The Dengue infection is the most rapidly spreading mosquito-borne viral disease in the world and an estimated 50 million dengue infections are reported annually [1]. The case fatality rates for the south-east Asian region are 1%, but in India, Indonesia and Myanmar, focal outbreaks have reported rates of 3-5% [1]. The pathogenesis of thrombocytopaenia in Dengue Fever (DF) has not been clearly understood. The increased peripheral destruction of the antibody coated platelets has been strongly suspected as the possible mechanism. The other modes include acute bone marrow suppression which leads to a megakaryocytic condition and enhanced platelet destruction by the reticuloendothelial system [2, 3].
Thrombocytopaenia is a constant manifestation in dengue fever, which often leads to life threatening Dengue Haemorrhagic Fever (DHF) and the Dengue Shock Syndrome (DSS). Both haemorrhagic diathesis and circulatory collapse are the fatal complications of the dengue infection [4,5]. Thrombocytopaenia and bleeding tendencies are the common problems in dengue, which cause concern for the patients and the treating doctors [6].
Global attempts have been made to develop new treatment strategies to combat these fatal complications of the dengue infection [7]. Steroids are used in the treatment of idiopathic thrombocytopaenic purpura to increase the platelet count, which is mediated by auto antibodies. This hypothesis would support the use of steroids in dengue fever [8].
There are limited studies in the literature which have assessed the benefits and the risk of the corticosteroid therapy in the thrombocytopaenia in the dengue infection. Various steroid regimens have been used and some of them have shown beneficial effects and some have shown no benefits. However, the Cochrane reviews have concluded that there is insufficient evidence on the use of steroids in DSS and DHF and they have advised large randomized trials [7]. Kularathnesam et al., conducted a survey to take the opinions of physicians and paediatricians on the management of the dengue infection in Sri Lanka. It revealed that the World Health Organisation (WHO) guidelines were followed by only 16(45%) physicians and 6(40%) paediatricians in the management of DF and DHF and that steroids were used empirically in anticipation of bleeding diathesis [5]. Rajapakshe et al concluded in his study, that the possible effects of steroids on thrombocytopaenia and bleeding in dengue fever were unknown, even though they were used empirically [9].
A study which was done by Kularathne Sam et al., to evaluate the effect of low dose dexamethasone (Inj dexamethasone 4mg initially followed by 2mg IV q8h for 4 days) in dengue fever with thrombocytopaenia on platelet count, concluded that there was no benefit with low dose dexamethasone and they advised on conducting studies with high dose dexamethasone [10]. This prompted us to conduct the similar study with high dose dexamethasone.
The objective of this study was to test the efficacy of intravenous high dose dexamethasone (Inj dexamethasone 8mg initially followed by 4mg IV q8h for 4 days) on the mean platelet count in the acute stage of dengue fever with thrombocytopaenia [11].
Material and Methods
This study was carried out in the medical wards in JSS Medical College Hospital, Mysore, Karnataka, India, a tertiary medical care centre, from June 2010 to June 2011. At admission, all the suspected patients with dengue fever, who were above 18 years of age were assessed by the consultant (chief investigator). A detailed history was elicited and a thorough clinical examination was done. The data was collected in a prewritten proforma. The patients were screened for Dengue NS1Ag, IgG ELISA, IgM ELISA, Quantitative Buffy Coat for the malaria parasite, the serology for enteric fever, scrub typhus, leptospirosis,Haemoglobin, Total leukocyte count, Differential leukocyte count, Platelet count, Haematocrit, Peripheral Blood smear and LFT, were done in all patients. The chest radiographs were taken whenever indicated. Only the serologically confirmed cases of dengue IgM ELISA were included, when their platelet counts dropped below 50000/cumm during the acute stage of the illness. The conditions which cause thrombocytopaenia like HIV, Autoimmune Diseases, Connective Tissue disorders and Vasculities, ITP, Malignancy were excluded by thorough clinical examination and relevant investigations whenever it was indicated. The patients with Diabetes mellitus, Hypertension, a history of peptic ulcer disease or hypersensitivity to corticosteroids and total leukocyte counts of more than 11000/cumm were excluded from the study.
The patients with an evidence of bleeding or shock were excluded before their enrolment and randomization, as they needed a close management and treatments such as platelet transfusions, which would have compounding effects on the study outcome. A prior approval was obtained from the Ethical Committee of the JSS Medical college Hospital, Mysore and informed consents were obtained from the study participants. The sample size was calculated according to the Formula N=Z2pq/d2 with a 4% prevalence. (Z-standard value, d - margin of error, p is proportion of prevalence, q = 1-p).
For the purpose of the study, dengue fever was suspected and screened in 128 patients. After the exclusion of 67 patients, the remaining 61 patients who were positive for IgM ELISA for dengue were included in the study. They were allotted randomly, 30 into the study group and 31 into the control group, by blocked randomization by using a fixed blocking method, into the open labeled study. The block size was 6 and the allocation ratio was 1:1, which would lead to a random assignment of 3 subjects to the study group and 3 to the control group. The study group received intravenous dexamethasone 8mg initially, followed by 4 mg every 8 hrs, thereafter for 4 days and IV fluids were given whenever they were required. The control Group received only IV fluids and antipyretics whenever necessary. Daily monitoring of the platelet count, temperature, pulse, BP, weight, fluid intake output chart, oedema, haematocrit value, blood glucose and electrolytes was done for four days of the study period.
The mean rise in the platelet count was measured daily in both the groups, which was taken as the primary outcome. The statistical analysis was carried out by SPSS, version 16 and then the baseline variables (Hb%, age, sex, haematocrit, and the days of illness during the enrollment) were compared between the study and the control groups to ensure a correct and a comparable allocation. The differences in the continuous data (mean platelet count) were compared by using the independent sample “t” test. The trends of change in the platelet counts between the study and the control groups according to the days, were calculated by using the repeated measure (ANOVA) test.
Results
The demographic and the haematological features of both the groups were comparable, as shown in [Table/Fig-1]. There were no significant differences in the base line characters like the mean (SD) age, sex, the mean duration of the illness during the enrolment, Hb%, haematocrit, and the platelets in the both groups at the time of the enrolment. The mean rise in the platelet counts over four days, which was calculated by the independent sample “t” test in the both groups, is shown in [Table/Fig-2].
Demographic and haematological features of the sample selected for study and control group
| Characteristics | Study Group No. & SD | Control Group No. & SD | p value |
|---|
| Gender | Male | 16 (53.3) | 21 (67.7) | 0.249 |
| Female | 14 (46.7) | 10 (32.3) | |
| Age | Mean age (SD) years | 31.27 (12.86) | 32.71 (12.66) | 0.661 |
| Illness | Mean (SD) days illness at enrolment | 6.13 (2.36) | 6.35 (2.05) | 0.697 |
| Haemoglobin | Mean (SD) haemoglobin (g/dl) | 13.93 (2.27) | 13.45 (2.74) | 0.45 |
| Hematocrit | Hematocrit | 40.67 (5.57) | 39.57 (7.72) | 0.529 |
| Total no in a group | 30 | 31 | |
Mean platelet counts of control and study group over days and results of independent sample “t” test
| No. Control (31) Study (30) | Mean platelet count (in thousands) | Std. Deviation (in thousands) | t value | p value |
|---|
| Day 1 | 31 | 32225.8 | 12049.0 | 0.687 | 0.495 |
| 30 | 29913.3 | 14194.8 |
| Day 2 | 31 | 56683.8 | 23771.5 | 2.168 | 0.34 |
| 30 | 44200.0 | 21073.5 |
| Day 3 | 31 | 78483.8 | 35037.0 | 0.530 | 0.598 |
| 30 | 74066.6 | 29677.5 |
| Day 4 | 31 | 125612.9 | 41033.8 | 0.844 | 0.402 |
| 30 | 116433.3 | 43885.1 |
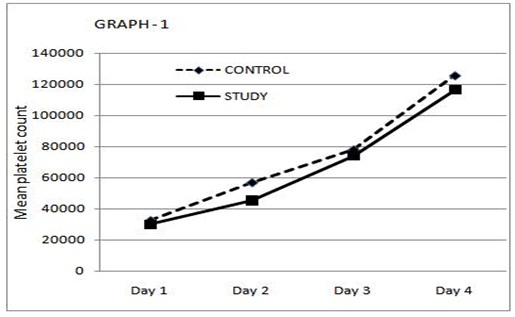
The repeated measure ANOVA statistics further showed increasing trends of the mean platelet counts in both the study group and the control group during the study period of four days. There was a rise in the platelet counts in both the study and the control groups; the rise in the mean platelet count being higher amongst the control group. However, it was statistically not significant. The estimated marginal means of the platelet count, as shown in the [Table/Fig-3], did not show any significant difference between the study and the control groups. There was no significant difference in the weight, oedema, haematocrit value, blood glucose, and the electrolyte levels among the groups for four days of the study period. The hospital stay was the same, without any mortality among the groups and none of them developed shock or required Transfusions or admitted to intensive care during the study period of four days.
Estimated marginal means of mean platelet count in study and control group
Discussion
The Dengue infection results in significant morbidity and mortality worldwide. The current recommended treatment is largely supportive, with careful fluid replacement and with no specific treatment being available at present [5]. The common goal in treating these patients with severe thrombocytopaenia is to stabilize the platelet count, which will prevent the major risk of bleeding [12]. Corticosteroids are potent anti-inflammatory agents that have a wide range of effects on the immunological processes. Although corticosteroids are not mentioned in the WHO guidelines on the management of dengue, clinicians use corticosteroids empirically, based on the presumed immunological basis of the complications of dengue, particularly in the south east Asian countries [5]. They are thought to be effective for stabilizing the capillary permeability and have been used in addition to the fluid replacement [5].
The study of Aneja R et al., showed that there was a cortisol insufficiency in the children with DHF and DSS [13]. Most of the studies which are related to the effect of steroids on dengue, have been done on children with DHF and DSS but only limited studies have been done on adults. The evidence for the benefit or a lack of benefit of corticosteroids on thrombocytopaenia and bleeding, as well as the other complications of dengue, are not clear [7]. The Cochrane Database of Systematic Reviews, 2006, concluded that there was insufficient evidence to justify the use of corticosteroids in DHF and DSS and it concluded the need for large randomized controlled trials [7]. In dengue fever, various steroid regimens have been used and some of them have shown beneficial effects [14] and some have not shown benefits [15–18].
Three trials compared intravenous hydrocortisone hemisuccinate with no corticosteroids or placebo [7,14,15] and one compared methyl prednisolone with placebo [16]. Futrakul et al., showed a positive response with a high dose of methyl prednisolone with mannitol in severe DSS which was unresponsive to fluid replacement [18]. In spite of these uncertainties, steroids are still used in the dengue infection by the local clinicians in Srilanka [5].
Panpanich R et al., observed an increased mortality after the use of steroids in DSS and DHF and opined that it was difficult to conduct a study on life threatening illnesses like DSS and DHF, as steroids would have compounding effects on the outcome of the disease [7]. Therefore in our study we included only the patients with dengue fever with thrombocytopaenia, without bleeding diathesis or the shock syndrome.
Sam Kularathne et al., used low dose dexamethasone ie 4mg initially, followed by 2mg q 8 hours for 4 days in dengue fever with thrombocytopaenia (platelets less than 50000/cumm) in a placebo controlled study and concluded that it was not effective in increasing the platelet count. They advised to conduct similar studies using high dose dexamehasone [10]. In our study, we used a high dose of dexamethasone ie 8mg initially, followed by 4mg IV q8hrs for 4 days, but there was no difference in the rise in the mean platelet counts in both the groups. In fact, the control group showed a higher rise in the mean platelet counts on all the 4 days of the study period as compared to the study group. In our study, a gradual rise in the platelet count was observed over four days in both the groups, which was in concordance with the natural history of the recovery of the platelet count in the dengue infection. A similar observation of the recovery of the platelet count after a maximum drop, with increasing platelet counts gradually over three days without any intervention, was observed in a Srilankan study [5].
The possible risk of the worsening of the dengue illness because of increased viral replication, due to the immunosuppressive property of corticosteroids, was raised in the study which was done by Sam Kularathne and his colleagues [10].
In both the groups of our study, there were no drop outs and all the patients improved without worsening of the clinical condition or mortality. This ruled out the possible risk of worsening of the illness due to the high dose short course steroids in our study, because of the strict adherence to the exclusion of the patients with dengue fever with an intercurrent infection. Several studies have shown that the empirical use of steroids in sepsis is still controversial [19–24]. The use of steroids, without excluding the intercurrent infection in dengue fever, may worsen the illness, leading to increased morbidity and mortality due to its immunosuppressive effect [25–29].
In view of these observations, the empirical use of steroids may be avoided in dengue fever with thrombocytopaenia. Our study demonstrated that high dose dexamethasone lacks efficacy in increasing the platelet count in thrombocytopaenic dengue patients. The rise in the mean platelet count (the primary outcome) remained similar in both the control and the study group. So, the results of our study are in concordance with the conclusions which were opined by the Cochrane review [7].
However, the lowest level of platelet count in dengue fever without bleeding is still controversial. This was supported in our study, where bleeding was not seen in three patients with platelet counts of less than 5000/cumm. The drawback of our study was, it was not a double blind placebo controlled trial and there were less number of subjects and cases of DHF and DSS were not included.
Therefore, dengue fever with thrombocytopaenia without bleeding diathesis can be managed with supportive therapy, as has been mentioned in the WHO guidelines. We conclude that a high dose, a short course of the dexamethasone therapy is ineffective in increasing the platelet count.