CEREBROSPINAL FLUID rhinorrhoea is defined as the leakage of CEREBROSPINAL FLUID through the nose due to communication between nasal cavity and Sub-arachnoid space. It occurs due to breach in 4 layers – mucosa of the nose and PNS, skull base, Duramater, Subarachnoid membrane. With the advent of nasal endoscope and advancement in technology, Endoscopic Endonasal closure of CEREBROSPINAL FLUID leak has reached tremendous heights due to exact localization and precise placement of graft. In this article, we are publishing a case report of Non-traumatic normal pressure CEREBROSPINAL FLUID leak of more than 1.5cm in size which was successfully closed Endoscopically by multilayered technique
Cerebrospinal fluid, Rhinorrhoea, Nasal endoscope, Endoscopy
Case Report
A 48 years old female presented with complaints of a watery nasal discharge from the left nose of one year’s duration. Patient had no past history of fever/trauma/nasal surgeries. Patient had been on symptomatic medical management for these symptoms, with no significant improvement. She was a known case of systemic hypertension since five years, who was on regular treatment. Local examination revealed a watery discharge from left nose, more so on bending down. Ear and Throat were within normal limits. Diagnostic Nasal Endoscopy revealed a watery discharge from left middle meatal region, which increased on Valsalva maneouver.
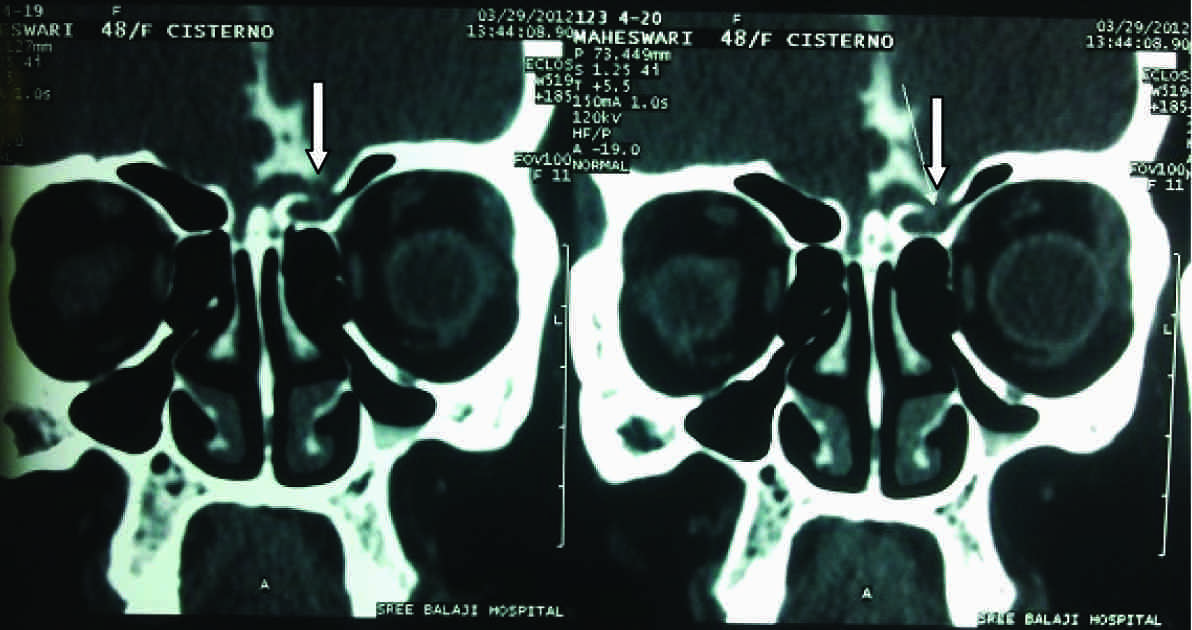
CT cisternography was done, which confirmed a bony defect in the roof of left anterior ethmoidal cells, with minimal herniation of adjacent dura and brain matter [Table/Fig-1]. Watery discharge was collected and sent for a biochemical analysis, which confirmed it to be Cerebrospinal Fluid. Beta 2 transferrin test was not done because it was not available in our hospital. Patient was started on acetozolamide 250mg twice daily and Injection Ceftriaxone 1gm Intravenously twice daily, two days before surgery.
CT Cisternography showing defect in the fronto-ethmoidal region left side
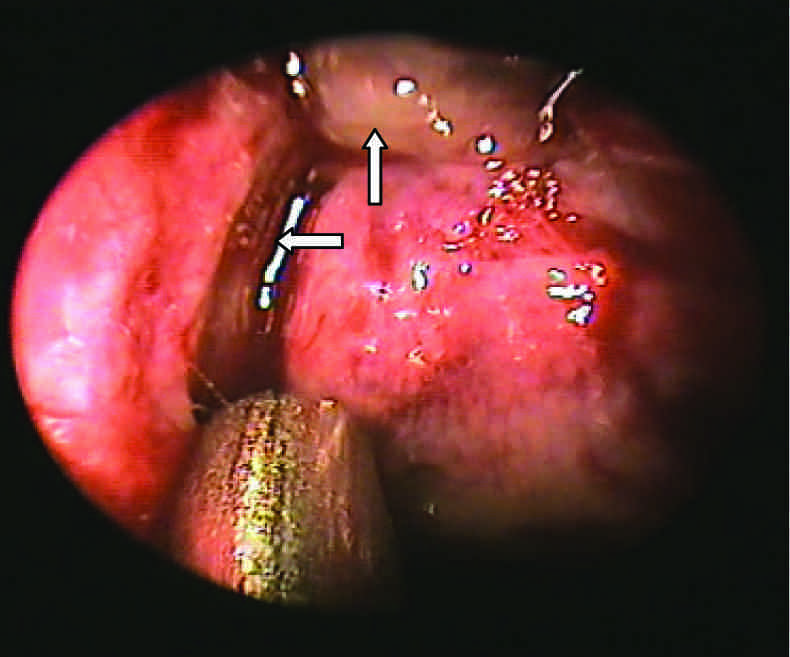
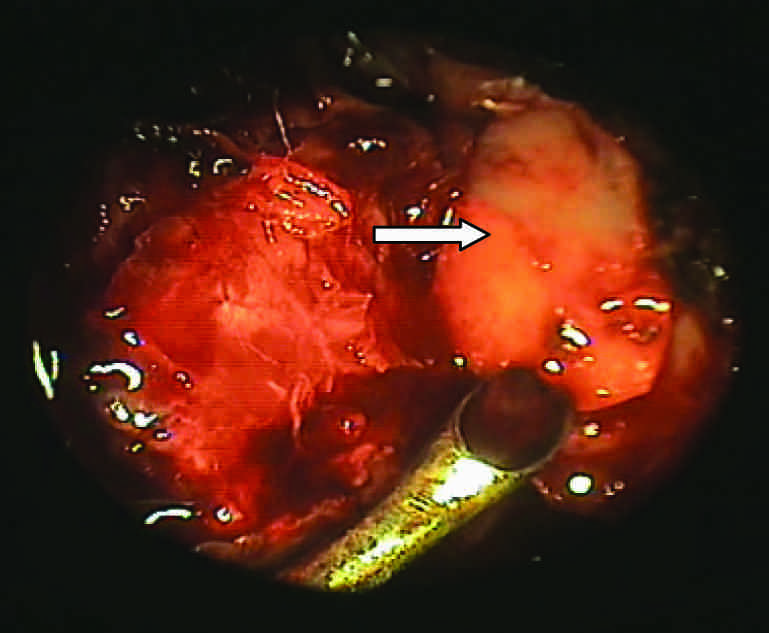
Under general anaesthesia, middle meatal antrostomy was done (left side). Frontal recess widened. Supraorbital cells were identified. A defect of approximately 1.5 cms was located in the skull base, in the region of anterior ethmoids, with minimal herniation of brain tissue [Table/Fig-2]. Middle turbinate was resected and it was preserved as a pedicled flap. Herniated brain tissue was cauterised. The site of leak was localised precisely and the margins were clearly delineated and freshened. Fascia lata was insinuated through the defect by underlay technique. Septal cartilage was snuggly fitted over the fascia lata [Table/Fig-3] and an another layer of fascia lata was placed over the cartilage. Surgicel was placed and fibrin glue (buffer solution) which was prepared from patient’s own blood was installed over it. Middle turbinate was rotated and it was transpositioned as pedicled flap. Merocele packing was done for securing complete haemostasis and to keep the graft in place for 1 week. Immediate post – operative period was uneventful. Patient was discharged on the second post operative day and she was advised to continue antibiotics and acetazolamide and to avoid straining. On the fifth post – operative day, patient developed a watery discharge (left side), headache and low grade fever.
Pre – operative picture showing the defect with herniation of brain and cerebrospinal leak
Pre – operative picture showing cartilage covering the defect
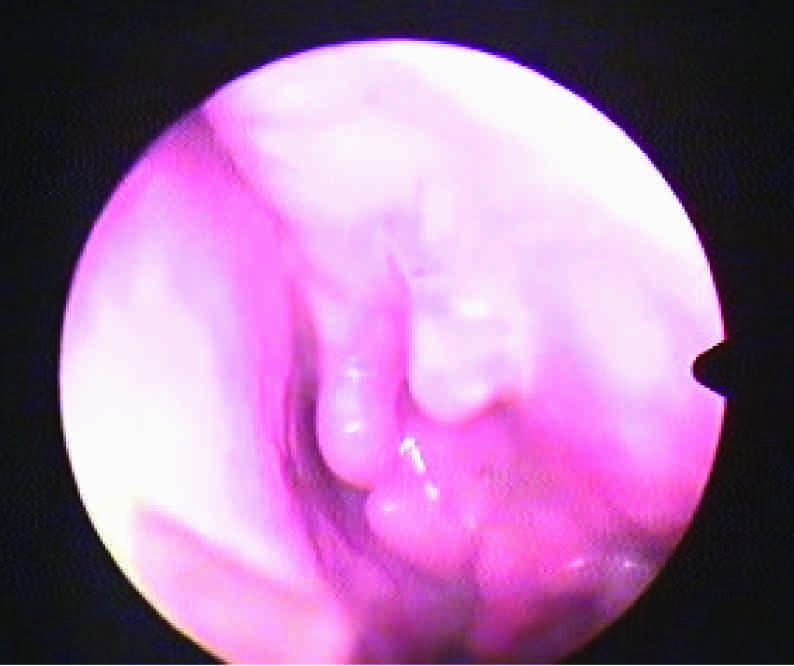
On examination, patient had signs of meningism, with temperature and no neck rigidity. Kernig’s and Brudzinski’s signs were negative. Patient was re – admitted and was treated conservatively with complete bed rest, acetazolamide, intravenous antibiotics (Vancomycin), a lumbar drain and stool softeners. Cerebrospinal fluid analysis showed no pus cells. Intermittent External Lumbar Cerebrospinal Fluid Drainage was performed at the rate of 50ml/day for three days. On the third day, there was no active leak from left side. Patient’s vitals were stable. She was continued on the same treatment for four days. Diagnostic nasal endoscopy which was done after ten days showed no evidence of any Cerebrospinal Fluid leak. Patient is on follow up for the past three months [Table/Fig-4].
Post operative picture showing no evidence of leak
Discussion
CSF rhinorrhoea can occur directly from anterior cranial fossa through the nose or indirectly from middle or posterior fossa through the Eustachian tube [1]. CSF rhinorrhoea was first described by Galen in 200 BC [1]. Saintclair Thompson reported the first series of patients with spontaneous leak in 1889 [1]. The first successful surgical approach was attributed to Dandy in 1926, by intracranial route [2]. The commonest etiology of CSF rhinorrhoea is trauma (80 – 90%) followed by Iatrogenic leaks (10 – 16%) and non-traumatic spontaneous leaks [2,3]. The incidence of CSF in closed head injury is 1-3% and is upto 15% of all base of skull fractures [3]. Most patients with CSF leak due to non-surgical trauma present immediately where as only 50% of patients with Iatrogenic CSF leak present within the 1st week [4]. 95% of all delayed CSF leaks in Non surgical trauma occurs within 3 months and are thought to occur as a result of a delayed elevation of ICP, lysis of clots in and around the site of injury, resolution of oedema, loss of vascularity, with resultant necrosis of soft tissue and bone. Non-traumatic CSF leaks are relatively uncommon. 45% of such leaks are high pressure leaks occuring due to Increased Intra cranial Tension due to tumor, hydrocephalus, etc.
Presence of headache should arouse the suspicion of Increased Intra cranial Tension [5]. Normal pressure leaks from 55% of non-traumatic CSF leaks, which is a very poorly understood entity and its origin remains unclear. In this article we are publishing one such challenging case of Normal pressure non-traumatic CSF leak of size approximately 1.5cm managed endoscopically.
The choroid plexus produces 50% – 80% of Cerebrospinal Fluid and 30% is produced by ependymal surface. Cerebrospinal Fluid production is regulated through multiple Na+/k+ ATPases. At any one time, roughly about 90 – 150ml of Cerebrospinal Fluid is in circulation and it is produced at the rate of 20 ml/hour and 500 ml/day. The commonest aetiology of a Cerebrospinal Fluid leak is trauma to the anterior skull bone, since the dura in this area is tightly adherent to the thin skull bone and can be easily torn. Initially, Iatrogenic Cerebrospinal Fluid was commonly due to Neuro Surgical procedures occurring in 12% acoustic neuroma resection [6]. Endoscopic sinus surgeries cause Cerebrospinal Fluid leaks in 0.5% cases and the most commonest site is right lateral cribriform lamella. High pressure non – traumatic leaks occur due to remodeling and thinning of skull bone, due to an increased intracranial tension, which causes ischaemia which results from compression of vessels, leading to formation of skull bone defects.
Hypothesized theory for a Normal pressure non – traumatic leak (a spontaneous leak) is a result of physiologic alterations in Cerebrospinal Fluid pressure and constant dural pulsation, leading to erosion of skull base. Congenital cases of Cerebrospinal Fluid leaks are considered as different entities, as they may have/not have increased Intracranial tension. The commonest causes are failure of closure of anterior neuropore, a persistent craniopharygeal canal [7] and empty sella syndrome [8]. Our case was an interesting case of a normal pressure, non-traumatic, Cerebrospinal Fluid leak with more than one year’s duration. In most of the cases, a Cerebrospinal Fluid leak is a clinical diagnosis with a good history and physical examination. A ring or halo sign can further help in physical examination, where Cerebrospinal Fluid is mixed with blood. When it is placed on a piece of filter paper, blood will separate out [central blood with a clear ring of Cerebrospinal Fluid [9]. Biochemical analysis of fluid for glucose (more than 30mg/dl) can help in diagnosis. Test for beta 2 transferrin is considered as gold standard for conforming Cerebrospinal Fluid. In our case, it was not done, as it was not available in our hospital. Beta-trace protein can be used for diagnosis, but it is also found in heart and serum, and its levels are altered in renal insufficiency, multiple sclerosis and Cerebral Infarcts [10]. Imaging techniques like CT cisternography which use an Intrathecal contrast dye [iophendylate] are more accurate in diagnosing Cerebrospinal Fluid leaks. Some authors recommend use of intranasal topic fluorescein during Diagnostic nasal endoscopy [11]. Our case was diagnosed, based on clinical examination and CT cisternography, which showed site of leak accurately. Surgical management of Cerebrospinal Fluid rhinorrhoea has evolved to a greater extent, from craniotomy through an endonasal approach [12] to an endoscopic endonasal closure [13,14]. A majority of acute post – traumatic Cerebrospinal Fluid leaks resolve spontaneously within 14 days. Initial treatment is always a conservative line, bed rest in decubitus position with a maximum inclination of 10°, fluid restriction, anti-histamines and stool softners [15]. Some authors recommend the routine use of a Lumbar drain post-operatively [16], although recent studies suggest that it should not be performed routinely [17]. Use of prophylactic antibiotics is controversial. Some authors do not adopt a regular prophylaxis [18] and some observed a higher incidence of meningitis in patients who underwent an antibiotic prophylaxis [19]. In our case, we started the patient on intravenous antibiotics, two days prior to surgery and continued for five days post operatively, but a lumbar drain was not done in immediate post-operative period.
Surgical closures through Intracranial route showed a higher incidence of cerebral oedema due to brain retraction, anosmia and haemorrhage. Endoscopic Endonasal closure of Cerebrospinal Fluid rhinorrhoea has gained great support due to decreased morbidity. The major advantages include a better visualisation, reduced hospitalisation, no external scars, no brain retraction, no anosmia and minimal recurrence. The success of Endoscopic closures mainly depend on exact localisation of site of leak and precise placement of graft (underlay/onlay). The contraindications include presence of Intra Cranial lesions, comminuted fractures of skull base, fractures of posterior wall of frontal sinus and lateral extension of frontal sinus fractures. Causes of failures include poor localisation of defects pre – operatively, sphenoid leaks, large Cerebrospinal Fluid leaks [13] and patients with increased intracranial tension [20].
Our case was considered as a surgical challenge due to the size of the defect and the eventful post – operative period. The endoscopic closure of defects which had a size of more than 1 cm was considered as a relative contraindication, due to the high chance of incomplete closures and recurrence. A single layered closure with fascia, which was augmented with surgicel and middle turbinate is done as a standard protocol for cases of cerebro spinal fluid rhinorrhoea. In this case, we successfully attempted a multi layered technique, where a septal cartilage was sandwiched between two layers of fascia, over which multiple layers of surgicel, fibrin glue and pedicle middle turbinate flap were transposed. The post operative period was also challenging, as the patient developed signs of meningism, with a cerebro spinal fluid leak on the third post operative day. It was also managed effectively by conservative methods and intermittent lumbar puncture drainage, thus avoiding revision surgery. Patient is on regular follow up till date, with no evidence of a recurrence.
Conclusion
With an excellent visualisation and high rates of success, Endoscopic Endonasal repair for Cerebrospinal Fluid of rhinorrhoea, is becoming the method of choice for surgical repairs of Cerebrospinal Fluid fistulas. In our case, a single layer closure was not sufficient and hence, a multilayered technique was attempted. Our experience in this case of a successful closure of a bony defect of 1.5cm endoscopically, supports the effectiveness and safety of this procedure. Endonasal Endoscopic closure of Cerebrospinal Fluid leak can be attempted even for large defects, due to stable long term results and an easy second procedure in case of a recurrence.
[1]. Wax MK, Ramadan HH, Ortiz O, Wetmore SJ, Contemporary management of cerebrospinal fluid rhinorrhoeaOtolaryngology-Head and Neck Surgery 1997 116(4):442-49. [Google Scholar]
[2]. Schick B, Ibing R, Bros D, Draf W, Long-term study of endonasal duraplasty and review of the literatureAnn Otol Rhino Laryngol 2001 110:142-47. [Google Scholar]
[3]. Calcaterra T, Diagnosis and management of ethmoid cerebro-spinal rhinorrhoeaOtolaryngol Clin North Am 1985 18:108-15. [Google Scholar]
[4]. Ommaya AK, Wilkins RH, Rengachary SS, Neurosurgery 1996 New YorkMcGraw-Hill:2773-82. [Google Scholar]
[5]. Citardi MJ, Cumming CW, Schuller DE, Thomas TJ, Textbook of Cummings Otolaryngology Head and Neck Surgery 2005 4th ednPhiladelphiaElsevier Mosby:1276-89. [Google Scholar]
[6]. Zlab MK, Moore GF, Daly DT, Yonkers AJ, Cerebrospinal fluid rhinorrhoea: a review of the literatureEar Nose Throat J 1992 71:314-17. [Google Scholar]
[7]. Kizilkilic O, MD, Hypothalamic Hamartoma Associated with a Craniopharygeal canalAmerican Journal of Neuroradiology 2005 26:65-67. [Google Scholar]
[8]. Elias MA,MD, Empty sella syndromeCNS Clinic–Jordan 2005 Online [available] http://pituitaryadenomas.com/emptysella.htm [Google Scholar]
[9]. Dula DJ, MD, Fales F, MD, The ‘Ring Sign’: Is it a reliable Indicator for Cerebral Spinal Fluid?Annals of Emergency Medicine 1993 22:718-20. [Google Scholar]
[10]. Moyer P, Beta-Trace Protein Shows Promise as a marker for diagnosing cerebrospinal fluid LeaksDoctor’s Guide 2002 Online [Available]: http://www.docguide.com/dg.nsf/printPrint/5DF097A1EB04B3FA85256C3E00731E65 [Google Scholar]
[11]. Jones ME, Reino T, Gnoy A, Guillory S, Wackim P, Lawson W, Identification of intranasal cerebrospinal fluid leaks by topical application with fluorescein dyeAm J Rhinol 2000 14:93-96. [Google Scholar]
[12]. Vrabec DP, Hallberg OE, cerebrospinal fluid rhinorrhoea by endonasal surgeryArch Otolaryngol 1964 80:218-29. [Google Scholar]
[13]. Wigand ME, Transnasal ethmoidectomy under endoscopic controlRhinology 1981 19:7-15. [Google Scholar]
[14]. Papay FA, Maggiano H, Dominguez S, Hassenbusch SJ, Levine HL, Lavertu P, Rigid endoscopic repair of paranasal sinus cerebrospinal fluid fistulasLaryngoscope 1989 99:1195-201. [Google Scholar]
[15]. Locatelli D, Rampa F, Acchiardi I, Bignami M, De Bernadi F, Castelnuvo P, Endoscopic endonasal approaches for repair of cerebrospinal fluid leaks: nine year experienceNeurosurgery 2006 58:246-57. [Google Scholar]
[16]. McCoy G, cerebrospinal fluid rhinorrhoea : a comprehensive review and a definition of the responsibility of the rhinologist in the diagnosis and the treatmentLaryngoscope 1963 73:1125-57. [Google Scholar]
[17]. Cassiano RR, Jassir D, Endoscopic cerebrospinal fluid rhinorrhoea repair: is a lumbar drain necessary?Otolaryngol Head Neck Surg 1999 121:745-50. [Google Scholar]
[18]. Nachtigal D, Frenkiel S, Mohr G, Endoscopic repair of cerebrospinal fluid rhinorrhoea: Is it the treatment of choice?The Journal of Otolaryngology 1999 28(3):129-33. [Google Scholar]
[19]. Choi D, Span R, Traumatic cerebrospinal fluid leakage: risk factors and the use of prophylactic antibioticsBr J of Neurosurgery 1996 10:571-75. [Google Scholar]
[20]. Mirza S, Thaper A, McClelland I, Jones NS, Sinonasal cerebrospinal fluid leaks management of 97 patients over 10 yearsLaryngoscope 2005 115:1774-77. [Google Scholar]