Pachydermoperiostosis is a rare hereditary disorder that is characterised by pachydermia (thickening of the facial skin and/or scalp), and periostosis (swelling of the periarticular tissue and a subperiosteal new bone formation). Other associated features are arthralgia, polyarthritis, clubbing, seborrhoea, hyperhidrosis, hypertrophic gastropathy, peptic ulcer and gyanecomastia. Eyelid ptosis which is caused by thickened eyelids (blepharoptosis) is a less common association. We are hereby reporting a patient with a complete form of Pachydermoperiostosis, wherein the presenting feature was bilateral ptosis.
Pachydermia, Periostosis, Blepharoptosis, Hyperhydrosis, Idiopathic hypertrophic osteoarthropathy
Introduction
Pachydermoperiostosis (Syn:Touraine Solente Gole syndrome, Primary Idiopathic Hypertrophic Osteoarthropathy) is a rare disease which is characterised by a periosteal new bone formation which involves the distal parts of the extremities, clubbing of fingers and toes, a column-like enlargement of lower limbs, swelling or pain of the large joints, excessive sweating of the palms and soles (hyperhidrosis), thickening of the skin, especially over the face and forehead, Cutis verticis gyrata (an undulating grooved and thickened scalp) and hypertrophic gastritis.The common symptoms which make the patients consult the health care provider are joint manifestations and skin changes [1]. Ptosis is a less commonly encountered association. We are reporting a case of complete Pachydermoperiostosis with ptosis as a presenting complaint.
Case Report
A 25 years old male presented with a history of puffiness and drooping of eyelids, which was there since one year. There was no diurnal variation in the severity of drooping or puffiness. He also had a history of pain in knee and ankle joints, with associated swelling, in the same period. Excessive sweating of hands and feet was also present.
He had earlier been seen at peripheral primary health centres by generalists, where he was advised investigations for myasthenia gravis and rheumatoid arthritis.
An examination revealed drooping of both eyelids with a narrowed palpebral fissure [Table/Fig-1]. The skin of both the eyelids was thickened. The levator palpebral strength was normal. There was also a thickened forehead skin with furrowing.

He had clubbing of the finger nails [Table/Fig-2]. The hands and feet were enlarged and they had a spade like appearance which was similar to that which is seen in acromegaly. The legs were widened and they had a “Column – Like” appearance [Table/Fig-3]. There was no joint effusion but a mild restriction of motion was present in both knees and ankles. Examination of cardiovascular system, respiratory system and abdomen revealed no significant abnormalities.

Spade like hands and feet

Investigations: Haemoglobin 13.3 gm/dl. The Total Leukocyte Count and Platelet count were normal. Erythrocyte Sedimentation Rate was 39 mm in the first hour. Random Blood Sugar was 85mg/dl, Urea was 1.6 mg/dl and Creatinine was 0.9 mg/dl. Serum Calcium, Phosphate, Alkaline phosphatase, and Liver Function Tests were normal. Thyroid Stimulating Hormone was normal at 2.41 U/l. Rheumatoid Factor and ANA were negative. VDRL test for Syphilis was negative. There was no albuminuria.
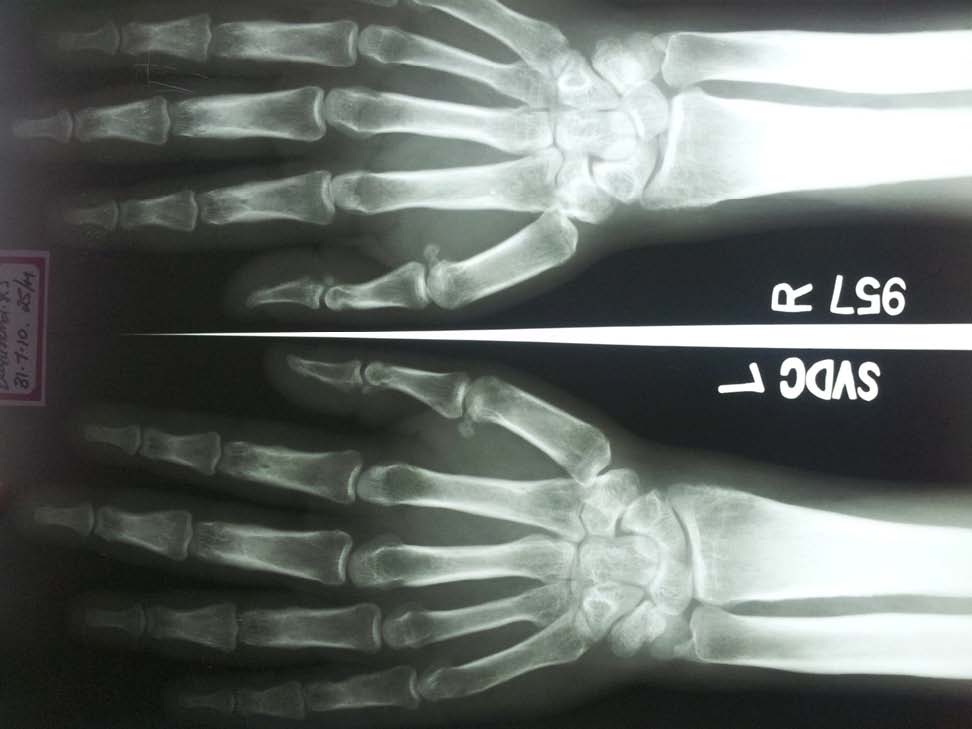
X–rays of hands and knees showed a sub – periosteal new bone formation and cortical thickening without narrowing of the medullary cavity [Table/Fig-4 and 5]
X–ray of hands showing sub – periosteal new bone formation and cortical thickening
X–ray of knees showing cortical thickening with periosteal reaction

Chest X–ray was normal. An X–ray of the skull showed a normal pitutary fossa.
The constellation of a thickened skin, a periosteal reaction in the long bones, clubbing and hyperhydrosis pointed to a clinical diagnosis of Pachydermoperiostosis (PDP). Another feature of PDP, thickened eyelids with ensuing mechanical ptosis, was a presenting complaint in this patient.
Discussion
PDP was first described by Nikolaus Friedreich in 1868, who considered it to be an example of Acromegaly. In 1935, Albert Touraine, Gabriel Solente andLaurent Gole identified it as a syndrome which was separate from acromegaly and secondary hypertrophic pulmonary osteoarthropathy [2]. Three forms of PDP have been described: Complete (Pachydermia with Periostosis and clubbing), incomplete (No pachydermia) and frusteform (Prominent Pachydermia with no Periostitis) [2,3]. The exact incidence is not known. There are ninety-six cases which have published from 1947-1960 and fifty cases have been published since 1990 [4]. Typically, men are more severely affected than women, with a ratio of 9:1 [5] and it has been reported in all the races. PDP is inherited in an autosomal dominant pattern, with a variable expression [6].
The pathogenesis of Pachydermoperiostosisis is unclear. A larger prevalence of HLA B12 was reported in one study [7]. A pathogenetic role of the vascular endothelial growth factor has been suggested, due to a good response to octreotide and the frequent finding of capillary endothelial hypertrophy in skin biopsies. Mutations in the gene which codes for 15–hydroxyprostaglandin dehydrogenase, the key enzyme which is responsible for prostaglandin degradation, which is located on chromosome 4q 33 4q34, which would lead to high concentrations of prostaglandin E2, a mediator which is involved in the processes of clubbing, skin thickening and periostosis have been described. Increased concentrations of Interleukin 6 have also been found [1].
Thickening of both eyelids, which gives rise to the mechanical ptosis which is seen in PDP, has been aptly termed as “Blepharoptosis”, to differentiate this kind of ptosis from that which results from neurologic causes.Sebaceous gland hyperplasia and dermal mucin deposition contribute to eyelid thickening and the development of ptosis [8]. In the report of Kirkpatrick et al., the patient had a difficulty in opening both eyes and he complained of findings crusts on the eye lid margins on waking up in the mornings. Tarsectomy of the tarsal plate, with shortening of the lid was performed, with excellent functional and cosmetic results. Excessive deposition of mucin in the dermis and sebatious gland hyperplasia were noted on histopathological examination [9]. Other ocular associations of PDP which are reported in the literature are corneal leucoma cataract and presenile macular dystrophy [9].
PDP is often confused with several other disorders. Acromegaly is the most common misdiagnosis which is made. However, in acromegaly, the facial skeleton, the jaw and the skull, as a whole, are enlarged. Visual defects may be detectable and there is no hormonal abnormality in pachydermoperiostosis. Pachydermoperiostosis may be identical clinically to hypertrophic pulmonary osteoarthropathy, but the distinguishing features of the former include a lack of pain and the absence of an underlying bronchial lesion (usually a carcinoma) [10]. This disorder must be differentiated from other causes of secondary hypertrophic osteoarthropathy, like suppurative pulmonary disease, congenital cyanotic heart disease and infective endocarditis. Thyroid acropachy and Syphilitic periostosis should also be considered. Diagnosis is based on recognising the characteristic phenotypical and radiological abnormalities and the exclusion of other diseases.
Although symptoms may begin to be seen at age of 7 or 8 years, this problem doesn’t strike anyone’s attention until adolescence. The most common presenting symptoms are aching along the tibial shafts and/or effusions into the knees. The symptoms slowly progress over the next 10-15 years and they later become quiescent, but the disorder can result in significant morbidity [11]. Patients may develop disabilities like severe kyphosis, restricted motion, and neurologic manifestations. Osteonecrosis of the femoral head and compressive myeloradicuopathy are other complications [12].
The characteristic radiologic features are cortical thickening and long bone periostitis, which is bilateral and symmetric. Periosteal reaction is irregular and it often involves epiphysis; there is preservation of the joint spaces and absence of erosions or periarticular osteopenias [13].
At present, there is no effective disease modifying therapy. Non Steroidal Anti – inflammatory Drugs (NSAIDS) and corticosteroids are used in symptomatic patients to alleviate the polyarthritis. Pamidronate, tamoxifen citrate octreotide, colchicine and bisphosphonates have been reported as effective therapies in refractory cases [14].
Plastic surgery is indicated for cosmetic reasons, to change the facial and scalp appearances. Bilateral blepharoplasties, tarsal wedge resections and excisions of skin furrows can be done to achieve a cosmetic improvement.
Our patient refused further investigations and a surgical referral for ptosis. He was managed conservatively with etoricoxib for the arthralgia and he had a good symptomatic relief.
Conclusion
Owing to the extreme rarity and varied presentation, the diagnosis of PCP requires a high degree of suspicion. A conservative management is sufficient in a majority of the cases. Counselling forms an important part of the therapeutic process.
[1]. Rodriguez Norberto Gomez, Ruan Jesus Ibanez, Perez Marisol Gonzalez, Primary shypertrophic osteoarthropathy (pachydermoperiostosis). Report of two familial cases and literature reviewRheumatol Clin 2009 5(6):259-63. [Google Scholar]
[2]. Touraine A, Solente G, Gole L, Un syndrome osteo-dermapathique:la pachydermie plicaturee avec pachyperiostse des extremitesPresse Med 1935 43:1820-24. [Google Scholar]
[3]. Mattuci-Cerinic M, Lotti T, Calvieri S, The clinical spectrum of pachydermoperiostosis (primary hypertrophic osteoarthropathy)Medicine 1991 70:208-14. [Google Scholar]
[4]. Jajic I, Jajic Z, Prevelence of primary hypertrophic osteoarthropathyClin Exp Rheum 1992 10(suppl.7):73 [Google Scholar]
[5]. Oikarinen A, Palatsi R, Kylmaniemi M, Pachydermoperiostosis: analysis of the connective tissue abnormality in one familyJ Am Acad Dermatol 1994 31:944-53. [Google Scholar]
[6]. Rimoin DL, Pachydermoperiostosis (Idiopathic Clubbing and Periostosis) Genetic and physiologic considerationsN Engl J Med 1965 272:923-21. [Google Scholar]
[7]. Jajic I, Jajic Z, Ozie-Bebek M, HLA antigens and primary hypertrophic osteoarthropathyClinExp Rheum 1992 10(suppl.7):74 [Google Scholar]
[8]. Offret H, Venencie PY, Fain J, Involvement of the connective tissue of the eyelids in pachydermoperiostosisJ Fr Ophthalmol 1996 19:64-68. [Google Scholar]
[9]. Kirkpatrick JNP, McKee P H, Spalton D J, Ptosis caused by pachydermoperiostosisBritish Journal of Ophthalmology 1991 75:442-46. [Google Scholar]
[10]. Vogl A, Goldfischer S, Pachydermoperiostosis: Primary or idiopathic hypertrophic osteoarthropathyAm J Med 1962 34:727-33. [Google Scholar]
[11]. Schumacher HR, Hypertrophic osteoarthropathy: rheumatologic manifestationsClin Exp Rheumatol 1992 10(suppl 7):35-40. [Google Scholar]
[12]. Jajic I, Jajic Z, The spectrum of skeletal and visceral abnormalities in 52 patients with primary hypertrophic osteoarthropathyClin Exp Rheum 1992 10(suppl7):73 [Google Scholar]
[13]. Bauer JS, Hypertrophic osteoarthropathy. in: Baert ALEncyclopedia of Diagnostic Imaging 2008 1st edBerlin New York HiedelbergSpringer:929-31. [Google Scholar]
[14]. Bhansali A, Singh R, Sriraam M, Bhadada S, Pachydermoperiostitis and bisphosphonatesJ Assoc Physicians India 2006 54:340 [Google Scholar]