Introduction
Inflammatory Pseudotumour of the spleen is an uncommon benign lesion of uncertain aetiology. It presents as a well-circumscribed mass which is usually solitary and composed of foci of inflammatory cells, mainly plaasma cells and lymphocytes in a fibroblastic stroma [1]. Cotelingam and Jaffe first described it in 1984 [2]. It is a distinct entity with specific histopathological, immunohistochemical and molecular characteristics. IPTs have been reported to occur at diverse anatomic sites such as the orbit, spinal canal, meninges, digestive system, heart, mesothelial membranes and the respiratory tract. They usually have a predilection for the lungs, without any gender bias. However, the extrapulmonary IPTs occur slightly more commonly in females, predominantly in the abdomen, head and neck, and the central nervous system. In the abdomen, they tend to occur in the gastrointestinal tract, the urinary bladder and the retroperitoneum. Most of these lesions are discovered incidentally during the work up for other malignancies, after splenectomy, for conditions such as idiopathic thrombocytopaenic purpura [3], etc. or at autopsy. They are frequently misdiagnosed as malignant neoplasms, clinically and radiologically. Currently, only histopathological and immunohistochemical evaluations are able to confirm the diagnoses of IPTs reliably.
Case Report
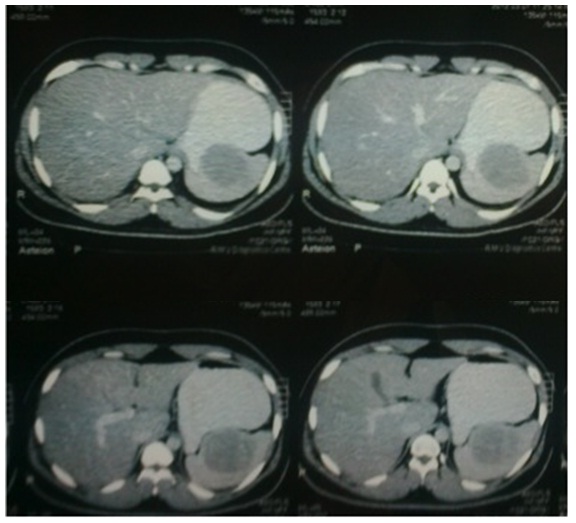
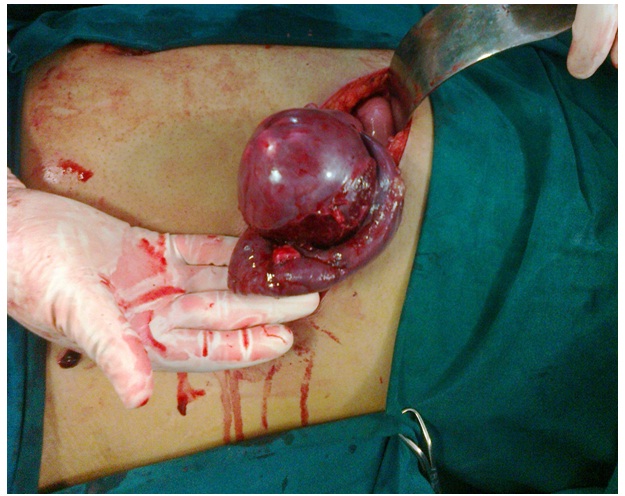
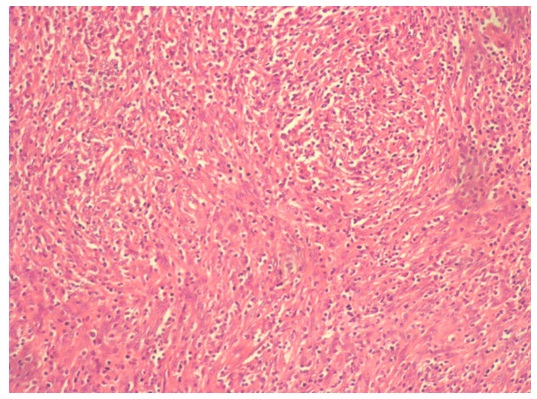
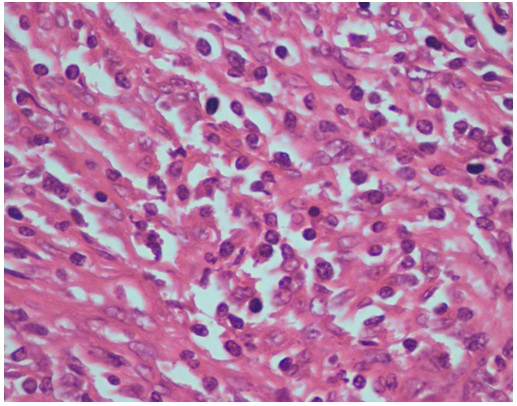
Our patient was a 24 years old male, who had pain in the abdomen and one episode of vomiting. The abdominal examination was unremarkable. While the blood investigations were within normal limits, an abdominal ultrasound showed the presence of a lobulated cystic lesion with thick echogenic contents and internal septations, which measured 6.5 x 6.6 x 5.5 cm, with a volume of 123 cc. On the CECT of the abdomen, [Table/Fig-1] a well-defined non-enhancing cystic lesion which measured 6.2 x 6.7 x 6.8 cm, with no enhancing solid components, was seen. The differential diagnosis according to the radiologists, at the time, included a splenic abscess, a hydatid cyst or a developmental cyst. The patient was advised a splenectomy, but he refused surgery for personal reasons. Six months later, he came to us on experiencing another episode of pain in the abdomen. A repeat ultrasound abdomen indicated mild splenomegaly, with a fairly large, complex cystic lesion in the splenic parenchyma, which measured 8.2 x 7.1 cm, with medium to high internal echoes and thin septations within it. A ruptured hydatid cyst or a splenic cyst with organized haemorrhage was suspected. The patient then underwent splenectomy without any complications. The removed spleen with the lesion in situ [Table/Fig-2], was sent for a histopathological examination and immunohistochemistry. On gross examination, a solid mass was seen within the spleen, which measured 9 x 7 x 3.5 cm. The cut surface of the mass showed circumscribed, grey white solid tissue with areas of haemorrhage and a whorled appearance. Microscopically [Tables/Figures 3a and 3b] the sections of the lesion comprised spindle cells, along with elongated nuclei and a moderate amount of eosinophilic cytoplasm. Interspersed amongst these, were lymphocytes and plasma cells. The adjacent splenic tissue which comprised red and white pulp, was compressed by the splenic-tumour. No atypia or a significant mitotic activity were seen. On immunohistochemistry, the spindle cells were found to be positive for SMA, CK and LMP 1 (Latent Membrane Protein 1 for Epstein Barr Virus) and negative for Alk, desmin, CD117, S100, CD 21 and CD 23. The AFB staining was negative. The above findings were in favour of an Inflammatory Pseudotumour.
CECT abdomen (plain and contrast) showing a well definedhypodense lesion in the spleen measuring 6.2 x 6.7 x 6.8cm
Per-operative photo of spleen with tumour in situ after splenectomy
H&E 100x magnification view of specimen slides showing an admixture of inflammatory cells within a stroma of spindle cells
H&E 400x magnification view of specimen slides showing an admixture of inflammatory cells within a stroma of spindle cells
Discussion
Inflammatory Pseudotumours are rare, circumscribed lesions of unknown aetiology, which may be symptomatic or asymptomatic. Cotelingam and Jaffe [2] characterized these lesions as a spectrum of non-neoplastic, inflammatory and reparative changes. The biological behaviour of IPT is controversial. Meis and Enzinger [4] documented the locally aggressive and the recurrent nature of these neoplasms and suggested that they were potentially malignant neoplasms. Meanwhile, Coffin et al., [5] described these lesions as benign, non-metastasising proliferations of myofibroblasts, with a potential for recurrence and a persistent local growth, which were similar to fibromatosis. Currently, the World Health Organization classification of soft tissue tumours places Inflammatory Pseudotumours in an intermediate category (Rarely metastasising, < 5 per cent), between benign and malignant [6].
Most of the theories on the origin of these tumours reflect an inflammatory process which is related to the overproduction of mediators such as IL-1β and IL- 6 [7], trauma, radiotherapy, steroids and surgery. Vascular, autoimmune and infective causes such as the Epstein Barr Virus, the Human Herpes Virus 8 and the Human Immunodeficiency Virus (HIV) have all been postulated, but they remain yet to be fully proven aetiologies [8]. Thomas S Neuhauser et al., [9] demonstrated EBV by immunohistochemical and in situ hybridisation studies. Clinically, the patients with IPTs of the spleen may be symptomatic or asymptomatic. The symptomatic patients may present with vague non-specific symptoms such as fever, weight loss, anaemia, malaise and abdominal discomfort. Pain in the left upper quadrant or in the epigastric region is the most common symptom. IPTs of the spleen have been detected almost exclusively in adults (4–87 years) and median age (49 years) [10] with a slight female preponderance (56.5 per cent) [11].
Most of the blood parameters tend to remain within the normal range, but abnormalities such as the elevation of CRP and ESR, as well as an increase, sometimes in the WBC count, reflects the inflammatory characteristics of the tumour [12]. In our patient, the laboratory investigations were by and large normal. A variety of imaging techniques have been used for their detection. The splenic mass is most often described as a lesion of low density on computed tomography, as hypoechoic on ultrasonography and as either hypovascular or avascular following angiography [10]. Surprisingly, in our patient, ultrasound of the abdomen was indicative of a lobulated cystic lesion of the spleen. The CECT abdomen scan of our patient showed a well defined, non-enhancing lobulated cyst in the upper pole of the spleen, which suggested that the lesion could be a thin walled abscess or a hydatid cyst. A repeat ultrasound of the abdomen which was done six months later, further confirmed this. It was decided to therefore go in for a splenectomy. A splenectomy is both diagnostic and curative and it results in an excellent prognosis [11].
Histologically, they are composed of acute and chronic inflammatory cells, predominantly plasma cells and lymphocytes, along with neutrophils, histiocytes and rarely eosinophils, in a stroma of mesenchymal fibroblastic spindle cells. The histopathological examination of the specimen was reported as an Inflammatory Pseudotumour of the spleen and this was further confirmed by an immunohistochemical positivity for SMA, CK and LMP 1 and a negativity for Alk. The following differential diagnoses were considered:
Inflammatory Myofibroblastic Tumour (IMT), which is Alk positive and EBV negative was ruled out. These tumours were often considered to be synonymous with IPTs by various authors [4, 5, 6, 9, 10]. However, Kutok et al., [13], Neuhauser et al., [9] and the Stanford Surgical Pathology Criteria [14] have described the two as distinct entities [9,13,14].
Follicular Dendritic Cell tumour (FDC) has a similar micro-scopic appearance, with minimal to moderate atypia of the spindle cells. These atypical cells are positive for the FDC markers like CD 21, CD 23 and CD 35. In the present case, CD 21 and CD 23 were negative [8].
Mycobacterial spindle cell pseudotumour is a spindle cell tumour which is usually associated with the Mycobacterium Avium Intercellulare infections and AIDS. The cytoplasm of these spindle cells stain strongly for AFB [15]. Our case was negative for AFB. The primary benign tumours of the spleen account for only 0.007 per cent of all operation and autopsy findings. The diagnostic dilemmas which we faced were on multiple fronts. The non-specific symptoms, along with the unusual location of the lesion, did not lead us to suspect an IPT of the spleen. Also, the imaging reports misled us towards a parasitic infestation, i.e., hydatid cyst. Ultimately, this diagnosis of a possibly ruptured splenic hydatid cyst prompted the splenectomy, which established the diagnosis of this rare entity. At present, neither modern imaging techniques, such as ultrasonography, CT, MRI nor FNAC, allow for a preoperative diagnosis of an inflammatory pseudotumour [16]. Differential diagnoses must be made with several diseases, such as abscesses, hemangiomas, angiosarcomas, malignant lymphomas and haematomas [16].
Inflammatory Pseudotumours of the spleen generally undergo non-aggressive clinical courses without local recurrences or metastases, if the lesions are removed completely. Following splenectomy, the prognosis of IPTs is favourable, and there have been no reports of metastatic disease. However, there have been reports of some patients with IPTs of the liver, who have died as a result of the progression of the disease [17]. At six months post-operatively, our patient was asymptomatic and a repeat ultrasonogram of the abdomen and the pelvis was a normal study, with no signs of recurrence.
Conclusion
An IPT of the spleen is an uncommon lesion which is not associated with specific clinical or radiological findings and hence, it is mistaken for a splenic neoplasm. Hence, no adequate preoperative diagnostic modality exists and a majority of the cases are detected incidentally after splenectomies and after the ensuing histopathological examinations and the immunohistochemistry. Though a recurrence and metastasis is unheard of, these patients must be followed up carefully, as IPTs are considered to be tumours with intermediate malignant potential.
[1]. Moriyama S, Inayoshi A, Kurano R, Inflammatory pseudotumor of the spleen: report of a caseSurg Today 2000 30:942-46. [Google Scholar]
[2]. Cotelingam JD, Jaffe ES, Inflammatory pseudotumor of the spleenAm J Surg Pathol 1984 8:375-80. [Google Scholar]
[3]. Hatsuse M, Murakami S, Haruyama H, Inaba T, Shimazaki C, Inflammatory pseudotumor of the spleen complicated by idiopathic thrombocytopenic purpuraAnn Hematol 2005 84:619-20. [Google Scholar]
[4]. Meis JM, Enzinger FM, Inflammatory fibrosarcoma of the mesenteryand retroperitoneum. A tumor closely simulating inflammatorypseudotumorAm J Surg Pathol 1991 15:1146-56. [Google Scholar]
[5]. Coffin CM, Watterson J, Priest JR, Dehner L, Extrapulmonaryinflammatory myofibroblastic tumor (inflammatory pseudotumor). A clinicopathologic and immunohistochemical study of 84 casesAm J Surg Pathol 1995 19:859-72. [Google Scholar]
[6]. Coffin CM, Humphrey PA, Dehner LP, Extrapulmonary inflammatory myofibroblastic tumor: a clinical and pathological surveySemin Diagn Pathol 1998 15:85-101. [Google Scholar]
[7]. Rohrlich P, Peuchmaur M, de Napoli Cocci S, Interleukin-6 and interleukin-1B production in a pediatric plasma cell granuloma of the lungAm J Surg Pathol 1995 19:590-95. [Google Scholar]
[8]. Lewis JT, Gaffney RL, Casney MB, Farrel MA, Morice WG, Macon WR, Inflammatory pseudo-tumor of the spleen associated with a clonal Epstein-Barr virus genome: Case report and review of literatureAm J Clin Pathol 2003 120:56-61. [Google Scholar]
[9]. Neuhauser TS, Derringer GA, Thompson LDR, Splenic Inflammatory Myofibroblastic Tumor (Inflammatory Pseudotumor) A Clinicopathologic and Immunophenotypic Study of 12 CasesArch Pathol Lab Med 2001 125:379-85. [Google Scholar]
[10]. Oshiro H, Nomura M, Yamanaka S, Splenic inflammatory Pseudotumor (Inflammatory Myofibroblastic Tumor)J Clin Exp Hematopathol 2007 47:83-88. [Google Scholar]
[11]. Shapiro AJ, Adams ED, Inflammatory pseudotumor of the spleenmanaged laparoscopically. Can preoperative imaging establish thediagnosis? Case report and literature reviewSurg Laparosc Endosc Percutan Tech 2006 16:357-61. [Google Scholar]
[12]. Pankaj PD, Wenle PW, Kamal SP, “Inflammatory myofibroblastic tumor of epididymis: a case report and review of literature,”World J Surg Oncol 2008 6:119 [Google Scholar]
[13]. Kutok JL, Pinkus GS, Dorfman DM, Fletcher CD, Inflammatory pseudotumor of lymph node and spleen: an entity biologically distinct from inflammatory myofibroblastic tumorHum Pathol 2001 32:1382-87. [Google Scholar]
[14]. Kempson RL, Rouse RV, 2008 Stanford School of Medicine Surgical Pathology Criteria: Inflammatory Myofibroblastic Tumor [Internet]. [updated 15 Jun, 2008; cited in 15 May, 2008] Available from:http://surgpathcriteria.stanford.edu/softfib/inflammatory_myofibroblastic_tumor/printable.html [Google Scholar]
[15]. Suster S, Moran CA, Blanco M, Mycobacterial spindle-cell pseudotumor of the spleenAm J Clin Pathol 1994 101:539-42. [Google Scholar]
[16]. Hsu CW, Lin CH, Yang TL, Splenic Inflammatory Pseudotumor mimicking angiosarcomaWorld J Gastroenterol 2008 14(41):6421-24. [Google Scholar]
[17]. Horiuchi R, Uchida T, Kojima T, Shikata T, Inflammatory pseudotumor of the liver: clinicopathologic study and review of literatureCancer 1990 65:1583-90. [Google Scholar]