Teratocarcinoma In A Non Seminomatous, Mixed Germ Cell Tumour of the Testis-A Rare Entity
Gayathri Malavalli1, Shilpa Karra2, Bharathi Muniyappa3
1 Assistant Professor, Department of Pathology,
2 Associate Professor, Department of Pathology,
3 Professor, Department of Pathology, Mysore Medical College & Research Institute, Mysore-570007, India.
Name, Address, E-Mail Id of The Corresponding Author: Dr Gayathri Malavalli, Assistant Professor, Department of Pathology, MMC&RI, Mysore-570007, India.
Phone: +9945629613
E-mail: drgayathri1967@gmail.com
Mixed Germ Cell Tumours (MGCTs) of the testis are the second most common testicular tumours. In the 10 years retrospective study which was done on testicular neoplasms at our institute, this reported case accounted for 0.4%. We are presenting the case of a 30 year old male with a painless testicular swelling. Abdominal ultrasonography disclosed it as a seminoma and the FNAC report was Mixed Germ Cell tumour of the testis. Histopathology concurred the cytological diagnosis and it additionally revealed the concomitant presence of a Yolk Sac Tumour (YST) and a Teratocarcinoma in a Non-Seminomatous Tumour of the testis. This case attains uniqueness with the very rare presence of the yolk sac tumour with the teratocarcinoma component in Non-Seminomatous Testicular Tumours. The reason behind the reporting of the case was its poor therapeutic response.
Non seminomatous testicular tumour, MGCT, YST, Teratocarcinoma
Introduction
The incidence of testicular tumours in Asia is only 0.4/100000 [1]. Mixed germ cell tumours are the second most common testicular germ cell tumours following seminomas and they account for 40-45% of all the primary testicular GCTs [2].
A teratocarcinoma is composed of undifferentiated stem cells and their more differentiated derivatives. The stem cells of teratocarcinomas are equivalent to the embryonal carcinoma cells, which are malignant cells with vescicular, irregular nuclei and a cytoplasm that has indistinct borders. The nuclei show overcrowding and they overlap one another. The chromatin is coarsely clumped along the nuclear membrane and a prominent nucleolus and by extrapolation to the undifferentiated cells in the early embryo. Developmentally, they correspond to the embryonic cells in the pre-gastrulation embryo, before the separation of the embryonic from the extra-embryonic lineages and before the formation of the germ layers. The stem cells of teratocarcinomas may differentiate into embryonic tissues which are derived from all the three germ layers on one hand and into extra-embryonic cells on the other.
Studies have shown that the human EC (embryonal cells) lines may differentiate into somatic tissues and that under the appropriate conditions, they may lose their malignancy and cease to proliferate. After chemotherapy, the teratocarcinoma stem cells can differentiate into non-proliferating somatic tissues [3]. The MGCTs are composed of two or more different germ cell tumour components, the commonest being a teratoma, an embryonal carcinoma, a yolk sac and syncytiotrophoblasts. Although teratomas are common, a malignant transformation is an uncommon occurrence and it highlights the need for its recognition, as it is resistant to the current chemotherapeutic regimens.
Case
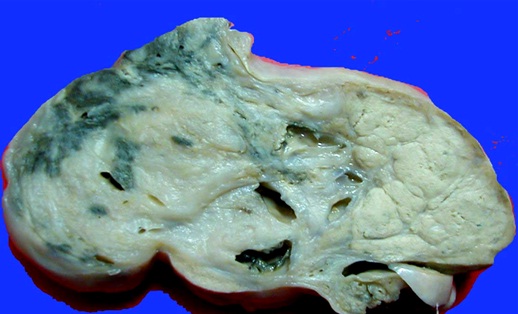
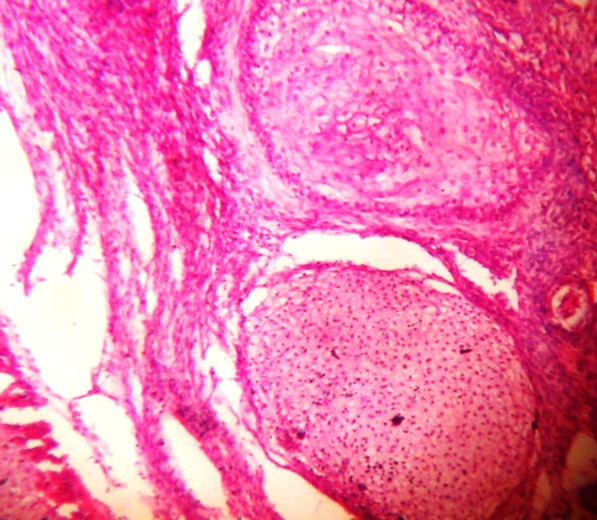
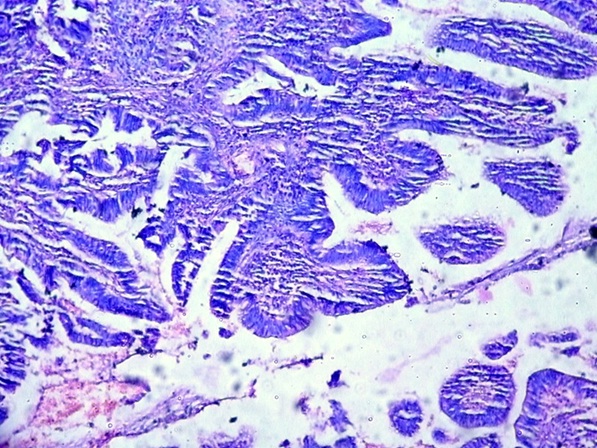
A 30 year old male presented to the surgery OPD with a history of swelling and dragging pain over the right side of the scrotum since 15 days. A scrotal ultrasound which was done, revealed an enlarged, minimally echogenic right testis which measured 8.2x5.8x6.2 cms, with multiple cystic areas and a minimal increase in its vascularity. A radiological diagnosis of a seminoma was opined. The left testis appeared to be normal. The serum alpha feto protein was elevated. Fine needle aspiration cytology reported it as an MGCT. A right high orchidectomy was performed and the specimen was sent for a histopathological examination. The gross examination showed an enlarged testis which measured 8.5x6x5.5 cms, with the spermatic cord measuring 7x2 cms. The cut surface was variegated, with multiple tiny cystic areas which were admixed with small areas of necrosis [Table/Fig-1]. On microscopy, the presence of NSGCT elements were identified-a YST and a teratoma. The major proportion was that of the teratoma, which was composed of cartilaginous tissue. Also seen were glands, tubules and stroma which was composed of spindle cells [Table/Fig-2]. One focus showed an evidence of an adenocarcinoma [Table/Fig-3]. The YST element and myxoid stroma. These were seen adjacent to the areas of necrosis. A diagnosis of a mixed germ cell tumour of the testis which was composed of a teratoma with a malignant transformation an adenocarcinoma and a yolk sac tumour in the NSTT was made.
Gross Enlarged testis C/S shows solid, cystic and mucoid areas
HP (300x.) Showing areas of cartilage, sebaeceous gland, spindle cells and myxoid stroma
HP (300x.) Multiple Papillary Structures lined by malignant cells-Teratocarcinoma
Discussion
The MGCTs are commonly composed of a YST and a Teratocarcinoma [4]. On the contrary, NSTTs with Teratocarcinomas is an infrequent occurrence. This retrospective study was conducted in the Department of Pathology, MMCRI, Mysore, India, from Jan 2002 to Dec 2012. During this period, a total of 342 orchidectomy specimens were received, out of which 23 were malignant, as has been shown in [Table/Fig-4], among which a teratocarcinoma in a non-seminomatous mixed germ cell tumour was reported for the first time in this institution. A majority of the lesions were observed in the third and fourth decades of life. Henceforth, a periodic survey should be an integral part, to know the incidence of a TC in an NSTT, which may serve in improving its management, which is the ultimate goal of the medical field.
Retrospective study of testicular tumor for a period of 10 years (2002-2012)
| Sl No. | Diagnosis | Total no. of cases |
|---|
| 1 | Seminoma | 06 |
| 2 | Non-seminomatous seminoma | 01 |
| 3 | Teratoma | 01 |
| 4 | Yolk sac tumor | 02 |
| 5 | Teratocarcinoma | 03 |
| 6 | Mixed germ cell tumor | 04 |
| 7 | Non-Hodgkins Lymphoma | 01 |
| 8 | Mixed Germ Cell Tumor with Malignant Transformation in Non-Seminomatous Seminoma. | 01 |
| 9 | Paratesticular tumor infiltration into testis | 04 |
In view of the current management protocol for testicular tumours, it is important to mention the different elements with their relative proportions in the MGCTs. Although YSTs are common components of the MGCTs, they present diagnostic difficulties due to their diverse morphological patterns. It has been observed that the YST tissues occur more frequently in the adult testicular tumours and in the MGCTs, they can be expected to dictate the behaviour, except when they are combined with seminomas. The adults with the YST components of the MGCTs usually have increased frequencies of stage 1 disease [5]. Teratomas with malignant transformations are rare in the testis. They generally contain the malignant tumours which are typically encountered in the other organs. The prognosis for the patients with the Sarcomatous element is generally poor [6, 7]. The teratomas with malignant transformations are generally metastatic at presentation, they have high recurrence rates and they are more aggressive. The malignant teratomas were found to be significantly resistant to the current chemotherapeutic regimen [8, 9], which was demonstrated by their poor radilogical responses to the treatment. Although, radiology and cytology help in the diagnosis of the MGCTs, a histopathological examination is required to enumerate the different elements which are present and their relative proportions, which ultimately have prognostic values and implications on the management of the patients, as was seen in this case which had malignant transformations of the teratomas in NSTTs [10] at our institution.
[1]. Parkin DM, Bray F, Ferlay J, Pisani P, Global Cancer Statistics 2002 [Google Scholar]
[2]. Eble JN, Sauter G, Epstein JI, Sesterhenn I, WHO Classification of tumors. Pathology and GeneticsTumors of the urinary system and male genital organs 2004 Lyon, FranceIARC Press [Google Scholar]
[3]. Damjanov Ivan, Linder James, Anderson’s Pathology 2009 210e:2184-85. [Google Scholar]
[4]. Mosharafa Ashraf A, Foster Richard S, Leibovich Bradley C, Ulbright Thomas M, Histology in mixed germ cell tumor. Is there a favorite pairingThe journal of Urology 2004 171:1471-73. [Google Scholar]
[5]. Talerman A MD, The incidence of Yolk sac tumor elements in germ cell tumor of testis in adultsCancer 1975 36:211-15. [Google Scholar]
[6]. Leibovitch I, Foster RS, Ulbright TM, Donohue JP, Adult primary pure teratoma of testis. The Indian experienceCancer 1995 75:2244-50. [Google Scholar]
[7]. Comiter Craig V, Kibel Adam S, Richie Jerome P, Nucci Marisa R, Renshaw Andrew A, Prognostic features of teratomas with malignant transformation. A Clinicopathologic study of 21 casesThe journal of Urology 1998 159:859-63. [Google Scholar]
[8]. Spies PE, Pisters LL, Liu P, Pettaway CA, Kamat AM, Gomes JA, Malignant transformation of testicular teratoma: a chemoresistant phenotypeUrologic Oncology 2008 26:595-99. [Google Scholar]
[9]. Donadio Alessia C, Motzer Robert J, Bojorin Dean FB, Kantoff Philip W, Sheinfeld Joel, Chemotherapy for teratoma with malignant transformationJournal of Clinical Oncology 2003 21:4285-91. [Google Scholar]
[10]. Michael H, Non-germ cell tumor arising in patient with testicular germ cell tumorThe journal of Urology Pathology9:39-60. [Google Scholar]