Objectives: To investigate the relationship of Body Mass Index (BMI) percentile cut off with Homeostasis Model Assessment-Insulin Resistance (HOMA-IR), a surrogate marker for insulin resistance in obese, overweight and non–obese adolescents.
Study Design: A cross-sectional analysis of 120 adolescents (divided into sixty overweight/obese and an equal number of non–obese) was performed on nondiabetic, nonpregnant (11 to 18 year old school going) adolescents in south Indian (Puducherry) population. The main outcome measure of insulin resistance was calculated as HOMA-IR (greater than 3.16). Obesity was defined as per the BMI criteria, BMI greater than or equal to 95th percentile,overweight greater than or equal to 85th percentile and non–obese less than 84.9th percentile. All adolescents were subjected to analysis of anthropometric parameters that included weight, height and BMI (body mass index). Biochemical parameters, namely venous plasma glucose (fasting) and venous plasma insulin (fasting) were included for insulin resistance calculation by HOMA-IR.
Results: Having a BMI of greater than or equal to 85th percentilewas associated with high HOMA-IR levels. As the BMI percentile increased, HOMA-IR levels also increased. Prevalence of insulin resistance for a BMI percentile of less than 84.9 was nil. Prevalence of insulin resistance for a BMI percentile of 85-94.9 was 26%.Prevalence of insulin resistance for BMI of greater than or equal to 95th percentile was 64%.
Conclusion: Insulin resistance is highly prevalent in obese and overweight adolescents as compared to that in non–obese adolescents. The onset of Impaired Fasting Glucose (IFG) is associated with the development of severe hyper–insulinaemia in obese adolescents and early primordial and primary prevention can thus alleviate the burden of future cardiometabolic disorders.
Introduction
It is a matter of great concern that adult obesity has a strong genetic predisposition [1]. However, this predisposition to obesity starts early during the first or second decade of life. It is of utmost importance to focus on the childhood and adolescent populations, to get an insight into various factors which are related to obesity and its prevalence in the south Indian population [1].
It is quite difficult to define obesity in adolescents, where there is greater fluctuation in anthropometric parameters in prepubertal to pubertal stages of adolescence [2]. There is no firm criteria among researchers on the adiposity index and on the optimal cut-off, to define the arguments which are related to over weight and obesity [3,4]. The method which is commonly used to assess body fat measurement is Body Mass Index (BMI). The measure of BMI is assessed in the clinical setting, because it can be assessed easily in field based surveys and as it is economical [5]. BMI is commonly used to define obesity: adolescents with a BMI of higher than the 85th percentile for age and gender are regarded as overweight [6]. Measurements of waist circumference and Waist-Hip Ratio (WHR) as markers of central obesity were obtained and they suggested an additional measure to BMI [7]. It is possible to define adolescents as obese by calculating the ratio between weight (kg) and height squared (in metres). This ratio is an index, which is called as the Body Mass Index (BMI), which is strictly associated with the level of general adiposity in adolescents, which is reproducible and valid. Assessment of percentiles of BMI provides valid information about the changes in obesity and general adiposity. The cut-off limits of BMI for defining over weight or obesity are still debatable. However, in agreement with Cole et al., the choice of BMI cut–off percentiles which pass through the adult BMI cut–off of 30, is reasonable [8].
Obese adolescents are fighting a quiet battle against the essential hormone, insulin. This conflict which is termed as insulin resistance is a hallmark of prediabetes and type 2 diabetes mellitus. The reason why a person fails to respond appropriately, continues to bother the scientific community. However, there are ways to make the body more receptive to insulin, which can thus help in preventing/ameliorating diabetes. For this, we planned this study with the aim of depicting different BMI cut offs as objective anthropometric measurements which were associated with insulin resistance.
Objectives
To investigate the relationship of Body Mass Index (BMI) percentile cut off with Homeostasis Model Assessment-Insulin Resistance (HOMA-IR), a surrogate marker for insulin resistance in obese, overweight and non–obese adolescents.
Subject and Methods
A cross-sectional analysis of 120 adolescents (divided into sixty overweight/obese and sixty non–obese) was performed on nondiabetic, nonpregnant (11 to 18 year) school going adolescents in south Indian (Puducherry) population. The main outcome measure of insulin resistance was calculated as HOMA-IR (greater than 3.16). Obesity was defined as per BMI criteria, BMI greater than or equal to 95th percentile,over weight greater than or equal to 85th percentile and non–obese lesser than 84.9th percentile. All adolescents underwent analysis of anthropometric parameters, namely, weight, height and BMI (body mass index). Biochemical parameters, namely, fasting plasma glucose,fasting plasma insulin and insulin resistance were also measured by HOMA-IR.
Physiological Parameters of Obesity
Both groups were analysed for physiological parameters: weight, height, BMI, blood pressure, Waist Circumference (WC), Hip Circumference (HC) and waist-hip ratio(WHR) to assess general and central obesity.
General Obesity: Height was measured to the nearest 0.1 cm, while the subject was standing in an erect position, barefoot on a flat floor, against a vertical scale and with heels touching the wall and head straight. The body weight was measured by using a weighing scale, while the subject was standing motion less, minimally clothed and without shoes on a weighing scale and it was recorded nearest to 0.1 kg. Body Mass Index (BMI) was calculated by using the formula BMI=weight (kg)/height (m2). The cut off value for obesity was more than 95th percentile in adolescents and over weight was greater than or equal to 85th percentile.
Central Obesity: Waist-Hip Ratio (WHR) was calculated to assess central obesity. Waist circumference (in cm) was measured at a point which was mid–way between the lower rib and iliac crest, with the measuring tape centrally positioned at the level of umbilicus. Waist circumference is the average of two measurements, one which is taken after inspiration and another which is taken following expiration in standing position. Hip circumference was measured (in cm) at trochanter major of the head of femur. WHR was calculated by using the following formula to assess central obesity. WHR=Waist (cm)/Hip(cm).
Biochemical Analysis of Cardio-Metabolic Risk Factors
Three ml of venous blood sample (fasting) was collected under aseptic precautions from adolescents, following ten hours of overnight fasting. Biochemical parameters were analysed as follows: fasting plasma glucose (analysed by glucose oxidase and peroxidase method GOD-POD), plasma insulin fasting (analysed by automated electrochemiluminescence), serum total Cholesterol (by the CHOD-PAP method), high density lipoprotein (by Polyanion precipitation), low density lipoprotein (by a Direct homogenous method) and serum triacylglycerols (by the Glycerol kinase method). All the above mentioned biochemical parameters were estimated by using IFCC approved procedures. The internal quality control was evaluated, based on QC samples which were provided by M/s Biorad USA. The external quality assessment was based on the QC samples which were provided by Clinical Biochemistry Lab, CMC Vellore.
Homeostasis Model Assessment of Insulin Resistance (HOMA-IR)
Insulin resistance was calculated by HOMAIR (homeostasis model assessment of insulin resistance) by using the following formula.
Insulin concentration was reported in μU/ml and glucose was reported in mmol/L.
Statistical Analysis
The statistically significant mean difference in the obese adolescents and the non obese healthy adolescents was calculated by using the unpaired student’s t test. All statistical analyzes were performed by using SPSS,16.0. Linear regression analysis was done between insulin resistance and all cardio-metabolic risk factors and anthropometric measurements such as BMI and waist circumference. Correlation analysis of insulin resistance with fasting glucose and insulin levels was doneby two-tailed Pearson’s correlation. A significant level of 95% was chosen for all tests. The level of significance was taken as (p<0.05).
Results
Having a BMI of greater than or equal to 85th percentile is associated with high HOMA-IR levels. As the BMI percentile increases, HOMA-IR levels also increase. Prevalence of insulin resistance for a BMI percentile of less than 84.9 was nil. Prevalence of insulin resistance for a BMI percentile of 85-94.9 was 26%.
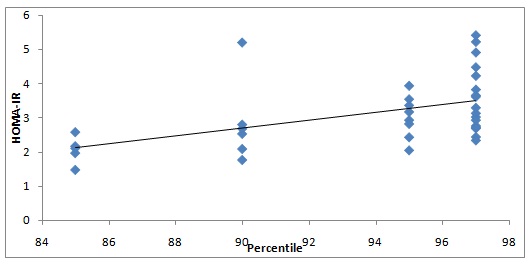
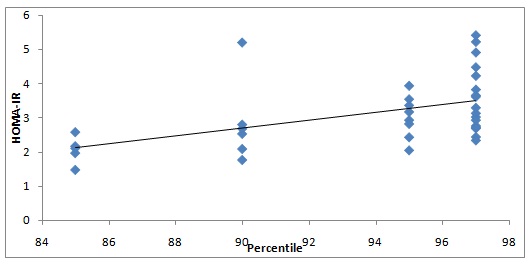
Prevalence of insulin resistance for a BMI of greater than or equal to 95th percentile was 64% [Table/Fig-1]. The results of plasma glucose (fasting) and plasma insulin (fasting) against HOMA-IR have been depicted in [Table/Fig-2] and [Table/Fig-3].
Correlation analysis of HOMA-IR with BMI percentile
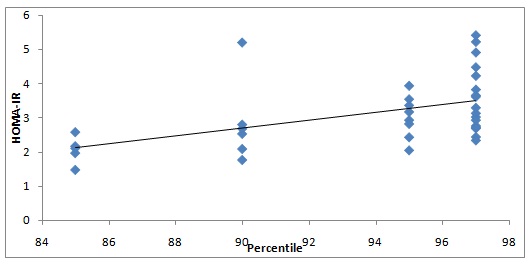
Correlation analysis of HOMA-IR with fasting plasma glucose
Correlation analysis of HOMA-IR with fasting insulin level
Details pertaining to linear regression analysis were tabulated [Table/Fig-4]. A P value of < 0.05 was considered as statistically significant. Analysis was performed by using SPSS-16 package.
Linear regression analysis of anthropometric and biochemical parameters with insulin resistance (HOMA-IR)
| Standardized Coefficients Beta | t value | p value |
|---|
| Constant | | -3.299 | 0.003 |
| Body mass index (BMI) | 0.023 | 1.081 | 0.292 |
| percentile | -0.065 | -3.525 | 0.002** |
| Waist circumference (WC) | 0.009 | 0.503 | 0.620 |
| Waist hip ratio(WHR) | -0.010 | -0.709 | 0.486 |
| Glucose | 0.277 | 22.814 | 0.000** |
| Insulin | 0.903 | 44.475 | 0.000** |
| Cholesterol | -0.335 | -1.971 | 0.061 |
| Triacylglycerol (TAG) | -0.003 | -0.18 | 0.859 |
| High density lipoprotein (HDL) | 0.188 | 1.971 | 0.061 |
| Low density lipoprotein (LDL) | 0.333 | 1.591 | 0.126 |
| Total cholesterol: High density lipoprotein ratio (TC/HDL) | 0.567 | 1.877 | 0.074 |
| Low density to high density ratio (LDL/HDL) | -0.472 | -1.567 | 0.131 |
| Mean blood pressure | -0.010 | -0.661 | 0.515 |
**p value <0.01(Highly significant)
Discussion
BMI in obese versus non–obese adolescents BMI was significantly higher among obese and overweight in comparison to that in non–obese adolescents (p<0.01). Insulin level in obese versus non–obese adolescents: Insulin level was significantly higher in the obese and overweight than in the non–obese adolescents (p<0.01). Insulin resistance among obese versus non–obese:Insulin resistance as per HOMA- IR was significantly higher among obese and overweight in comparison to that in non–obese adolescents (p<0.01).
Linear regression of HOMA-IR: Insulin resistance as per HOMA-IR could be used as a surrogate marker which is dependent only on BMI percentile, glucose and insulin levels. It is more dependent on insulin levels as compared to glucose (fasting) levels. So, insulin resistance is correlated more with insulin levels than with the fasting blood glucose in obese adolescents. Whereas, in T2DM cases, insulin resistance may or may not change because of phase wise insulin secretion. Hence, in T2DM cases, HOMA-IR is a marker which is more dependent on glucose level. Insulin resistance increases more with increasing BMI percentile. Hence, insulin resistance is more in adolescents with BMI 85th percentile and it is even higher in 95th percentile.
Building Up Resistance against insulin
In people who have neither diabetes mellitus nor insulin resistance, eating a typical mixed meal will cause blood glucose levels to rise, triggering the pancreas to produce insulin. The hormone travels distally from the site of production and it induces fat and muscle cells to absorb excess glucose from the blood for use as energy. As the cells utilize glucose, blood glucose levels decline and reach basal levels. Insulin also signals the liver to hold on to its glucose stores for use in fasting stage. Morever, insulin also decreases hepatic output of glucose through gluconeogenesis.However, people with insulin resistance (also known as impaired insulin sensitivity)build up a tolerance to insulin, thus making the hormone less effective. As a result, more insulin is needed to persuade fat and muscle cells to take up glucose and the liver to continue to store it[9]. But, in the normal scenario, the liver builds up its glycogen stores rather than output through gluconeogenesis.
In response to the body’s insulin resistance, the pancreas deploys greater amounts of the hormone to keep cells energized and blood glucose levels under control. Patients with T2DM tend to have elevated levels of circulating insulin (hyperinsulinism). The ability of the pancreas to increase insulin production,essentially means that insulin resistance alone won’t have any symptoms at first. Over a period of time, insulin resistance tends to worsen and it leads to β cell failure or depletion. Eventually, the pancreas no longer produces enough insulin to overcome the cell’s resistance. The result is higher blood glucose levels (prediabetes) and they culminate in T2DM. Insulin plays other physiological and biochemical roles in the body,besides regulating glucose metabolism, and the health effects of insulin resistance are thought to go beyond diabetes [10]. For instance, research has shown that insulin resistance, independent of diabetes, is associated with cardiovascular diseases [11].
Monitoring adolescent obesity-The need of the hour
Scientists are beginning to perceive a better vision of how insulin resistance develops. Genetic predisposition to obesity has been identified as one that makes a person more or less likely to develop the condition. It is well documentedthat older people are more prone to developing insulin resistance. Lifestyle can play a role too. Sedentary habits, overweight, or obesity increases the risk for insulin resistance [12]. Deposition of extra fat (adiposity) may also lead to inflammation, physiological stress, or other changes in the cells, that eventually contribute to insulin resistance [13]. There may be certain hitherto undiscovered factors which are produced by fat tissue, which signal the body to become insulin resistant. We therefore advise that HOMA-IR may be included in the mandatory armamentarium of laboratory investigations in obese adolescents.
How to enhance the receptivity to insulin
While it may not be possible to overcome insulin resistance entirely, there are certain ways to make the body cells more receptive to insulin. Exercise and Lifestyle Modifications (LSMs) can dramatically reduce insulin resistance. In addition to making the body more sensitive to insulin and building muscle that can absorb blood glucose, physical activity opens up newer vistas for glucose to enter the muscle cells without insulin acting as an intermediary. Weight loss can also drastically cut down on insulin resistance [14]. Research has proven that people who undergo weight-loss surgeries (bariatric) are likely to become significantly more sensitive to insulin [15].
No pharmaceutical preparations have been specifically approved for treating insulin resistance. Metformin and thiazolidinediones (TZD) are insulin sensitizers that lower blood glucose by reducing insulin resistance [16]. Thus, these oral medications are frequently employed in the management of T2DM. In addition to oral medications,yoga, meditation,listening to music,etc.would prove to be effective [17]. Receptors for insulin are crucial to its action, which may get modulated during periods of stress and anxiety. Hence, any modulation that alleviates chronic stress and anxiety would thus help in preventing or delaying the entry of obese adolescents into the realms of the insulin resistance that culminate in T2DM [18]. The present day, school going adolescent population in India is exposed to enormous physical and mental stress which has been largely linked to watching TV for a longer time, playing videogames, sedentary lifestyles, watching cartoons on TV and eating junk/preserved/less nutritious food [19,20]. All of these predispose to an early onset of insulin resistance. Hence, an aggressive lifestyle modification, healthy eating habits and insistence of health and medical education would go a long way in delaying insulin resistance [21]. This problem assumes great relevance in view of the rapid urbanisation of the commune based, panchayat population of the Union Territory of Puducherry.
Conclusion
A higher BMI in adolescents, which is greater than 85th percentile, is associated with insulin resistance. BMI could thus be asensitive anthropometric marker of evaluation in adolescent obesity as well as insulin resistance in school based and field surveys. So, in those obese adolescents with a BMI of greater than or equal to 85th percentile, the clinical approach for achieving acardiovascular prevention is modifying and preventing all the cardio-metabolic risk factors. For metabolic syndrome and in obese adolescents, the desirable approach would be to advocate a lifestyle intervention, especially weight reduction and increasing the physical activity. Insulin resistance as per HOMA-IR could thus be included as a mandatory biochemical parameter, as it would forewarn the susceptible adolescents about the impending Insulin Resistance (IR) and a wide gamut of complications which are associated with IR.
**p value <0.01(Highly significant)
[1]. Mathias RA, Deepa M, Deepa R, Wilson AF, Mohan V, Heritability of quantitative traits associated with type 2 diabetes mellitus in large multiplex families from South IndiaMetab. Clin. Exp 2009 Oct 58(10):1439-45. [Google Scholar]
[2]. Tobisch B, Blatniczky L, Barkai L, Correlation between insulin resistance and puberty in children with increased cardiometabolic riskOrv Hetil 2011 Jul 3 152(27):1068-74. [Google Scholar]
[3]. Ong KK, Early determinants of obesityEndocr Dev 2010 19:53-61. [Google Scholar]
[4]. Viner RM, Cole TJ, Fry T, Gupta S, Kinra S, McCarthy D, Insufficient evidence to support separate BMI definitions for obesity in children and adolescents from south Asian ethnic groups in the UKInt J Obes. (Lond) 2010 Apr 34(4):656-58. [Google Scholar]
[5]. Cole TJ, Flegal KM, Nicholls D, Jackson AA, Body mass index cut offs to define thinness in children and adolescents: international surveyBMJ 2007 Jul 28 335(7612):194 [Google Scholar]
[6]. Pergher RNQ, Melo ME de, Halpern A, Mancini MC, Is a diagnosis of metabolic syndrome applicable to children?J Pediatr (Rio J) 2010 Apr 86(2):101-08. [Google Scholar]
[7]. Katzmarzyk PT, Heymsfield SB, Bouchard C, Clinical utility of visceral adipose tissue for the identification of cardiometabolic risk in white and African American adultsAm. J. Clin. Nutr 2013 Mar 97(3):480-86. [Google Scholar]
[8]. Leung SS, Cole TJ, Tse LY, Lau JT, Body mass index reference curves for Chinese childrenAnn. Hum. Biol 1998 Apr 25(2):169-74. [Google Scholar]
[9]. Rizzo AC, Goldberg TB, Silva CC, Kurokawa CS, Nunes HR, Corrente JE, Metabolic syndrome risk factors in overweight, obese, and extremely obese brazilian adolescentsNutr J 2013 12:19 [Google Scholar]
[10]. Ho TF, Cardiovascular risks associated with obesity in children and adolescentsAnn. Acad. Med. Singap 2009 Jan 38(1):48-49. [Google Scholar]
[11]. Reilly JJ, Kelly J, Long-term impact of overweight and obesity in childhood and adolescence on morbidity and premature mortality in adulthood: systematic reviewInt J Obes (Lond) 2011 Jul 35(7):891-98. [Google Scholar]
[12]. Grøntved A, Ried-Larsen M, Ekelund U, Froberg K, Brage S, Andersen LB, Independent and Combined Association of Muscle Strength and Cardiorespiratory Fitness in Youth With Insulin Resistance and β-Cell Function in Young Adulthood: The European Youth Heart StudyDiabetes Care 2013 Apr 11 [Google Scholar]
[13]. Park SH, Heo NY, Park JH, Kim TO, Yang SY, Moon YS, Obesity, insulin resistance, and the risk of an elevated alanine aminotransferase activity in the Korean adolescent populationJ. Pediatr. Endocrinol. Metab 2012 25(9-10):945-49. [Google Scholar]
[14]. Ruiz JR, Rizzo NS, Ortega FB, Loit HM, Veidebaum T, Sjöström M, Markers of insulin resistance are associated with fatness and fitness in school-aged children: the European Youth Heart StudyDiabetologia 2007 Jul 50(7):1401-08. [Google Scholar]
[15]. Till H, Bluher S, Kiess W, Bariatric surgery for morbid obesity in childhood and adolescence: where do we stand in 2008?Obes Facts 2009 2(Suppl 1):34-36. [Google Scholar]
[16]. Kedikova S, Sirakov M, Boyadzhieva M, Metformin efficiency for the adolescent PCOS treatmentAkush Ginekol (Sofiia) 2012 51(6):6-10. [Google Scholar]
[17]. Matson KL, Fallon RM, Treatment of obesity in children and adolescentsJ Pediatr Pharmacol Ther 2012 Jan 17(1):45-57. [Google Scholar]
[18]. Levy-Marchal C, Arslanian S, Cutfield W, Sinaiko A, Druet C, Marcovecchio ML, Insulin resistance in children: consensus, perspective, and future directionsJ. Clin. Endocrinol. Metab 2010 Dec 95(12):5189-98. [Google Scholar]
[19]. Walpole B, Dettmer E, Morrongiello B, McCrindle B, Hamilton J, Motivational interviewing as an intervention to increase adolescent self-efficacy and promote weight loss: methodology and designBMC Public Health 2011 11:459 [Google Scholar]
[20]. Wate JT, Snowdon W, Millar L, Nichols M, Mavoa H, Goundar R, Adolescent dietary patterns in Fiji and their relationships with standardized body mass indexInt J Behav Nutr Phys Act 2013 Apr 9 10(1):45 [Google Scholar]
[21]. Nitzko S, Overweight and obesity in childhood and adolescencePrax Kinderpsychol Kinderpsychiatr 2010 59(10):831-51. [Google Scholar]