to detect the incidence of hyponatrsemia among the patients of carcinoma of the lung before putting them into specific treatment categories for cancer and to see their effects upon their ECOG performance statuses. The specific objectives of our study were to detect the incidence of hyponatraemia in the patients of carcinoma of the lung at the time of presentation, the effect of hyponatraemia after their correction over ECOG performance status and the association of hyponatraemia with the hypo-osmolarity of the serum.
The subjects who were enrolled in the study were both male and females who were histologically confirmed cases of lung cancer, who were above 18-years of age. The patients who received prior anti-cancer therapy for lung cancer, those who were suffering from or who were known to have diabetes mellitus, thyroid disorders, cardiac diseases, chronic liver diseases, renal diseases, tuberculosis and the HIV infection, the patients who were on a long term steroid therapy or on drugs (ex–diuretic) which were known to cause serum sodium disturbances, pregnant women and those who were unwilling to give their consents were excluded from our study.
A detailed history which included the demography and the smoking status was taken initially for each patient. The ECOG performance status was assessed at presentation before getting any specific form of therapy which was meant for lung cancer (i.e. surgery/chemotherapy/radiotherapy) [11]. The patients were grouped according to their performance statuses as ECOG 0, ECOG1, ECOG 2, ECOG 3, ECOG 4 and ECOG 5 at the time of their presentation. Again, the ECOG performance status score was assessed after the correction of the electrolytes, only for those patients who showed hyponatraemia in their initial serum estimation. A tissue diagnosis of bronchogenic carcinoma was made by doing procedures like image-guided Fine Needle Aspiration Cytology (FNAC) and true–cut needle biopsy on peripheral lung masses and fibre-optic bron–choscopy guided biopsy for the centrally located lung masses. FNACs from the accessible and clinically palpable lymph nodes, pleural fluid studies and blind and video-assisted thoracoscopic pleural biopsies were also done as were required, to aid in the tissue diagnosis. The lung cancer patients were histologically classified into the Small Cell Lung Carcinoma (SCLC) and the Non–Small Cell Lung Carcinoma (NSCLC) types and into their subtypes, namely, Squamous Cell Carcinoma (SCC), adenocarcinoma and large cell carcinoma. Any mixed or uncommon types of NSCLC were termed as “other” in our study.
The NSCLC cases were staged according to the TNM classification [12] and the SCLC cases were staged clinically as limited disease (LD) (limited to one hemithorax, which included supraclavicular and mediastinal lymphadenopathy) or Extensive Disease (ED).
The complete blood count, fasting blood sugar, serum sodium, urea and creatinine and liver function tests were done for each of the patients. Venous blood was drawn aseptically by ante-cubital vein puncture slowly after 12 hours of fasting by using a 10 ml disposable plastic sterile syringe and it was dispensed into plastic vials for analysis.
Serum sodium was analysed by using an Easylyte–Plus analyzer machine. Blood sugar, urea and creatinine and the liver function tests were analysed by using a full auto-analyzer, ERBAXL-600. A complete haemogram which was done, was analysed by using a SYSMEX analyzer auto machine. Sputum examinations for acid-fast bacilli and malignant cells were also done. Serum sodium which was in the range of 135–145 meq/l was taken as normal in our study [13]. The hyponatraemia was classified as mild (131–134 meq/l), moderate (126–130meq/l) and severe (<126 meq/l). The ECOG statuses of the hyponatraemic patients were again reassessed after the treatment, to observe any changes in the ECOG statuses from their initial ECOG status scores at the time of their admissions. They were noted and recorded under the heading of ‘ECOG after correction’ in our data base.
The asymptomatic and the mild to moderate hyponatraemia cases were treated with a water restriction of 500–1000 ml per day as the initial treatment. The treatment plan for the severe hyponatraemic or symptomatic cases was an intravenous infusion of hypertonic (3%) saline (100 ml) over 4 hours, with monitoring of the serum Sodium twice daily. The rate of correction of serum sodium was slow and it was limited to 2 meq/l per hour or a maximum of 20 meq/l per day, until a serum sodium level of 135 meq/l was achieved [13,14]. The serum osmolarity was calculated on the basis of the fasting blood sugar, the serum blood urea nitrogen (BUN) and the initial serum sodium value. Serum BUN is calculated from the serum urea value (BUN = Serum urea × 0.466 mg/dl. We selected age, sex and socioeconomic status matched control patients (n = 58) and their serum sodium, fasting blood sugar, urea and creatinine were analysed to rule out any laboratory error. These control cases were selected from among other indoor patients who were admitted with diseases other than carcinoma of the lung. The exclusion criteria of the controls were identical to those of the cases in our study. All the data were analysed and the statistical analysis was done by using the SPSS, v19 software.
Results
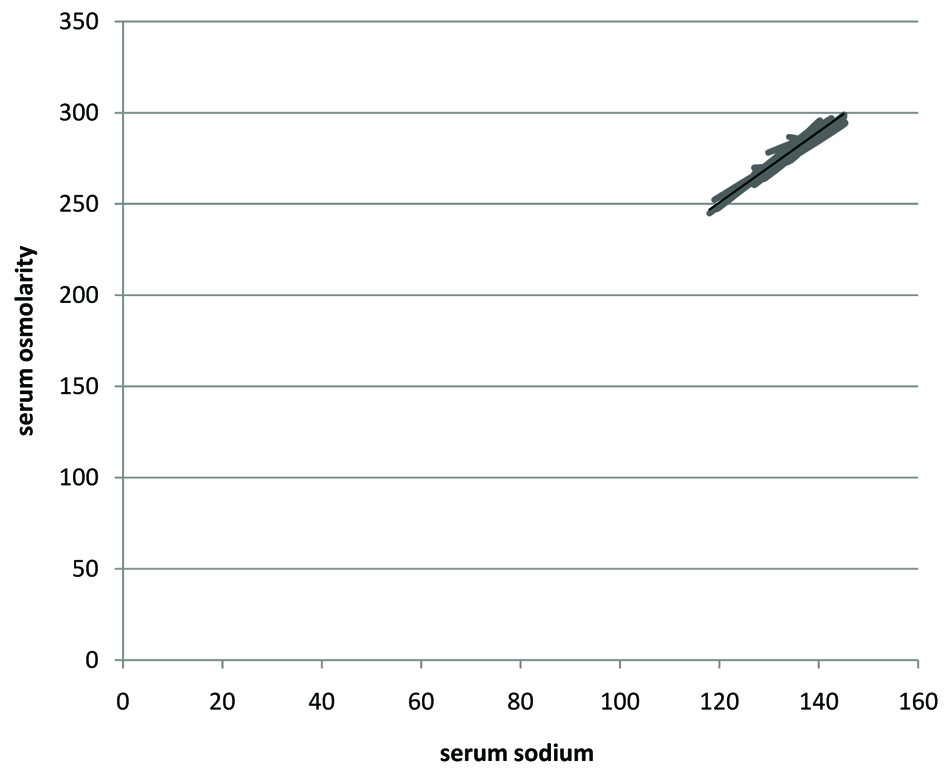
The study subjects comprised of 83 males (71.6%) and 33 females (28.4%). The median age of the study population was 58 years, which ranged from 18–85 years and 80 (68.96%) patients were smokers. The most common presenting symptom was cough (85%), followed by dyspnoea (70%), chest pain (60%), haemoptysis (51%) and fever (14%) and other symptoms like nausea, anorexia, weakness, lassitude, fatigue, constipation, less mobility and bone pain (12%). In our study, there were 99 cases (85.34%) of NSCLC and 17 cases of SCLC (14.66%) [Table/Fig-1]. The most common histology was squamous cell carcinoma (41.37%), followed by adenocarcinoma (36.20%) and SCLC (14.66%). Large cell carcinoma of lung was an uncommon histological type (0.86%) in our study population [Table/Fig-2]. The maximum of patients (44/116) were in the performance status of ECOG 2 (37.93%) and the minimum number of patients (15/116) were in the performance status of ECOG1 (12.93%). No patients with the ECOG 0 performance status were found [Table/Fig-2]. 79.8% of the NSCLC patients (79/99) presented in the stages IIIB and IV i.e. in advanced stage of lung carcinoma. All the cases (17/17) of the SCLC variety were in the extensive stages (ED). The ECOG score was significantly poor in the advanced clinical stages. (ECOG ≤2 Vs ECOG ≥ 3 in NSCLC cases, χ2 =11.25, p=.0008). Hyponatraemia was noted in 44.8% (52/116) of the lung cancer patients and the rest showed normal serum sodium (64/116) on the initial routine serum sodium estimation. The hyponatraemia (25/52,48.1%) was mild among most of the patients. Hypernatraemia was not detected in any of the subjects. The mean serum sodium level at presentation of all the cases was 134.74 meq/l (SD = ±6.15). The minimum serum sodium was 118 meq/l and the maximum value was 145meq/l. 45.5% of the NSCLC patients (45/99) suffered from hyponatraemia in comparison to 41.2% SCLC patients (7/17) who had hyponatraemia [Table/Fig-2]. A majority of the hyponatraemic NSCLC patients were of the adenocarcinoma (48.88%, 22/45) variety, followed by those with squamous cell carcinoma (20/45,44.44%). A normal serum osmolarity was seen in 64 patients and hypo-osmolarity was seen in 52 patients (44.8%) and this correlated well with the initial serum sodium levels [Table/Fig-3]. We selected a total of 58 age and sex matched control subjects who consisted of 31 males and 27 females. The mean age of all the patients was 49.68 years. The mean ages of males and females were 51.09 years and 48.07 years respectively. The mean serum sodium of the control subjects was 138.79 meq /l (SD ± 4.41) [Table/Fig-4]. In the control group, hyponatraemia was present in 5 patients (8.62%) among a total of 58 control subjects and the rest of the 53 patients (91.38%) had normal serum sodium levels. No one among the control group had hypernatraemia. In our study, the distribution of the serum sodium levels in both the cases and the control group was highly statistically significant (p<0.0005, χ2=23.01,df =1, RR=0.60, odds ratio=0.12). There was also a statistically significant difference in the mean serum sodium levels at presentation between the cases and the control group (p<0.05 and standard error of mean =0.83). On comparison of the ECOG score with the initial serum sodium level on admission, we did not find any patients with the ECOG score, zero. Among the total number of lung cancer patients within the ECOG score ≤ 2 group, we detected that 20.7% of the patients (24/116) had hyponatremia and that 30.2% of the patients had normal sodium (35/116). In the ECOG > 2 group (3 and 4 score) i.e. less ambulatory group, 24.1% patients (28/116) and 25% patients (29/116) had hyponatraemia and normal serum sodium levels respectively. When we clubbed the ECOG scores of all the patients between the two groups i.e. ECOG ≤ 2 vs. ECOG >2, the difference in the distribution of the serum sodium levels between these two groups of patients was found to be not statistically significant (9p=0.361, χ2=0.84). The ECOG performance status score at admission showed a negative correlation with the serum sodium status, which was measured on admission among all the patients (Pearson’s correlation coefficient = –0.186) . The clinical stage of the lung cancer also showed a positive correlation with the ECOG score on admission in our study. (Pearson’s correlation coefficient = 0.295).
Distribution of the study population according to ECOG score at presentation with respect to gender, the histology and clinical stage of carcinoma of lung
| ECOG score at presentation | M | F | Total | NSCLC | SCLC | Clinical stage of NSCLC | Clinical STAGE of SCLC |
|---|
| Up to IIIA | IIIB & IV | LD | ED |
|---|
| ECOG-1 | 12 | 03 | 15 | 14 | 01 | 05 | 09 | 0 | 01 |
| ECOG-2 | 27 | 17 | 44 | 37 | 07 | 12 | 25 | 0 | 07 |
| ECOG≤2 | 39 | 20 | 59 | 51 | 8 | 17 | 34 | | 08 |
| ECOG-3 | 29 | 05 | 34 | 31 | 03 | 02 | 29 | 0 | 03 |
| ECOG-4 | 15 | 08 | 23 | 17 | 06 | 01 | 16 | 0 | 06 |
| ECOG≥3 | 44 | 13 | 57 | 48 | 09 | 03 | 45 | 0 | 09 |
| TOTAL (N=116) | 83 | 33 | 116 | 99 (85.34%) | 17 (14.66%) | 20 (20.2%) | 79 (79.8%) | 00 | 17 (100%) |
Status of serum sodium as per histology in the study population at presentation
| Histological type | Serum Sodium Grade (meq/l) | Total no of cases |
|---|
| Mild hyponatremia (131-134 meq/l 132-135 | Moderate hyponatremia (126-130 meq/l ) | Severe hyponatremia (≤125 meq/l ) | Total hyponatremia | Normal sodium (135-145 meq/l ) | Hypernatremia ≥146 meqll |
|---|
| Squamous cell carcinoma | 11 | 04 | 05 | 20 | 28 | 0 | 48 |
| Adeno carcinoma | 11 | 09 | 02 | 22 | 20 | 0 | 42 |
| large cell carcinoma | 0 | 0 | 0 | 0 | 01 | 0 | 01 |
| Others | 01 | 01 | 01 | 03 | 05 | 0 | 08 |
| NSCLC (total) | 23 | 14 | 08 | 45 | 54 | 0 | 99 |
| SCLC (total) | 02 | 04 | 01 | 07 | 10 | 0 | 17 |
| Total cases | 25 | 18 | 09 | 52 | 64 | 0 | 116 |
| % of total cases [N=116] | (21.5%) | (15.5%) | (7.8%) | (44.8%) | (55.2%) | (00%) | |
Correlation between serum sodium and osmolarity
ECOG score vs. Serum Sodium grade wise population distribution
| ECOG SCORE | No of patients as per Serum Sodium Grade at admission |
|---|
| Mild Hyponatrema (131–134 meq/l ) | Moderate Hyponatrema (126–130 meq/l) | Severe Hyponatremia (≤125 meq/l ) | Total Hyponatremia (<135 meq/l) (% of total patients) | Normal Sodium (% of total patients) | Total (% of total patients) |
|---|
| ECOG 0 | 0 | 0 | 0 | 0 (0%) | 0 (0%) | 0 (0%) |
| ECOG 1 | 4 | 2 | 0 | 6 (5.17%) | 9 (7.75%) | 15 (12.93%) |
| ECOG 2 | 8 | 7 | 3 | 18 (15.52%) | 26 (22.41%) | 44 (37.93%) |
| ECOG 3 | 7 | 3 | 3 | 13 (11.20%) | 21 (18.10%) | 34 (29.31%) |
| ECOG 4 | 6 | 6 | 3 | 15 (12.93%) | 8 (6.9%) | 23 (19.83%) |
| Total (N=116) | 25 | 18 | 9 | 52 (44.8%) | 64 (55.2%) | 116 (100%) |
We attempted to correct the hyponatraemia and we found that the serum Sodium of 48 out of 52 hyponatremic lung cancer patients got corrected through a fluid restriction of 500–1000ml, nearly within two days after their admissions. The serum sodium was monitored twice daily to check for its correction among all the hyponatraemic patients. The intravenous administration of 3% hypertonic saline was required for the correction of the rest of the 4 severe hyponatraemic patients and it became normal also within two days. No change in the ECOG score was found even after the correction of the hyponatraemia. The analysis of our study population was performed in a dichotomised fashion and the results have been shown in [Table/Fig-5].
Multiple variables with respect to Serum Sodium
| Variables | Hyponatremia | Normal Sodium | p- value |
|---|
| Male | 37 | 46 | p=0.92 |
| Female | 15 | 18 |
| ECOG 0-2 OR [ECOG≤2] | 24 | 35 | p=0.361 |
| ECOG 3-4 OR [ECOG>2] | 28 | 29 |
| NSCLC | 45 | 54 | p=0.74 |
| SCLC | 7 | 10 |
| Staging: NSCLC |
| Stage≤3A | 7 | 13 | p=0.293 |
| Stage≥3B | 38 | 41 |
| Staging: SCLC |
| Limited disease | 0 | 0 | Not possible |
| Extensive diseases | 7 | 10 |
Discussion
The water and sodium homeostasis is commonly disrupted in the patients with lung cancer. Only few studies are available regarding the role of the hormones other than Arginine Vasopressin (AVP) in the sodium and water homeostasis in the patients with lung cancer [15]. Johnson et al., in their prospective study, showed that a third of the patients with small cell lung cancer and hyponatraemia had no evidence of an ectopic production of AVP in either their tumour or tumour cell line [16]. The ectopic production of the Atrial Natriuretic Peptide (ANP) may play a role in the aetiology of the hyponatraemia which is associated with lung cancer, either alone or in concert with the ectopic production of AVP [15]. Gross et al., found that eleven of the 21 patients of SCLC (52%) had hyponatraemia at presentation [16]. Johnson et al., in their prospective study, revealed that eleven of the 50 (22%) patients with lung cancer had hyponatraemia [15]. Vurgese et al., studied a group of lung cancer patients who presented with the signs and symptoms and a laboratory evidence of the Paraneoplastic Syndrome (PNS). Among them, 5.8% patients had hyponatraemia of the SIADH type [17]. Gill et al., reviewed that about 14% of hyponatraemia in the medical inpatients was caused by underlying tumour-related conditions [18]. In a recent study which was conducted by Petereit et al., 4.7% patients with lung cancer were found to have hyponatraemia at presentation [4]. Harmes et al., in a study which was done on 395 newly diagnosed cases of SCLC, revealed that hyponatraemia was present in 18.9% of all the cases of lung cancer [5]. Bose et al., in a study which was conducted in Kolkata, commented that the NSCLC patients were at a high risk of having hyponatraemia at presentation in India and that this was significantly associated with a worse outcome [19]. It was noteworthy that most of the studies were conducted in western countries and mostly on SCLC cases. Indian studies which were done on the electrolytes in both SCLC and NSCLC are limited. Our observation on the incidence of hyponatraemia in lung cancer cases was close to few [16] but it did not match with those of many studies which had been done earlier, particularly in the western countries. The results of our study were identical to those of a study which was done by Bose et al., of Kolkata, which emphasised that the NSCLC cases were also at an increased risk of developing hyponatraemia at their presentations. The ECOG performance status score at admission did show a negative correlation with the serum sodium status which was measured on admission among all the patients. This correlation would not always signify the causation. A high ECOG score meant a poor performance status, which was often correlated with an advanced stage of lung cancer in many studies [20]. The clinical stage of the lung cancer also showed a positive correlation with the ECOG score at admission in our study. [Pearson’s correlation coefficient = 0.295] So, our observation of the presence of an initial hyponatraemia with a higher ECOG score could be attributed to the clinical stage of the disease. This observation became apparent in our study only and it might not be true for all the subsets of the patients with carcinoma of the lung. More and more studies are required to establish this correlation, especially at multiple centres and in different subsets of populations in randomised prospective studies. According to Adedayo et al., the diagnosis of hyponatraemia with a tumour may not correlate with the stage, the anatomical spread or the response to the therapy [21]. PA Tai et al concluded from their study, that the SCLC cases with SIADH at presentation had a poor performance status as compared to those without SIADH (28.6% versus 7.8%, p=0.03) [22]. It was also to noted here, that that the initial ECOG scoring of hyponatraemic patients had not changed even after the correction of their hyponatraemic statuses during their close watchup at the wards, with a serial monitoring of the serum sodium. Peterit et al., showed in their study, that the median survival in lung cancer with hyponatraemia was less than that in normonatraemic patients. The serum correction of serum sodium above the level of 138 meq/l was correlated with an improved survival in their study [4]. Capewe et al., and Blagde et al., in their studies, commented that the performance score was highly correlated with the stage (and age) and in this study, it represented the “best prognostic factor” in the clinical practice [23,24].
It was not clear in different studies whether the survival benefit was associated with a change in the ECOG score. In our study, we could not detect or establish the relative % of SIADH in our patients as a contributor to hyponatraemia [3]. We calculated that 45% of patients had hypo–osmolarity, as was calculated from the serum sodium, glucose and the BUN levels of each lung cancer patient at admission. It was closely correlated with the serum sodium in our patients. (p<0.0001) Serum hypo-osmolarity is a characteristic feature of SIADH (euvolemic hyponatremia). The estimations of the urine osmolarity and the urine sodium content estimate and the measures of serum AVP and ANP for establishing SIADH as an aetiology of hyponatraemia, were not possible in our study due to economic constraints.
It was certain from our study, that hyponatraemia was not an uncommon condition and that it should be suspected and screened in the patients who are diagnosed and are being treated for malignancies. The elucidation of the aetiology of hyponatraemia on a case–by-case basis and the appreciation of the presence and the severity of it are often required, to institute the proper intervention(s) to reduce the morbidity. The other possible explanations of the high percentage of hyponatraemics could be the summer season of the study period, the bias referral from distal health centres, the moderate pain of the cancer patients which possibly induces SIADH and the possible metastasis to the adrenal gland handling sodium and water balance. A pituitary metastasis which caused hyponatraemia was reported in a case [25]. The composition of the study population and age i.e. the rural or urban status, the nutritional status and the cultural factors, together with many co-morbid illnesses in a lung cancer patient, may cause hyponatraemia.
It is note worthy that most of the studies which have been done on the incidence of hyponatraemia in lung cancer patients were conducted in western countries and mostly on SCLC cases. Indian studies which were done on the electrolytic disorders in both SCLC and NSCLC are limited. In addition, to the best of our knowledge, we found only limited Indian studies where the ECOG score was evaluated or compared or correlated with the serum sodium status in lung cancer patients on presentation. So, our study was undertaken to estimate the incidence of hyponatraemia among the patients of carcinoma of the lung and their effect on their ECOG performance statuses.