Pathologic Tooth Migration-Spontaneous Repositioning Following a Non-Surgical Periodontal Therapy: A Case Report
Punit Vaibhav Patel1
1 Faculty of Dental Sciences, Department of Dentistry, Institute of Medical Sciences, Banaras Hindu University, Varanasi, India.
Name, Address, E-Mail Id of The Corresponding Author: Dr Punit Vaibhav Patel, Faculty of Dental Sciences, Department of Dentistry, Institute of Medical Sciences, Banaras Hindu University, Varanasi, India.
Phone: 91-7275832787,
E-mail: punitvai@gmail.com
This case report describes the spontaneous correction of a pathologic tooth migration (PTM) and reduced infra-bony pockets after a nonsurgical periodontal therapy.
Pathologic tooth migration, Periodontal therapy, Spontaneous repositioning
Case Report
A 23-year-old woman reported to the Department of Periodontics with the chief complaint of an increasing gap between her maxillary anterior teeth which was there since one year and a bleeding gingiva on brushing. There was no history of dental treatment, and the patient had no deleterious oral habits. Her medical history had no contraindications for a periodontal therapy. Intraoral examination revealed a 3 mm diastema [Table/Fig-1a and b] between the maxillary central incisors. Her generalised plaque control record was 66%. Bleeding on probing was present and average generalised probing pocket depth was approximately 5-6 mm, with a clinical attachment loss of approximately 2 – 3 mm. Supra- and subgingival calculi were detected, which were concomitant with the attachment loss. The maxillary left central incisor had pocket depths which ranged from 5 to 8 mm, with greater probing depths mesially and palatally. The tooth had migrated to facial, distal, and occlusal directions with a grade one mobility. A deep overbite and fremitus was associated with maxillary and mandibular central incisors. A radiographic evaluation showed widening of the periodontal ligament space and bone loss around upper central incisors, with no sign of a periapical infection.
Preoperative photograph showing diastema between central incisors with supra and subgingival deposits. (a) front view (b) lateral view showing anterior proclination of central incisors

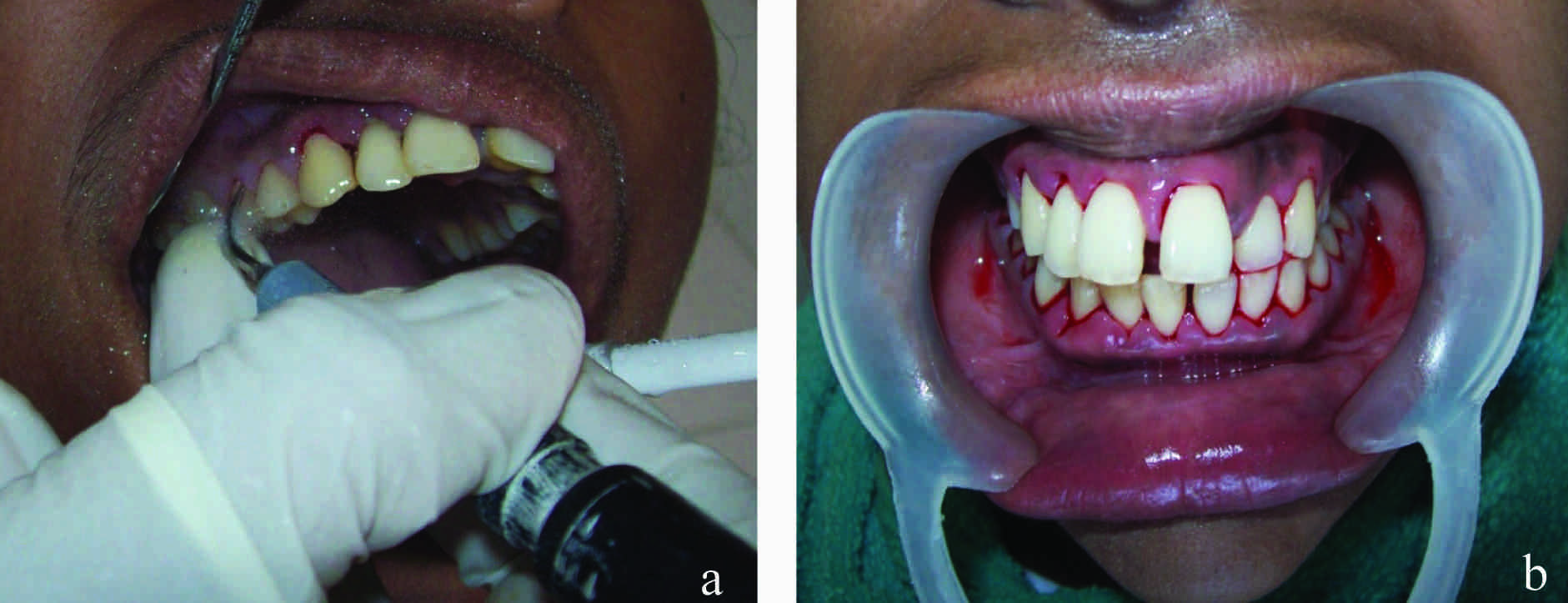
Full mouth scaling and root planning were performed [Table/Fig-2a and b], followed by meticulous plaque control instructions, which included demonstration of the proper brushing technique as well as inter-dental brushing and flossing; 0.2% chlorhexidine rinsing (10 ml per rinse) was prescribed on a 12 hour frequency for 2 weeks. After three weeks, the patient was re-evaluated for her clinical outcomes. At this time, the maxillary diastema was found to be reduced to 1 mm and signs and symptoms of periodontal disease were found to be significantly controlled [Table/Fig-3a and b]. The mobility of the migrated incisor was also reduced. Oral hygiene maintenance instructions were reinforced- The patient was placed on a 3 – month maintenance program, and after 6 months of follow-up, her periodontal condition was found to be stable.
(a) Performing ultrasonic scaling (b) Immediately after ultrasonic scaling
Postoperative photograph (3 weeks) showing reduction in diastema between central incisors with restoration of healthy gingiva. (a) Front view. (b) Lateral view-showing reduction in anterior proclination of central incisors

Discussion
Several case series have shown success in treating PTM with periodontal therapy alone. A periodontal treatment can induce spontaneous repositioning (SR) which is defined as a tooth movement that occurs without the use of orthodontic appliances, leading to a spontaneous resolution of PTM [1]. SR, because of periodontal treatment, occurs within weeks and it tends to move rapidly at the beginning of the therapy and then to slow down. SR can be accomplished through surgical and non-surgical periodontal treatments according to Gaumet et al.,[2] who evaluated SR in 33 PTM cases which exhibited diastema. In his study, partial and complete diastema closures were obtained in 49% and 36% of the teeth respectively after scaling and root planing (SRP). When the patients received surgical treatment (Open Flap for Debridement or Guided Tissue Regeneration with Demineralized Freeze Dried Bone Allograft), 52% of the teeth underwent complete diastema closures without any additional orthodontic therapy. A higher percentage of complete closures was found if the diastema was small to moderate (<1mm). Other case reports have shown that a periodontal therapy alone (non-surgical or surgical) can be successful in closing a diastema. PTM cases and the results appeared to be stable, with no relapse, at least one year following the therapy [3].
[1]. Gaumet PE, Brunsvold Ml, McMahan CA, Spontaneous repositioning of pathologically migrated teethJ Periodontol 1999 70:1177-84. [Google Scholar]
[2]. Brunsvold M, Zammit K, Dongari A, Spontaneous Correction of Patho-logic Migration Following Periodontal TherapyInt J Peridont Rest Dent 1997 17:183-89. [Google Scholar]
[3]. Sato S, Ujiie H, Ito K, Spontaneous Correction of Pathologic Tooth Migration and Reduced Infrabony Pockets Following Nonsurgical Periodontal Therapy: A Case ReportInt J Periodontics Restorative Dent 2004 24:456-61. [Google Scholar]