Significance of Prophylactic Paratracheal Lymphnode Dissection in A Case of Retrosternal Goitre: A Case Report
Kathir Chandramouleeswari1, Shivali Budhiraja2, Anita Suryanarayan3, Jagdeesh Chandra Bose4
1 Associate Professor, Department of Pathology, Stanley Medical College, Consultant Pathologist, Lister Metropolis, Chennai, India.
2 Junior Pathologist, Lister Metropolis Labortaory, Chennai, India.
3 Chief of Laboratory Services, Lister Metropolis Labortaory, Chennai, India.
4 Professor & Head, Department of Surgical Oncology, Madras Medical College, Chennai, India.
Name, Address, E-Mail Id of The Corresponding Author: Dr Shivali Budhiraja, Junior Pathologist, Lister Metropolis Labortaory, Chennai, Tamil Nadu, India.
Phone: 08056081270 E mail: doctorshivali@gmail.com
An elective or a prophylactic lymph node dissection is the removal of the lymph nodes that are normal on physical examination and on radiographic imaging. This type of dissection is not based on the visible disease in the targeted nodal basins, but on the potential of a radiographically occult tumour which can exist. The pathologic results of an elective lymph node dissection may help in predicting the risk of a future recurrence and, in some solid tumours, guide the delivery of the adjuvant therapy and as in this case, may contribute to a pathological diagnosis. The decision to proceed with an elective node dissection is based on the assessment of the risks and benefits of the procedure. The morbidity of the regional lymph node dissection must be balanced against the potential benefit of the procedure. A thyroid papillary microcarcinoma is defined according to the WHO criteria and Shaha as a thyroid tumour which is smaller than 1–1.5cm. Different terms are currently used to define this thyroid cancer such as small, tiny, minute, minimal or occult papillary carcinomas of the thyroid, impalpable thyroid carcinoma and incidental thyroid papillary cancer. A common clinical scenario is the incidental diagnosis of papillary thyroid microcarcinoma (PTMC) on the histology of the resected thyroid, following the surgery which was done for a presumably benign thyroid disease. PTMC was diagnosed in 7.1% of the patients with a presumably benign thyroid disease. It may be possible that this is an underestimation of the true incidence, because we did not use the serial sectioning technique and maybe because the PTMC which was present was so small that it was grossly not identified and sectioned. Herein, a case which was clinically suspicious and was radiologically and cytologically diagnosed as a case of retrosternal multinodular goitre underwent a near total thyroidectomy and a paratracheal lymphnode dissection. The node was found to have micrometastasis of the follicular variant of a papillary carcinoma and the thyroid, on a retrospective step sectioning, revealed an incidental PTMC. This case has been presented, to highlight the possibility of an incidental PTMC in the thyroid cases which were resected for benign disease and the importance of elective lymphnode dissection in contributing to the diagnosis of PTMC.
Incidental papillary microcarcinoma, Prophylactic lymphadenectomy
Case Report
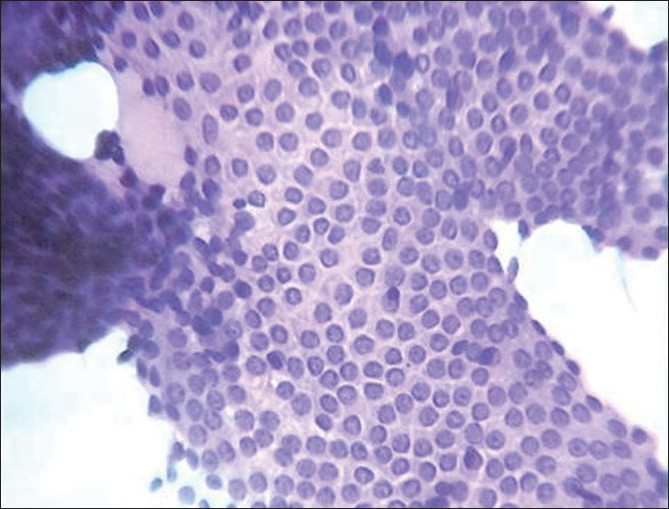
A 70 years old male presented with a swelling in the front of the neck, which was accompanied by dyspnoea, dysphagia and a choking sensation. His TSH level was 1.4 mIU/L and his free T4 level was 1.5 μg/dL. The patient did not give any family history of a malignancy or a history of irradiation of the cervical region for any malignancy. Ultrasound of the thyroid swelling was done, which showed gross enlargement of both the lobes of the thyroid, with multiple nodules of varying sizes. CT was done and it did not reveal any space occupying lesion anywhere else in the body. A clinical diagnosis of a multinodular goitre was suggested and the patient was sent for fine needle aspiration cytology (FNAC). The cytology smear showed monolayered sheets and clusters of thyroid follicular epithelial cells which were admixed with bare nuclei, in a background of colloid and haemorrhage [Table/Fig-1]. A diagnosis of a multinodular goitre was made on FNAC.
Fine needle aspiration cytology picture showing monolayered sheets of thyroid follicular epithelial cells in colloid background. H & E 40x view
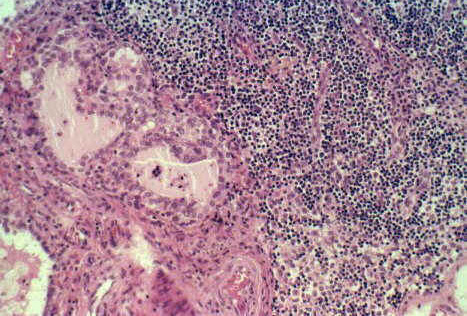
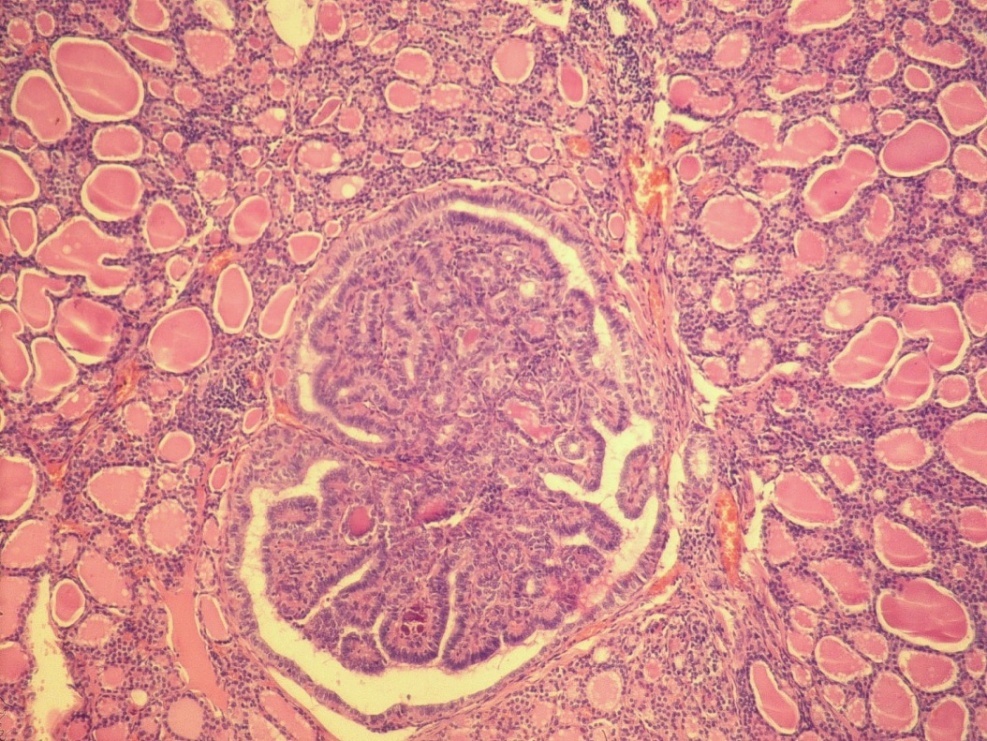
The patient was taken up for surgery and a near total thyroidectomy with a right and left prophylactic paratracheal lymph node dissection was done. For the histopathological examination, we sent a specimen of the thyroid, which measured 9x7x6 cms, which included the right lobe, the left lobe and the isthmus. The surface of the thyroid appeared to be lobulated. Its cut surface showed grey brown, solid and cystic areas. The cysts were filled with colloid.The lymph nodes measured 0.8 cms each and the cut sections of the nodes were grey brown. The representative sections were taken and they showed thyroid tissue which was composed of multiple colloid filled follicles which were lined by flattened follicular epithelial cells. The interfollicular area showed foci of haemorrhage and fibrosis and areas of calcification. A pathological diagnosis of a multinodular goitre was thought of but when the paratracheal lymph nodes were examined, two of the three left paratracheal lymph nodes showed micrometastasis of the follicular variant of the papillary carcinoma, which occupied more than one half of each lymph node [Table/Fig-2]. Then retrospectively ,the entire right lobe, left lobe and the remaining tissue were embedded and studied, which revealed a follicular variant of a papillary microcarcinoma at one focus, which measured 0.8x0.6 cms in the left lobe [Table/Fig-3].
Lymphnode micrometastasis of follicular variant of papillary carcinoma. H&E 40x view
PTMC in the left lobe of thyroid H&E 40x view
Discussion
Autopsy studies tell us that 3-4% of the adult population harbours micro papillary carcinomas of the thyroid without any apparent ill effects [1]. Approximately 1 in 15 patients who undergo thyroidectomy for benign disease are found to have an incidental 1-2 mm focus of thyroid cancer on careful pathologic examinations [2]. In our case, PTMC was diagnosed in the thyroid specimens which were resected for benign disease and this was done only after the detection of micrometastasis in the paratracheal node which was dissected in view of the clinical suspicion .This emphasizes the practice of sentinel lymph node (SLN) biopsies, frozen sections and prophylactic lymphadenectomies of the paratracheal nodes in patients with incidental thyroid cancer, who undergo surgeries for benign disease of the thyroid [3–6].
The thyroid follicles which were found in two of the left paratracheal lymphnodes had to be differentiated from the benign thyroid inclusions. Inclusions of the thyroid type are frequently found in cervical and axillary lymph nodes (Gritsman and Schwartz,1985) and they were considered in the differential diagnosis when initially, multiple sections did not reveal a tumour in the thyroid tissue .The criteria for establishing a diagnosis [1] of benign inclusions of the thyroid type in the lymph nod es are: (1) The inclusions must be microscopic and they should be located in the subcapsular sinus of the lymph node or in close contact with it, and they should be generally solitary; (2) The follicles must be of regular size, containing abundant colloid, and the cells of the cuboid type should be arranged in a single uniform line. Furthermore, they must not present atypical structures such as nuclear hyperchromasia, atypical mitotic figures, papillary structures or psammomatous bodies; and (3) The thyroid gland must be clinically normal and non-palpable (Ibrahim et al., 1981). By using these criteria strictly, the thyroid tissue which was found in the lymph node was diagnosed as a micrometastasis from the thyroid tumour, after which the entire thyroid tissue was embedded and a PTMC was identified.
The central cervical compartment is the primary zone of the lymphatic involvement for all the thyroid cancers except those which are located in the upper pole of the glands, from which the lymphatic drainage may flow directly into the lateral neck nodes. Since 1993, all the patients underwent neck ultrasonographies for the presurgical assessment of the cervical lymph-node metastases. Prior to 1996, level VI cervical lymph-node compartment dissections were performed only when lymph-node metastases were identified preoperatively or during surgery; however, after 1996, all the patients with presurgical cytologic evidences of incidental PTMCs underwent total thyroidectomies with pretracheal and ipsilateral paratracheal lymph-node dissections if a frozen-section specimen revealed metastases in a dissected lymph node. The patients with lymph-node metastases in the lateral compartments underwent modified neck dissections in the cervical lymph-node-compartment levels II and IV. Mercante et al., performed neck lymph-node compartment dissections in 226 patients (50%), of whom 166 (73%) did not have presurgical evidences of lymph-node metastases but had undergone total thyroidectomies with prophylactic level VI (central) cervical compartment dissections, while 60 (27%) others with presurgical evidences of cervical lymph-node metastases had undergone total thyroidectomies with therapeutic central compartment and lateral neck dissections. The effect of the initial therapy thyroid surgery, lymph-node compartment dissections, and radioiodine therapy in a group of patients with papillary microcarcinomas, half of whom had their tumours discovered during surgery for multinodular goitre (n = 103) has been difficult to identify and hence we published this case report.
PTMC was associated with 3.5% of the patients who had experienced a recurrence after a median of 10.3 years.But the 30-year recurrence rate was 40% in the patients who were older than 55 years and it was less than 10% in the patients who were younger than 55 years. The recurrence rates after 35 years of follow-up were 3% for the tumours which had sizes of 1 to 5 mm. Almost all of the recurrences were in the neck. Of the 2070 patients who underwent follow-ups for 16.5 ± 7.3 years, only 12 (0.6%) had died of thyroid cancer [7]. Because of the general favourable outcome in most of the patients with PTC, whether the improved detection of the early lymph node metastases and the clearance which is afforded by the prophylactic lymphadenectomy or simply an increase in the extent of the neck dissection without a clinically meaningful impact on the locoregional disease control or survival will be viewed as a clinical progress, remains unknown.
However, this case reiterates the following facts: namely, the thyroid tissues which are resected for a benign diagnosis should be carefully evaluated for the presence of PTMC. An elective paratracheal lymphadenectomy also contributes to the diagnosis of PTMC apart from its other benefits The thyroid tissue in the lymph nodes should be evaluated by using the stringent criteria which have been described above, to differentiate between the benign thyroid inclusions and the micrometastasis from papillary carcinomas.
[1]. Mazzaferri EL, Young RL, Papillary thyroid carcinoma: a 10 year follow-up report of the impact of therapy in 576 patientsAm J Med 1981 70:511-8. [Google Scholar]
[2]. Samaan NA, Maheshwari YK, Nader S, Impact of therapy for differentiated carcinoma of the thyroid: an analysis of 706 casesJ Clin Endocrinol Metab 1983 56:1131-8. [Google Scholar]
[3]. Kelemen PR, Van Herle AJ, Giuliano AE, Sentinel lymphadenectomy in thyroid malignant neoplasmsArch Surg 1998 133:288-92. [Google Scholar]
[4]. Fukui Y, Yamakawa T, Taniki T, Sentinel lymph node biopsy in patients with papillary thyroid carcinomaCancer 2001 92:2868-74. [Google Scholar]
[5]. Stoeckli SJ, Pfaltz M, Steinert H, Schmid S, Sentinel lymph node biopsy in thyroid tumors: a pilot studyEur Arch Otorhinolaryngol 2003 260:364-68. [Google Scholar]
[6]. Rubello D, Pelizzo MR, Al-Nahhas A, The role of sentinel lymph node biopsy in patients with differentiated thyroid carcinomaEur J Surg Oncol 2006 32:917-21. [Google Scholar]
[7]. Noguchi S, Yamashita H, Uchino S, Watanabe S, Papillary microcarcinomaWorld Journal of Surgery 2008 32(5):747-53. [Google Scholar]