Rare Case of Ileal Perforation
Vinod Kumar B1, John Joseph S Martis2, Sheldon G Mathias3, Priyatham Kamath4, Vivek Shetty5
1 Senior Resident, Department of General Surgery, Father Muller Medical College, Mangalore, Karnataka – 575002, India.
2 Professor, Department of General Surgery, Father Muller Medical College, Mangalore, Karnataka – 575002, India.
3 Senior Resident, Department of General Surgery, Father Muller Medical College, Mangalore, Karnataka – 575002, India.
4 Senior Resident, Department of General Surgery, Father Muller Medical College, Mangalore, Karnataka – 575002, India.
5 Resident, Department of General Surgery, Father Muller Medical College, Mangalore, Karnataka – 575002, India.
Name, Address, E-Mail Id of The Corresponding Author: Dr Vinod Kumar B, S/o Rukmaya B, Mayyarabailu, Balehithlu house, Bantwal, D.K, Karnataka – 574211, India.
Phone: 9611321700
E-mail: vinnudoc1998@yahoo.co.in
Ileitis, or inflammation of the ileum, is often caused by Crohn’s disease. However, ileitis may be caused by a wide variety of other diseases. These include infectious diseases, spondyloarthropathies, vasculitides, ischemia, neoplasms, medication-induced, eosinophilic enteritis, and others. Eosinophilic enteritis can present as abdominal pain, protein loosing enteropathy, ulcers, intestinal obstruction, intussusception and perforation.Bowel perforation is an uncommon presentation of eosinophilic enteritis. We report a rare case of ileal perforation due to eosinophilic enteritis in a 57 years old female.
Eosinophilic ileitis, Ileal perforation, Laparotomy
Introduction
Ileitis, which is defined as an inflammation of the ileum, is classically caused by Crohn’s Disease (CD). However, a wide variety of diseases may be associated with ileitis. These include infectious diseases, spondyloarthropathies, vasculitides, ischaemia, neoplasms, drug-related diseases, eosinophilic enteritis, amyloidosis, and a variety of other conditions [1]. Eosinophilic ileitis is observed mainly in three coastal areas in Holland, Japan and Britain [2]. Although the aetiology is unknown, a personal or family history of food allergies and atopic disorders is present in 50% to 70% of the cases. The proposed pathogenesis is an alteration in the mucosal integrity, which results in the localization of various antigens in the gut wall, thereby inducing tissue and blood eosinophilia [3]. The clinical features vary, depending on the layers and the extent of the bowel which is involved with the eosinophilic infiltration. Small – bowel eosinophilic enteritis may present with abdominal pain, diarrhoea, or malabsorption. Ileal strictures and bowel obstructions may occur with a muscle layer involvement and eosinophilic ascites may manifest if the serosa is affected. The uncommon presentations of eosinophilic gastroenteritis include an acute abdomen, a colonic obstruction, eosinophilic ascites, and bowel perforations [4–6]. We are reporting a rare case of an ileal perforation which was caused by eosinophilic enteritis, which was treated successfully by surgery in a 57-years old female.
Case Report
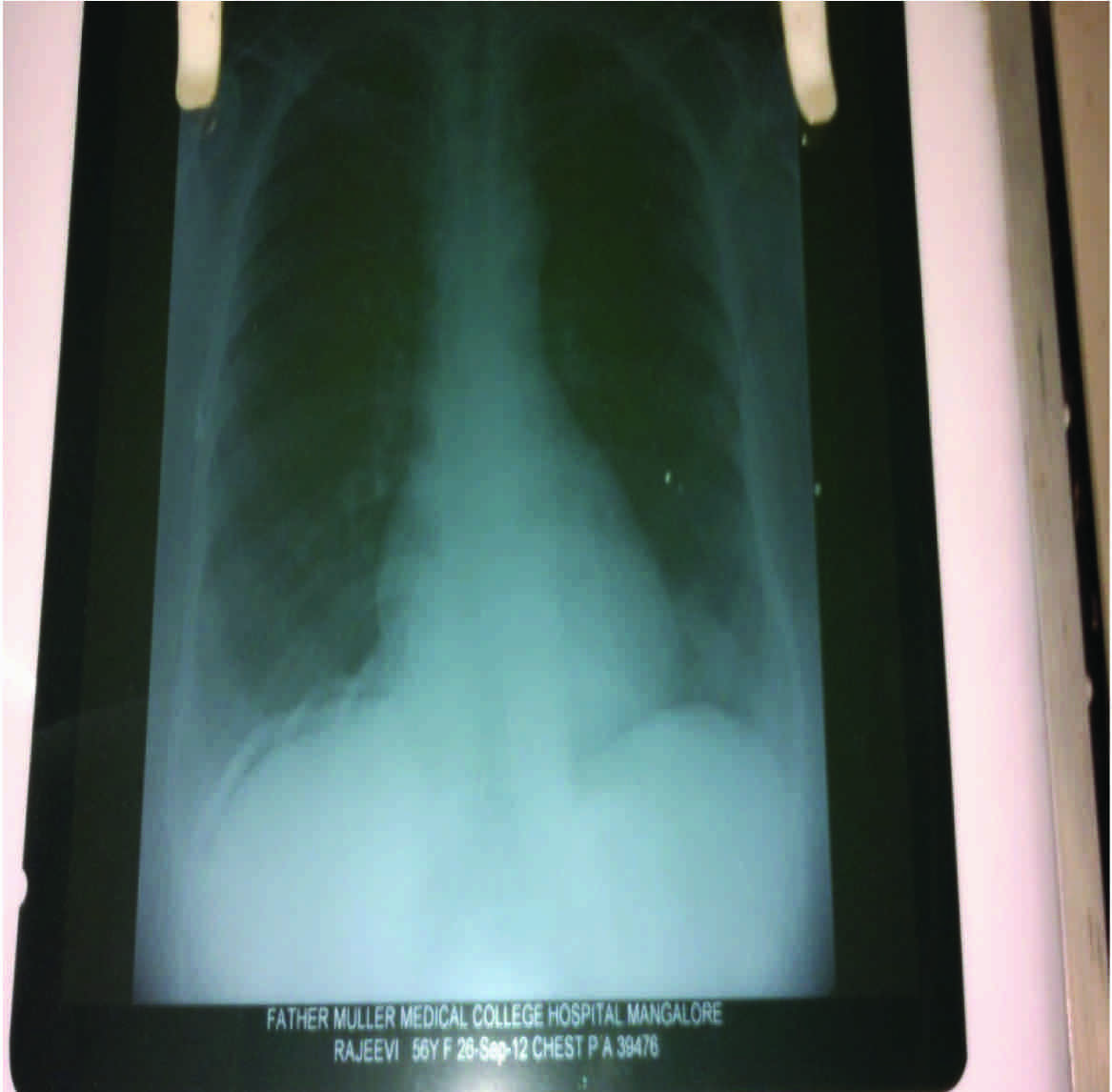
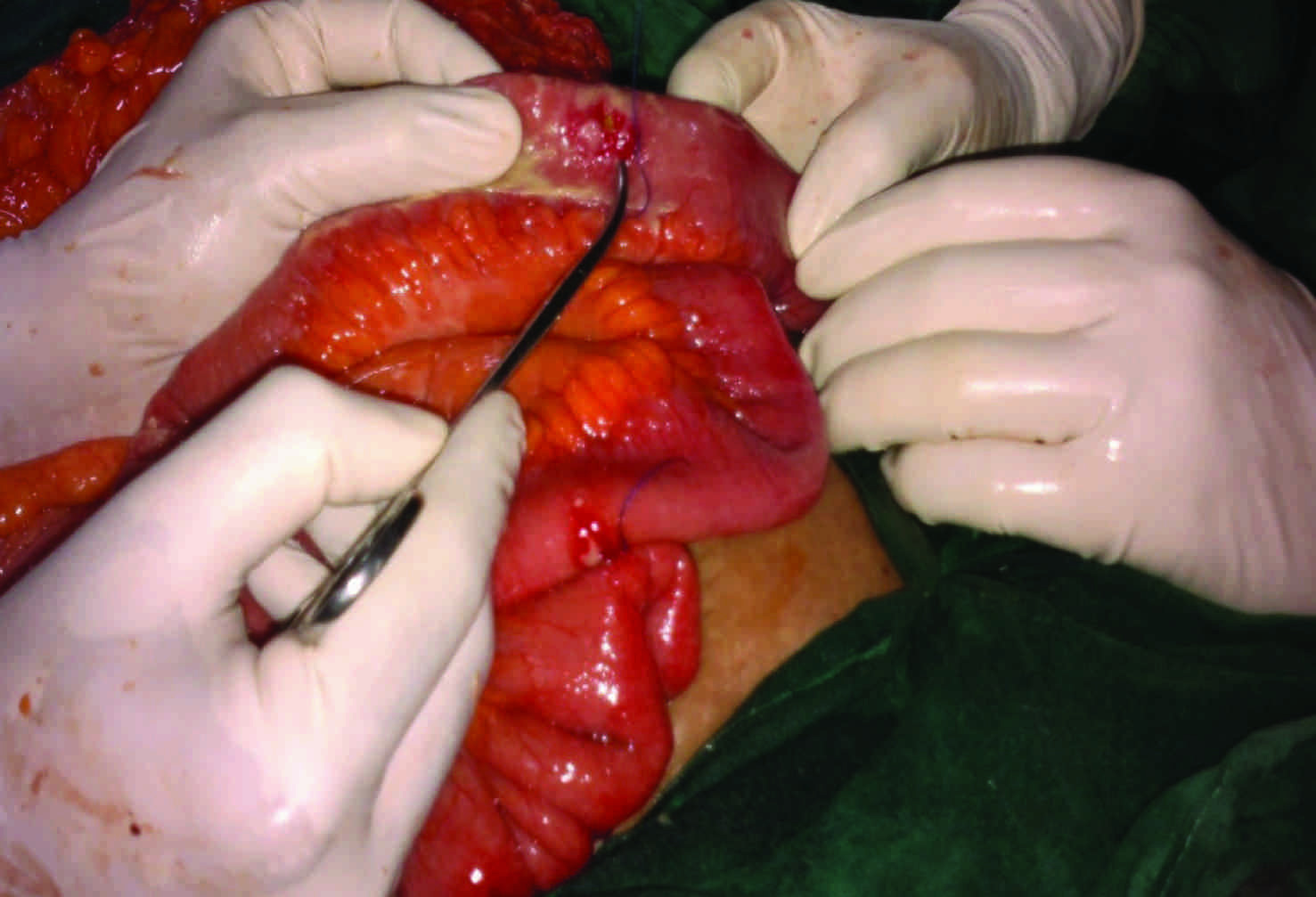
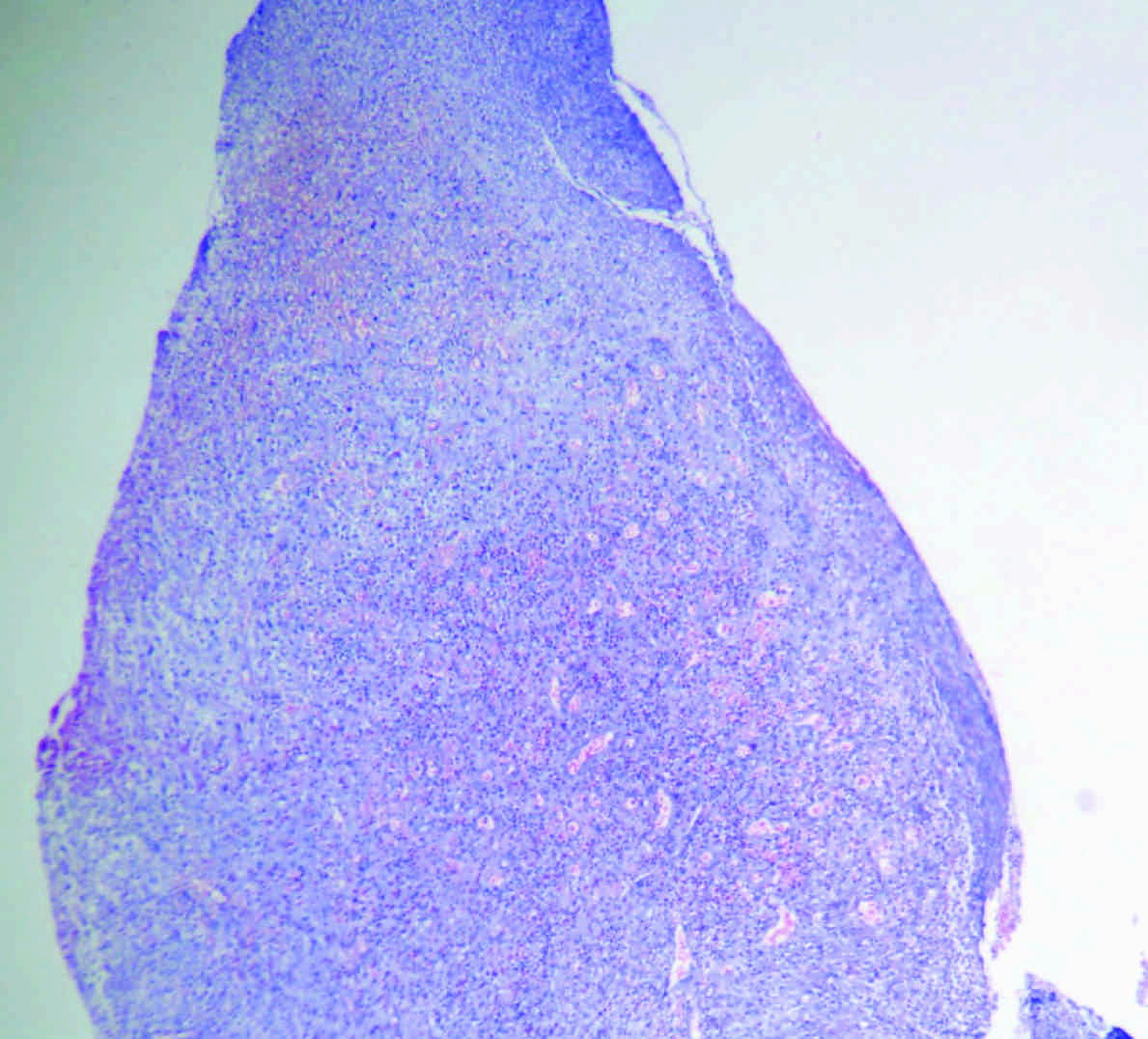
A 57 years old woman presented with pain in the abdomen, of one day’s duration. Her past history was not contributory. Her general physical examination was unremarkable. On abdominal examination, a generalized distension with guarding and rigidity and absent bowel sounds was seen. The chest X-ray (PA view) showed air under the diaphragm [Table/Fig-1]. The differential count was neutrophils – 68, lymphocytes – 32 and eosinophils – 1. After resuscitation, an exploratory laparotomy was done and it showed copious amounts of bilious fluid with flakes in the peritoneal cavity. An ileal perforation which measured about 5mm was present about 50cm from the ileocaecal junction, with surrounding erythema [Table/Fig-2]. Segmental resection of the small intestine and peritoneal lavage was done.The patient made an uneventful recovery. She is on regular follow up and has not been started on steroids. The histopathological examination of the excised specimen revealed an ileal tissue with ulceration, necrosis, granulation tissue and infiltration by inflammatory cells, which was composed predominantly of eosinophils, few lymphocytes and histiocytes, which were suggestive of eosinophilic ileitis [Table/Fig-3].
Chest X-ray PA view showing air under diaphragm
Intraoperative picture showing site of perforation with surrounding erythema
Histopathologicalpicture showingileal tissue with inflammatory cells predominantly eosinophils –eosinophilic ileitis
Discussion
Eosinophilic enteritis is defined as an inflammation with a characteristic eosinophilic infiltration of the bowel wall, in which various layers can be affected, which occurs anywhere along the gastrointestinal tract, from the oesophagus to the rectum [7]. Shaped in large part by case reports and series over the years, there are no strict diagnostic criteria for this disorder. Rather, a combination of the gastrointestinal complaints with supportive histologic findings is sufficient to make the diagnosis. Serum eosinophilia is present in many cases. It is a relatively rare entity which had been previously described in association with conditions such as collagen vascular disease, malignancy, food allergy, parasitic or viral infections, inflammatory bowel disease, and drug sensitivity [8–11]. The proposed pathogenesis is an alteration in the mucosal integrity which results in the localization of various antigens in the gut wall, thereby inducing tissue and blood eosinophilia [3]. Primary eosinophilic enteritis has also been described, where no precipitating factors can be identified, which lead to such an inflammation [7]. It can present with various symptoms such as abdominal pain, protein-losing enteropathy, ulcers, ascites, obstruction, intussusception and perforation and it can mimic inflammatory bowel disease [12–14]. A granulomatous formation has also been described along with the eosinophilic infiltration [15]. Typhoid ileitis is generally considered to be the most common cause of the perforations of the terminal ileum. Not all ileal perforations, however, are caused by typhoid. The reports in the foreign literature have documented other possible aetiologies’ of the ileal perforations. Among them are Campylobacter, Escherichia coli, Streptococcus and Haemophilus and Yersinia [16,17]. The surgical treatment of an eosinophilic ileal perforation consists of a segmental resection of the involved bowel segment.
Conclusion
A typhoid ileal perforation is the most common cause of an ileal perforation. Eosinophilic ileitis one of the rare causes of the non-typhoid ileal perforations. A careful intraoperative examination is required. Laparotomy and segmental resection are the recommended treatments for this condition. This case has been presented because of its rarity.
[1]. DiLauroand Steven, Crum-Cianflone Nancy F, Ileitis: when it is not Crohn’s diseaseCurr Gastroenterology Rep 2010 August 12(4):249-58. [Google Scholar]
[2]. Germain M, Lemaigre G, Lapierre J, Lenriot JP, Eosinophilic ileitisJ Chir. (Paris) 1977 114(5):377-84. [Google Scholar]
[3]. Daneshjoo R, Talley J N, Eosinophilic gastroenteritisCurr Gastroenterology Rep 2002 Oct 4(5):366-72. [Google Scholar]
[4]. Khan S, Orenstein SR, Eosinophilic gastroenteritis masquerading as pyloric stenosisClin Paediatr (Phila) 2000 39:55-57. [Google Scholar]
[5]. Shweiki E, West JC, Klena JW, Eosinophilic gastroenteritis presenting as an obstructing cecal mass—a case report and review of the literatureAm J Gastroenterology 1999 94:3644-45. [Google Scholar]
[6]. Huang FC, Ko SF, Huang SC, Eosinophilic gastroenteritis with perforation mimicking intussusceptionJ Paediatr Gastroenterology Nutr 2001 Nov 33(5):613-15. [Google Scholar]
[7]. Rothenberg ME, Eosinophilic gastrointestinal disorders (EGID)J Allergy Clin Immunol 2004 Jan 113(1):11-28.Quiz 29 [Google Scholar]
[8]. Sunkureddi PR, Luu N, Xiao SY, Tang WW, Baethge BA, Eosinophilic enteritis with systemic lupus erythematosusSouth Med J 2005 Oct 98(10):1049-52. [Google Scholar]
[9]. Shakeer VK, Devi SR, Chettupuzha AP, Mustafa CP, Sandesh K, Carbamazepine-induced eosinophilicenteritisIndian journal of gastroenterology 2002 May-Jun 21(3):114-15. [Google Scholar]
[10]. Montalto M, Miele L, Marcheggiano A, Santoro L, Curigliano V, Anisakis infestation: A case of acute abdomen mimicking Crohn’s disease and eosinophilic gastroenteritisDig Liver Dis 2005 Jan 37(1):62-64. [Google Scholar]
[11]. Gonsalves N, Food allergies and eosinophilic gastrointestinal illnessGastroenterology Clin North Am 2007 Mar 36(1):75-91. [Google Scholar]
[12]. Clegg-Lamptey JN, Tettey Y, Wiredu EK, Kwawukume EY, Eosinophilic enteritis – a diagnostic dilemmaWest Afr J Med 2002 July-Sep 21(3):258-59. [Google Scholar]
[13]. Bouhmidi A, Lorente Poyatos R, Romero Cara P, Ibanez Martin JJ, Casado Caballero F, Eosinophilic enteritis as a rare cause of ascites (in Spanish)Gastroenterol Hepatol 2003 Oct 26(8):480-81. [Google Scholar]
[14]. Biswas S, Hoo W, Katsoulas N, Munro J, Oke O, Eosinophilic enteritis: A rare cause of abdominal painInt J Colorectal Dis 2007 Jan 22(1):87-88. [Google Scholar]
[15]. Walia HS, Abraham TK, Walia HK, Eosinophilic enteritis with perforationCan J Surg 1988 Jul 31(4):268-69. [Google Scholar]
[16]. Boyd JF, Acute iletisBr Med J 198l 283:1333 [Google Scholar]
[17]. Morain CO, Acute ileitisBr Med J 1981 Oct24 283(6299):1075-76. [Google Scholar]