Peripheral Adenomatoid Odontogenic Tumour — Is It Really Peripheral?: A Case Report
N. Lavanya1, M.R.C. Rajeshwari2, R. Bharathi3, A. Shaheen4
1 Formerly Postgraduate Student, Department of Oral and Maxillo Facial Pathology, Tamil Nadu Government dental College and Hospital, Chennai, India.
2 Formerly Assistant Professor, Department of Oral and Maxillo Facial Pathology, Tamil Nadu Government Dental College and Hospital, Chennai, India.
3 Reader, Department of Oral and Maxillo Facial Pathology, Tamil Nadu Government Dental College and Hospital, Chennai, India.
4 Formerly Head of Department, Department of Oral and Maxillo Facial Pathology, Tamil Nadu Government Dental College and Hospital, Chennai, India.
Name, Address, E-Mail Id of The Corresponding Author: Ms N Lavanya, 15/1, Canal Road, Tiruvanmiyur, Chennai – 600 041, India.
E-mail: lavanyabds@yahoo.com
A Peripheral Adenomatoid Odontogenic Tumour (PAOT) is quite a rare entity which has been infrequently reported in the literature. These uncommon clinical variants of an Adenomatoid Odontogenic Tumour (AOT), typically manifest as a soft tissue mass of the gingiva, which mimick a common epulis, but yet have an identical histopathologic presentation as their intraosseous counterpart. These lesions, though they are indolent in nature, have a tendency to cause well defined deep bony pockets. Only fourteen cases have been adequately documented so far. We are reporting a case of a PAOT of the anterior maxillary gingiva, with a periodontal bone defect in a 12 year old girl. The relevant literature has been briefly reviewed, with an insight into the probable origin of PAOTs with bony defects.
Peripheral, Adenomatoid, Gingiva, Odontogenic
Introduction
Being reported in the literature as sporadic, Peripheral adenomatoid odontogenic tumours (PAOTs) account for a meagre 2.3% of the adenomatoid odontogenic tumours (AOTs) which have been published so far [1]. These rare clinical variants of AOT typically manifest as a soft tissue mass of the gingiva, which mimick an epulis, but yet have an identical histopathologic presentation as their intraosseous counterpart [2]. These occur mainly during the mixed dentition period and a couple has also been reported in children who are less than five years of age. Though they are indolent in nature, some of the reported cases have been associated with deep bony pockets [1].
Case Report
A 12 years old girl presented to our hospital with a six month history of an asymptomatic soft tissue mass on the maxillary gingiva. Her history revealed that the growth had started as a small nodule and had attained the present size and was not associated with pain or spontaneous bleeding. Her medical history was uneventful. Intra orally, a sessile growth of size 0.8 x 1.2 x 0.5 cm was seen, that almost entirely covered the labial surface of the right maxillary central incisor [Table/Fig-1]. The growth had displaced the tooth palatally [Table/Fig-1 inset]. Palpation revealed a firm to hard mass with a slightly lobulated surface and mobility of the involved tooth. No cervical lymphadenopathy was detected. On the Intra Oral Periapical Radiograph, extensive bone loss along the distal surface of the right maxillary central incisor, with periodontal ligament space widening on the mesial surface, was appreciated [Table/Fig-2].
Intra – oral photograph showing a sessile growth almost entirely covering the labial surface of right maxillary central incisor. Inset shows palatal displacement of right maxillary central incisor

Intra – oral Periapical radiograph showing well defined bone defect loss along the distal surface and periodontal ligament space widening on the mesial surface of the right maxillary central incisor

With a provisional diagnosis of fibrous epulis, the lesion was excised in toto; the bone defect was curetted and the mobile right maxillary central incisor was splinted with the adjacent teeth.
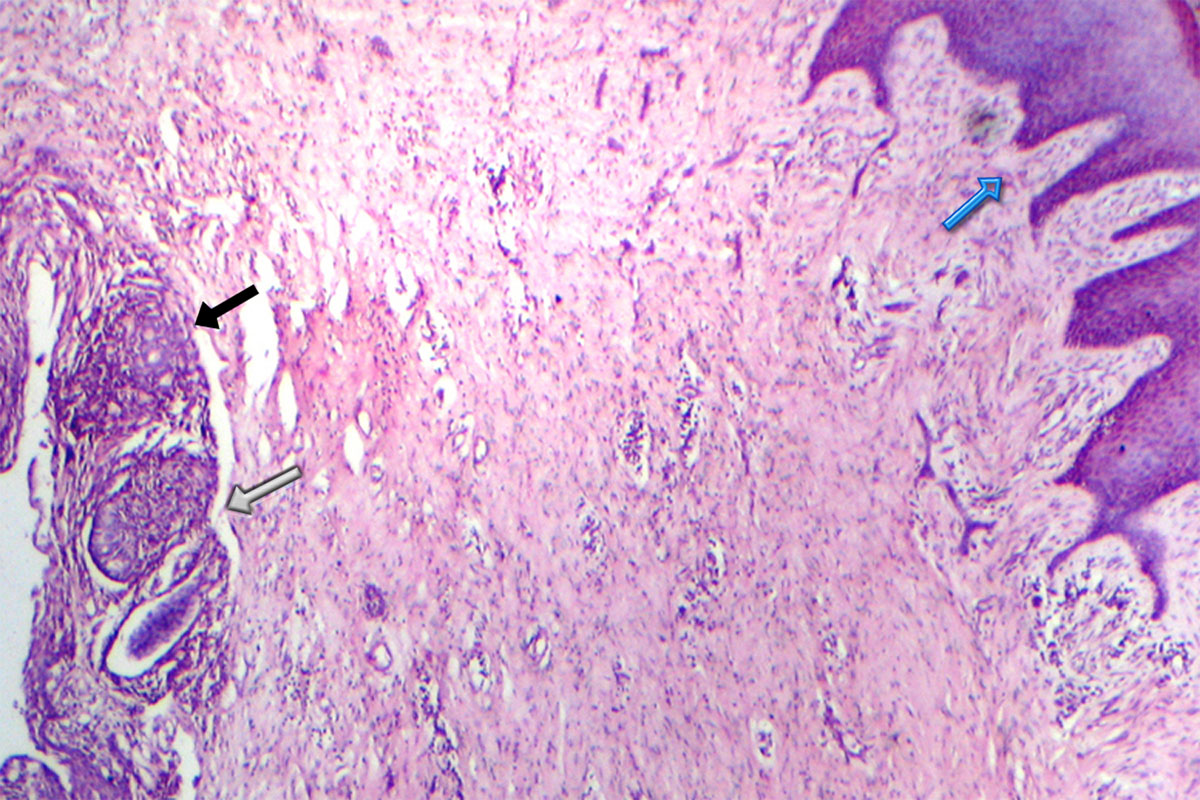
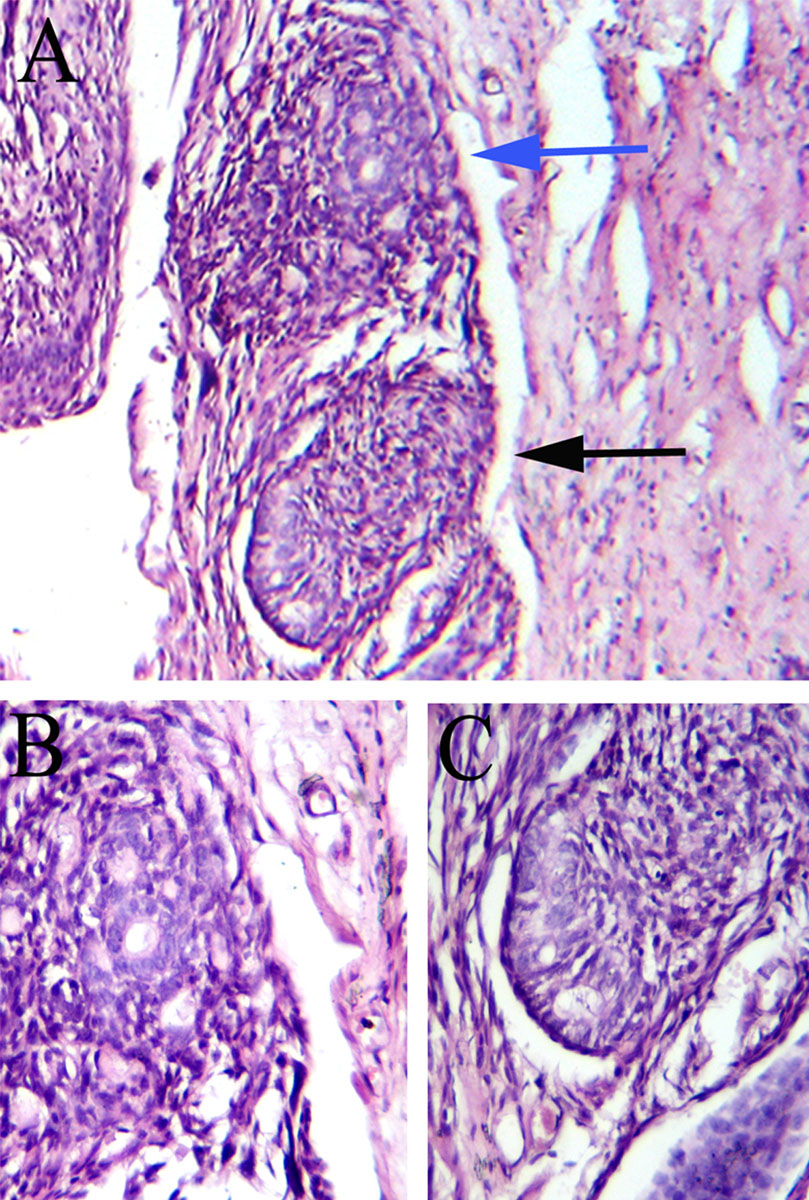
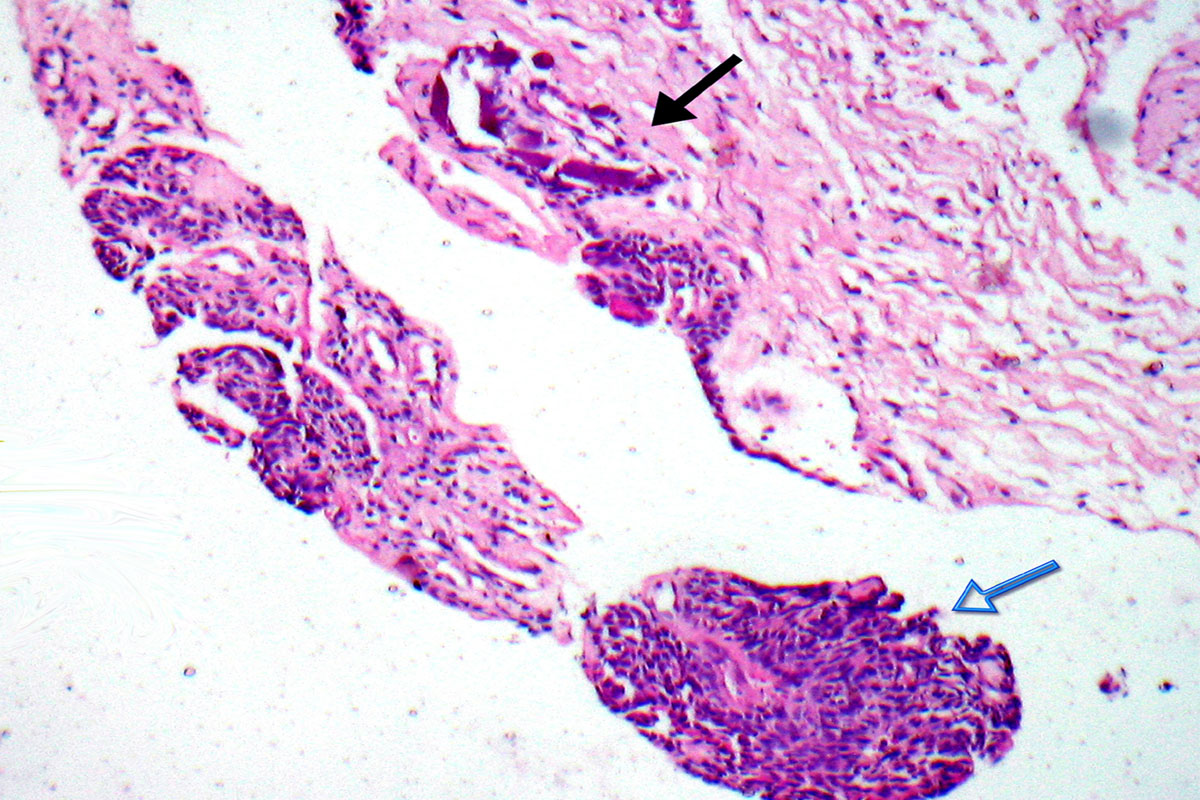
The excised lesion was examined microscopically. It was composed of a fibrous connective tissue which was covered by overlying oral epithelium [Table/Fig-3]. The deeper layers of the connective tissue showed proliferation of the darkly staining, tall, columnar, odontogenic epithelial cells which were arranged in rossetes and a few duct like structures. The ducts were variably lined by columnar or cuboidal epithelial cells [Table/Fig-4]. The deeper sections of the specimen, which were evaluated, showed varying amounts of calcified material [Table/Fig-5]. A diagnosis of a Peripheral adenomatoid odontogenic tumour was rendered.
Photomicrograph showing rosettes of odontogenic epithelial cells (grey arrow) and scattered duct like structures (black arrow). Overlying stratified squamous epithelium is also seen (blue arrow). (Original magnification x 40)
(A) Photomicrograph showing rossetes of odontogenic epithelial cells (black arrow) and duct like structures (blue arrows) (Original magnification x 100). (B) Photomicrograph showing well defined duct like structures lined by cuboidal cells. (C) Photomicrograph showing duct like structures lined by columnar odontogenic epithelial cells. (B and C – original magnification x 400)
Photomicrograph showing basophilic amorphous calcified material (black arrow) and rosettes of odontogenic epithelial cells near by (blue arrow). (Original magnification x 150)
A subsequent follow up to six weeks revealed considerable reduction in the mobility of the right maxillary central incisor. An inclined plane was planned to align the right maxillary central incisor in cross bite. Unfortunately, the patient was lost for further follow up.
Discussion
Peripheral or extra osseous odontogenic tumours are quite infrequent, rare lesions of the oral cavity. Within the classification of odontogenic tumours, they constitute a mere 3.4% [3] of the tumours. These have identical histopathologic presentations as their intra-osseous counter parts, except that they occur in the soft tissue which overlie the tooth bearing areas of the maxilla and the mandible [2].
AOTs are benign odontogenic tumours with unique clinical and histopathologic characteristics. The three known variants of AOT include the follicular variant, the extra follicular variant and the peripheral epulis like variant. The follicular and the extra follicular variants are intraosseous lesions; the former shows a pericoronal relationship with the crown of an unerupted tooth, while the latter does not [2]. The peripheral variant is an extra osseous lesion and it accounts for a meagre 2.3% of the AOT’s which have been reported in the literature [1]. They typically present as soft tissue masses of the gingiva which mimick an epulis, as most of the other peripheral odontogenic tumours do. Their demographic features are very similar to those of their intra osseous counter parts. PAOT has a surprisingly high female predilection in the ratio of 2:1 [4]. These are about seven times more common in the maxilla than in the mandible [4]. With a peak incidence at 12 years (9-17 years), these manifest most often on the labial aspect of the maxillary teeth, mostly in relation to the incisors [5]. Although there are no pathognomonic radiographic findings, it has a tendency (67% of the reported cases) to cause periodontal bone loss or a well defined deep bony pocket [1,6,4,7], which was observed in the present case.
The clinical differential diagnosis for these peripheral epulis like variants should range from the more common lesions like the fibrous epulides, pyogenic granulomas, peripheral giant cell granulomas and the peripheral ossifying fibromas to the rarer connective tissue neoplasms like fibromas, neurofibromas and peripheral odontogenic neoplasms.
The histogenesis of the peripheral variant, as for the central variant, is quite debatable. It can be categorised either as a benign tumour or as a hamartomatous lesion [5], which is derived from the odontogenic epithelium and its remnants. The lesions which occur very early in life, at around three years of age, can be regarded as hamartomatous lesions, while the others which occur at a later age are considered as benign neoplasms. There still prevails an uncertainty over the categorisation and the nomenclature of these Epulis like AOTs, which show a deep punched out moat like bony defect of the periodontal space. Whether these are follicular/extra – follicular AOTs which originated intraosseously and erupted along with the tooth in relation and finally assumed a peripheral position or lesions with a denovo peripheral origin, is a question to ponder upon [2]. The present case also falls into this category of un – identifiable origin, which was named by Philipsen et al., as hybrid variant [6]. A similar case which was recently reported by Jham et al., [7] had the features of a central lesion and a peripheral presentation can also be called as a hybrid variant of an AOT. The intraosseous origin of the epulis like variant with a radiographic periodontal manifestation becomes the most rational argument, since such small lesions are not expected to cause a appreciable bone loss. Hence, the bony defect is most likely to be a remnant of the eruptive pathway of the AOT, when it erupted along with the tooth in relation and finally assumed a peripheral location [4]. The cell rests of serrae in the superficial gingiva or in the basal cell layer of the oral epithelium, seem to be the most probable origin for those PAOTs without a periodontal bony defect [6,8].
The histopathology of the peripheral variant is analogous to that of the central variant with the characteristic rosettes of the odontogenic epithelial cells and duct like structures which are lined by columnar or cuboidal cells, with their nuclei being polarized away from the luminal surface and diffuse calcifications. These are usually unencapsulated unlike the central lesions [2,9].
The peripheral odontogenic tumours are generally indolent. This benign biologic behaviour appears to be true for the PAOTs too. So, a conservative excision with adequate margins seems to be the treatment of choice [10]. In cases like the present one, with associated bone defects and mobility of the tooth, a deep curettage, filling the defect with bone graft and splinting the compromised tooth with the adjacent teeth, will salvage the tooth. Bone grafting was not considered in this case, as during surgery, a single walled defect was evident. There is too little information on PAOTs in the literature and recurrences have not been documented.
Conclusion
The Peripheral odontogenic tumours, by themselves, are rare. Within the classification of the peripheral odontogenic tumours, the PAOTs are still rarer and uncommon. The intraosseous origin of these hybrid PAOTs with bony defects seems to be the most plausible answer. The strikingly high (7:1) predilection in the maxilla and the fact that all but one PAOT have been reported in relation to the incisor teeth as opposed to a high incidence of canine related intra-osseous AOTs being still, warrants a discussion regarding the nomenclature and the reclassification of these hybrid variants of AOTs. The future reports on PAOTs with or without bony defects will answer the question.
[1]. Philipsen HP, Reichart PA, Siar CH, Ng KH, Lau SH, An updated clinical and epidemiological profile of the adenomatoid odontogenic tumour: a collaborative studyJ Oral Pathol Med 2007 36:383-93. [Google Scholar]
[2]. Curran AE, Peripheral odontogenic tumours. In: White DK, guest editorOral Maxillofacial Surg Clin N Am 2004 16:399-408. [Google Scholar]
[3]. Ladeinde AK, Ajayi OF, Ogunlewe MO, Adeyemo WL, Arotiba GT, Odontogenic tumours: A review of 319 cases in a Nigerian teaching hospitalOral Surg Oral Med Oral Pathol Oral Radiol Endod 2005 99:191-95. [Google Scholar]
[4]. Ide F, Mishima K, Saito I, Kusama K, Rare peripheral odontogenic tumours: report of 5 cases and comprehensive review of the literatureOral Surg Oral Med Oral Pathol Oral Radiol Endod 2008 106:e22-28. [Google Scholar]
[5]. Kearns GJ, Smith R, Adenomatoid odontogenic tumour: an unusual case of gingival swelling a 3-year old patientBr Dent J 1996 181:380-82. [Google Scholar]
[6]. Philipsen HP, Samman N, Ormiston IW, Wu PC, Reichart PA, Variants of adenomatoid odontogenic tumour with a note on tumour originJ Oral Pathol Med 1992 21:348-52. [Google Scholar]
[7]. Jham BC, Passos JB, Do Carmo MAV, Gomes CO, Mesquita RA, Oral Oncology EXTRA 2006 42:268-71. [Google Scholar]
[8]. Yazdi I, Nowparast B, Extra-osseous adenomatoid odontogenic tumour with special reference to the probability of the basal-cell layer of the oral epithelium as a potential source of origin. Report of a caseOral Surg Oral Med Oral Pathol 1974 37:249-56. [Google Scholar]
[9]. Philipsen HP, Reichart PA, Zhang KH, Nikai H, Yu Qx, Adenomatoid odontogenic tumour: biologic profile based on 499 casesJ Oral Pathol Med 1991 20:149-58. [Google Scholar]
[10]. Buchner A, Sciubba JJ, Peripheral epithelial odontogenic tumours: a reviewOral Surg Oral Med Oral Pathol 1987 63:688-97. [Google Scholar]