Purpose:Staphylococcus aureus has developed resistance against most of the therapeutic agents. The most notable example of this phenomenon was the emergence of Methicillin resistant Staphylococcus aureus (MRSA). We are reporting the prevalence and the antibiotic susceptibility pattern of the MRSA isolates from a tertiary care hospital.
Methods: A total of 450 Staphylococcus aureus isolates from clinical samples were taken up for the study and they were screened for MRSA by using standard microbiological methods. An antibiotic assay was done for the confirmed MRSA isolates. The differentiation of the isolates into community acquired MRSA (CAMRSA) and hospital acquired MRSA (HAMRSA) was done according to the prescribed criteria. The double disc diffusion test was performed for both the groups, to identify the inducible clindamycin resistance. The HAMRSA and the CAMRSA isolates were subjected to a molecular analysis by PCR, to detect the presence of the Mec A gene and the PVL gene respectively.
Results: Out of the 450 Staphylococcus aureus isolates, 121 were Methicillin Resistant Staphylococcus aureus (MRSA, 27%) and 329 were Methicillin Sensitive Staphylococcus aureus (MSSA, 73%). 91 MRSA isolates were grouped into HAMRSA and 30 were grouped into CAMRSA, with a prevalence of 20% and 7% respectively. All the MRSA strains were resistant to Penicillin (100%), Cefoxitin (100%) and Oxacillin (100%). 53.7% of the HAMRSA isolates showed inducible clindamycin resistance against that of 44.4% among the CAMRSA isolates. All the isolates were susceptible to Vancomycin and Linezolid. 64% of the HAMRSA isolates showed the presence of the Mec A gene and 48% of the CAMRSA isolates showed the presence of the PVL genes.
Conclusion: The prevalence of the HAMRSA was higher than that of the CAMRSA and they showed a higher drug resistance.
Methicillin resistant Staphylococcus aureus, Community acquired MRSA, Hospital acquired MRSA
Introduction
The ubiquity of the gram positive bacteria in nature makes the interpretation of their recovery from patient specimens occasionally difficult, unless the clinical manifestations of an infectious disease are apparent. The recovery of these organisms from specimens should always be correlated with the clinical conditions of the patients, before their role in the infectious process can be established [1]. Staphylococcus aureus is the most important human pathogen among the Staphylococci. It is found in the external environment and in the anterior nares of 20-40% of the adults. The other sites of its colonization include the intertriginous skin folds, the perineum, the axillae, and the vagina [2].
Staphylococcus aureus is a versatile human pathogen which causes infections which range from a relatively mild involvement of the skin and the soft tissue, to life – threatening sepsis and pneumonia, and the toxic shock syndrome [2]. This organism causes illness through the production of numerous cell surfaces and secreted virulence factors, and the disease is facilitated by its propensity to develop resistance to multiple antibiotics. Infections in the community and hospital settings are common [1,3,4].
Originally, penicillin was the drug of choice for the Staphylococcus aureus infections. Most of the penicillin-resistant strains of Staphylococcus aureus produce β- lactamase, which hydrolyzes the β-lactam ring of the antibiotic. The resistance to methicillin and other β-lactamase resistant penicillins was first observed in Staphylococcus aureus, soon after methicillin was introduced into the clinical use in 1961 [3]. The first case of an MRSA infection recorded in Australia, was in Sydney in 1965 [5,6]. The first case of a community – associated MRSA (CAMRSA) infection in the United States was reported in 1980.
The HA-MRSA isolates do circulate in the community, especially among adults. Additionally, many reports have demonstrated that the MRSA clones bear SCCmec type IV.
The CA-MRSA strains are genetically and phenotypically distinct from the HA-MRSA. They typically resemble some strains of methicillin-susceptible S. aureus (MSSA), in being susceptible to a wider range of anti-staphylococcal antibiotics (some are resistant only to β-lactams), and they often produce PVL, a toxin that destroys the white blood cells and is a staphylococcal virulence factor [7,1].
Many of the MRSA isolates are becoming multidrug resistant and they are susceptible only to the glycopeptide antibiotics such as vancomycin. A low level resistance, even to vancomycin, is emerging. A prolonged hospital stay, the indiscriminate use of antibiotics before hospitalisation, etc. are the common factors of the MRSA infections which occur globally. These affected patients act as the root cause for the spread of the infections to the hospital staff and they can act as carriers, adding more complications to the treatment.
Material and Methods
This study was carried out in the Department of Microbiology, in a tertiary care hospital which was situated on the outskirts of Chennai, India. The study material consisted of 450 non-repetitive isolates of Staphylococcus aureus which were obtained from the clinical samples of the inpatients and the outpatients who were treated in various clinical departments. The comprehensive particulars of the patients were meticulously noted before the samples were collected. The patient particulars, the presenting complaints, previous history of hospitalisation or surgeries under went were noted. The Staphylococcus aureus isolates were subjected to an antibiotic sensitivity testing by the Kirby Bauer disk diffusion method. Penicillin, ampicillin, azithromycin (15μg), cefoxitin (30μg), cefotaxime (30μg), chloramphenicol (30μg), clindamycin (2μg), erythromycin (15μg), oxacillin (1μg), vancomycin (30μg), teicoplanin (30μg)), ciprofloxacin, ofloxacin (5μg), linezolid (30μg) and tetracycline (30μg) were used to study the susceptibility patterns of the isolates.
Detection of MRSA
A phenotypic test for the detection of the MRSA was done by using a cefoxitin (30 μg) disc. A zone of inhibition which was equal to or more than 22 mm was considered as susceptible to Cefoxitin and the Staphylococcus aureus isolate produced it was reported as Methicillin Sensitive Staphylococcus aureus and those isolates which produced a zone of inhibition which was less than or equal to 21 mm were considered as Methicillin Resistant Staphylococcus aureus [8].
The MRSA isolates were classified into Community Acquired or Hospital acquired, based on the history of the patient [9]. A simpler, temporal definition is often used to designate the CAMRSA. Based on this criterion, all infections occurring among the out patients or inpatients with an MRSA isolate earlier than 48 hours of hospitalisation, would be considered as CAMRSA. The Community acquired MRSA occurs in individuals in the community, who are generally healthy and who were not receiving healthcare in a hospital or on an ongoing outpatient basis. The HA-MRSA refers to the hospital or healthcare acquired methicillin resistant Staphylococcus aureus. Any MRSA which was isolated from a patient after 48 hours of hospitalisation or from a patient with a history of hospitalisation for surgery or dialysis, or of a residence in a long term care facility within 1 year of the MRSA culture date.
Inducible Clindamycin Resistance
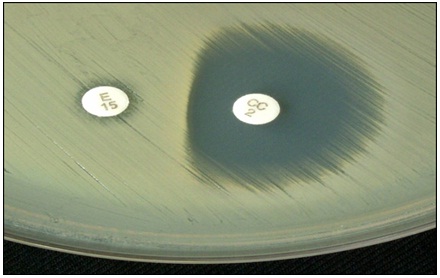
The erythromycin resistant isolates of MRSA were tested for inducible clindamycin resistance by doing the ‘D’ test. It was detected by the double disk test, by placing a 2 μg clindamycin disk, 15 mm away from the edge of a 15 μg erythromycin disk on a Muller Hinton agar plate, in which a lawn culture of the organism was made. The plate was incubated at 37°C. Flattening of the zone around the clindamycin disc towards the erythromycin disc was considered as inducible clindamycin resistance (D test) positive [8]. This denoted that the D test positive isolates were resistant to clindamycin in-vivo [Table/Fig-1].
Inducible clindamycin resistance (D test positive)
Genomic Analysis
The genomic analysis was done according to the standard protocols by extracting the DNA by using Phenol-Chloroform extraction procedures and subjecting it to a PCR analysis [5,9].
The primer sequence for mec A gene is as follows:
A 30 nucleotide forward primer:
5’- AAT CTT TGT CGG TAC ACG ATATTC TTC ACG -3’
A 30 nucleotide reverse primer:
5’-CGT AATGAG ATT TCA GTA GAT AAT ACA ACA -3’
The primer sequence for PVL A gene is as follows:
luk-PV-1, 5’ – ATCATTAGGTAAAATGTCTGGACATGATCCA-3’
luk-PV-2, 5’ – GCATCAASTGTATTGGATAGCAAAAGC-3’.
Results
A total of 450 non-repetitive Staphylococcus aureus isolates were selected for the study. Among them, 121 (27%) were Methicillin Resistant Staphylococcus aureus and 329 (73%) were Methicillin Sensitive Staphylococcus aureus (MSSA,). The prevalence of MRSA in our hospital was found to be 27% [Table/Fig-2].The MRSA isolates were classified into HAMRSA snd CAMRSA, based on the clinical history. 91 MRSA isolates were grouped into HAMRSA and 30 were grouped into CAMRSA, with a prevalence of 20% and 7% respectively. The highest number of positive MRSA isolates were obtained from exudates (91%), followed by blood (5%), urine (2%), and respiratory (2%) specimens [Table/Fig-3]. More number of MRSA cases were reported from surgical wards (52%), followed by medical wards (26%), gynaecology wards (8%), ICUs (7%), paediatric wards (4%) and other wards (3%).
| Type | Number (n = 450) | Prevalence (%) |
|---|
| MSSA | 329 | 73% |
| MRSA | 121 | 27% |
| HAMRSA | 91 | 75% |
| CAMRSA | 30 | 25% |
Distribution of MRSA from different clinical samples
| Clinical specimen | S. aureus (n = 450) | MRSA (n = 121) |
|---|
| Exudate | 284 | 110 (91%) |
| Blood | 76 | 6 (5%) |
| Urine | 55 | 3 (2%) |
| Respiratory specimens | 35 | 2 (2%) |
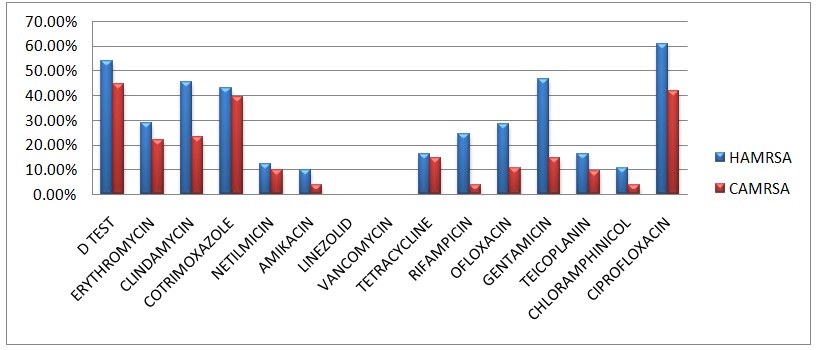
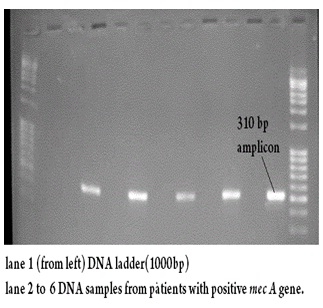
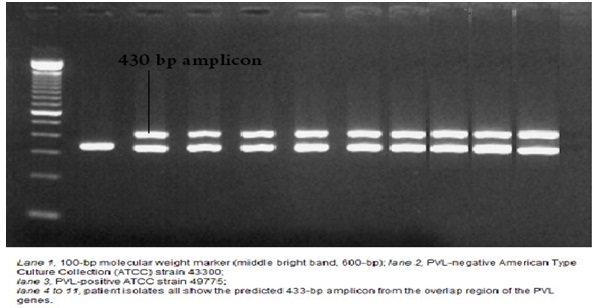
From this study, it was concluded that the active age groups were more susceptible to MRSA and its associated diseases. 48 HAMRSA (52.74%) and 13 CAMRSA (43.33%) isolates showed inducible clindamycin resistance, which was confirmed by the ‘D’ test. All the MRSA isolates were 100% susceptible to vancomycin and linezolid. Overall, the resistance patterns of the HAMRSA were (10 – 30%) higher as compared to those of the CAMRSA [Table/Fig-4]. The Mec A gene [Table/Fig-5] was isolated from 64% of the HAMRSA isolates and the PVL gene [Table/Fig-6] was isolated from 48% of the CAMRSA isolates.
Resistance pattern of HAMRSA and CAMRSA
Gel electrophoresis picture of Mec A gene from HAMRSA isolates Lane 1 (from left) DNA ladder (1000bp) Lane 2 to 6 DNA samples from patients with positive mec A gene
Gel electrophoresis picture of PVL gene from CAMRSA isolates Lane 1. 100-bp molecular weight marker (middle bright band. 600-bp). Lane 2. PVL-negative American Type Culture Collestion (ATCC) strain 43300: Lane 3. PVL-positive ATCC strain 49775: Lane 4 to 11, patient isolates all show the predicted 433-bp amplicon from the overlap region of the PVL
Discussion
In developing countries like ours, in spite of the strict aseptic precautions which are being followed, MRSA causes important nosocomial infections. The improper usage of antibiotics can be identified as the root cause of the present condition. Since drug resistance is common among Staphylococcus aureus, appropriate antibiotics should be chosen, based on the susceptibility pattern.
Methicillin-Resistant S. Aureus (MRSA) is a significant pathogen that has emerged over the past four decades, which causes both nosocomial and community-acquired infections. A rapid and an accurate detection of the methicillin resistance in S. aureus is important for the use of the appropriate antimicrobial therapy and for the control of the spread of the MRSA strains, because MRSA is an important nosocomial pathogen which causes significant morbidity and mortality.
One hundred and twenty one MRSA isolates were isolated from among a total of 450 Staphylococcus aureus isolates which were from various clinical samples. The prevalences of the MRSA isolates were as follows: 91% of the MRSA were obtained from exudates, 5% from blood and 2% from urine and respiratory samples. Similar results were reported by PD Fey et al., [5] and by Quresh A et al., [10].
The skin and the soft tissue was the most common site for the infection among all the subjects who were selected for the study, especially among the CAMRSA patients, and 80% of the cases had cutaneous infections. Besides the dermatological conditions, diabetes and chronic renal failures were the most common underlying diseases which were observed among the HAMRSA cases. These findings correlate with the findings of the studies which were done by Hsin Huang et al., [11].
From the statistical analysis, the prevalence of MRSA was calculated as 27%. Among these cases, 20% were HAMRSA cases and 7% were CAMRSA cases. Out of the 121 patients from whom MRSA was isolated, 91 had a previous history of a hospitalisation or surgery and they were classified as HAMRSA and 30 were not having any previous history or who did not satisfy the criteria to be included as HAMRSA, were classified in the group of CAMRSA. The studies which were done by Tacconelli E et al., [12] showed similar results.
The surgical wards (52%) provided the highest number positive MRSA isolates, followed by the medical wards (26%), the gynaecology wards (8%), the ICUs (7%) and the paediatrics wards (4% with the lowest numbers). Floriana Campanile et al., [13], conducted similar studies and reported that the highest numbers of MRSA were obtained from the ICUs (53%), followed by the medical wards (34%) and other wards, which did not correlate with the findings of our study.
The active age group (15 to 60 years) was more susceptible to these infections. Similar findings were reported by Jessica E West et al., [14]. The antibiogram showed the HAMRSA to have more resistance (10 – 30%) to various antibiotics as compared to the CAMRSA. This correlated with the results of Hsin Huang et al., [11]. The Mec A gene was isolated from 64% of the HAMRSA isolates and the PVL gene was isolated from 48% of the CAMRSA isolates.
This study also suggested that a majority of the MRSA isolates which were recovered at hospital admission, were acquired during a prior exposure to a healthcare setting. The presence of virulence genes in the MRSA (either the Mec A gene in the HAMRSA or the PVL gene in the CAMRSA) increases their ability to resist antibiotics through altered gene products. The involvement of carriers is another important factor which spreads the infections in hospitals. Proper hand washing procedures must be practised, to avoid the spread of the infection in healthcare settings
[1]. Peter Borriello S, Patrick Murray R, Hodder Arnold, Topley and Wilson’s Microbiology and Microbial infections Bacteriology 2005 10ASM press:769-70. [Google Scholar]
[2]. Collee JG, Franser AG, Marmion BP, Simmons A, Mackie and McCartney Medical Microbilogy. Chapter 6 1996 6Tata McGraw Hill Publications:380-88. [Google Scholar]
[3]. Diederen BML, van Leest, van Duijn I, Willemse P, van Keulen PHJ, Kluytmans JAJ, Performance of MRSA ID, A new chromogenic medium for detection of methicillin-resistant Staphylococcus aureusJ Clin Microbiol 2006 44:586-88. [Google Scholar]
[4]. Calfee DP, Durbin LJ, Germanson TP, Spread of methicillin resistant Staphylococcus aureus (MRSA) among household contacts of individuals with nosocomially acquired MRSAInfect Control Hosp Epidemiol 2006 24:422-26. [Google Scholar]
[5]. Fey PD, Saïd-Salim ME, Hinrichs SH, Boxrud DJ, David CC, Kreiswirth BN, Comparative molecular analysis of community or hospital acquired methicillin-resistant Staphylococcus aureusAntimicrob Agents Chemother 2003 47(1):196-203. [Google Scholar]
[6]. Fluit AC, Wielders CLC, Verhoef J, Schmitz FJ, Epidemiology and susceptibility of 3,051 Staphylococcus aureus isolates from 25 university hospitals participating in the European sentry studyJ Clin Microbiol 2001 39:3727-32. [Google Scholar]
[7]. Ellis MW, Griffit ME, Jorgensen JH, Hospenthal DR, Mende K, Patterson JE, Presence and molecular epidemiology of virulence factors in methicillin-resistant Staphylococcus aureus strains colonizing and infecting soldiersJ Clin Microbiol 2009 47:940-47. [Google Scholar]
[8]. CLSI guidelines for antimicrobial susceptibility testing, M100, S21, 2011 [Google Scholar]
[9]. ASM microlibrary (http://www.microbelibrary.org/library/laboratory-test/3656-polymerase-chain-reaction) [Google Scholar]
[10]. Qureshi A, Rafi HS, Qureshi SM, Ali AM, The current susceptibility patterns of methicillin resistant staphylococcus aureus to conventional anti staphylococcus antimicrobials at RawalpindiPak J Med Sci 2004 20(4):361-64. [Google Scholar]
[11]. Hsin Huang, Neil Flynn M, Jeff King H, Caroline Monchaud, Margaret Morita, Stuart Cohen H, Comparisons of Community Associated Methicillin Resistant Staphylococcus aureus (MRSA) and Hospital-Associated MSRA Infections in Sacramento, CaliforniaJ Clin Microbiol 2006 44(7):2423-27. [Google Scholar]
[12]. Tacconelli E, Venkataraman L, De Girolami PC, Agata D EM, Methicillin-resistant Staphylococcus aureus bacteraemia diagnosed at hospital admission: distinguishing between community-acquired versus healthcare-associated strainsJ Antimicrob Chemother 2004 53(3):474-79. [Google Scholar]
[13]. Campanile Floriana, Bongiorno Dafne, Borbone Sonia, Stefani Stefania, Hospital associated methicillin resistant Staphylococcus aureus (HA-MRSA) in ItalyAnnals of Clinical Microbiology and Antimicrobials 2009 8:22-28. [Google Scholar]
[14]. Karri Bauer A, Jessica West E, Joan Miquel, Balada Llasat, Pancholi Preeti, Stevenson Kurt B, Debra Goff A, An antimicrobial stewardship program’s impact with rapid polymerase chain reaction methicillin resistant Staphylococcus aureus/S. aureus blood culture test in patients with S. aureus bacteremiaClinical Infectious Diseases 2010 51(9):1074-80. [Google Scholar]