Alopecia, or hair loss, is a common and an often distressing problem. The physicians may find it difficult to make a specific diagnosis [1]. Primary alopecia of the scalp is commonly divided into two groups, namely scarring and non-scarring [2]. Scarring alopecia or Cicatricial alopecia results from a follicular damage which is sufficient to produce destruction and replacement of the pilosebaceous structures by the scar tissue [3]. It is an enigmatic group of hair disorders which is linked by the potential permanent loss of the scalp hair follicles in the involved areas [4].
Primary scarring alopecias represent a group of disorders which are characterized by replacement of the follicular structure by fibrous tissue, with consequent permanent alopecia [5]. The evaluation of the patients with cicatricial alopecia is particularly challenging, and dermatopathologists receive only little training in the interpretation of the scalp biopsy specimens. An accurate interpretation of the specimens from the patients with hair disease requires both qualitative (morphology of follicles, inflammation, fibrosis, etc.) and quantitative (size, number, follicular phase) information. Much of this data can only be obtained from transverse sections. In most of the cases, a good clinical/pathologic correlation is required, and so the clinicians are expected to provide demographic information as well as a brief description of the pattern of hair loss and a clinical differential diagnosis [6].
Material and Methods
This prospective study included 32 biopsy – proven cases of Scarring Alopecia, who had attended the dermatology clinic of our tertiary care hospital between January 2009 and May 2012.
Primary SA was defined as a disease in which the pathology centred around the pilosebaceous hair follicles and Secondary SA was defined as one in which the follicles were destroyed due to a disease of the same or a skin disease on the scalp, which was independent of the follicles.
Primary SA was classified according to the North American Hair Research Society.
The working classification of the North American Hair Research Society (NAHRS) [7].
Lymphocytic group (e.g., Discoid Lupus Erythematosus (DLE), Lichen Planopilaris (LPP), classic pseudopelade of Brocq, central centrifugal cicatricial alopecia)
Neutrophilic group (e.g., Folliculitis Decalvans (FD), dissecting cellulitis)
Mixed group (e.g., folliculitis keloidalis)
Non – specific SA
The SPSS, version 14 software was used to analyse the data. Frequencies and percentages were used to describe the data.
Results
During the study period, 32 cases of scarring alopecia (SA) were diagnosed, of which 24 were primary SA and 8 were secondary SA. Most of the cases were seen in the third and fourth decades of life, with a male preponderence [Table/Fig-1].
Showing Age and Sex distribution
| Age (years) | Male | Female | Total | Percentage |
|---|
| 1-10 | 00 | 01 | 01 | 3.12 |
| 11-20 | 03 | 00 | 03 | 9.37 |
| 21-30 | 08 | 05 | 13 | 40.62 |
| 31-40 | 06 | 06 | 12 | 37.50 |
| 41-50 | 00 | 01 | 01 | 3.12 |
| 51-60 | 01 | 01 | 02 | 6.25 |
| Total | 18 | 14 | 32 | 100 |
Among the Primary SA, lupus erythematosus constituted 19 cases, lichen planopilaris constituted 3 cases and folliculitis decalvans and non specific SA constituted one case each. In secondary alopecia, there were 4 cases of morphea and one each case of lupus vulgaris, congenital absence of skin, burn and sarcoidosis [Table/Fig-2].
Showing incidence of various lesions with comparison with other studies
| Moure et al., [7] | Oremovic et al., [8] | Present study |
|---|
| Lupus erythematosus | 44.73% | 75% | 79.16% |
| Lichen planopilaris | 10.42% | 2.77% | 12.5% |
| Folliculitis decalvans | 7.89% | 2.77% | 4.16% |
Primary SA was classified, based on the inflammatory infiltrate, according to the North American Hair Research Society’s (NAHRS’) classification. Primary SA which showed a lymphocytic infiltration was seen in 23 cases, among which lupus erythematosus was seen in 19 cases, lichen planopilaris was seen in 3 cases and non specific SA was seen in 1 case. A neutrophilic inflammatory infiltrate was seen in only one case i.e., folliculitis decalvans [Table/Fig-3].
Classification of Primary SA based on inflammatory cell infiltrate based on North American Hair Research Society
| Primary SA – 24 |
|---|
| Type of Inflammatory cell | Disease |
|---|
| Lymphocytes – 23 | Lupus erythematosus - 19 |
| Lichen planopilaris – 03 |
| Non – specific scarring alopecia – 01 |
| Neutrophils – 01 | Folliculitis decalvans – 01 |
Microscopy of the hair follicles was also done and most of the hairs which were studied were in the anagen phase, followed by the telogen and the catagen phases [Table/Fig-4].
Microscopy of hair follicle with stage
| Findings |
|---|
| Average no/ of hair follicles per 1mm | 1.0 |
| Stage of hair in biopsy specimen (%) | |
| Anagen | 86.3 |
| Catagen | 5.6 |
| Telogen | 8.1 |
The histopathological features of various lesions were studied and analysed. The differences between lupus erythematosus, lichen planopilaris and folliculitis decalvans have been shown in [Table/Fig-5].
Comparison of histopathological features of lupus erythematosus, lichen planopilaris and folliculitis decalvans
| Histopathological features | Lupus erythematosus | Lichen planopilaris | Folliculitis decalvans |
|---|
| Hyperkeratosis extrafollicular | + | - | - |
| Horn plug | + | + | - |
| Epidermal atrophy | + | - | + |
| Vacuolar degeneration of basal cells | + | +/- | + |
| Neutrophilic folliculitis | - | - | + |
| Lichenoid Perifolliculitis | + | + | - |
| Dermal lymphocytic periecrine infiltrate | + | - | - |
| Fibrous tract replacing follicle | + | + (Colloid bodies) | + |
| Extrafollicular extensive dermo-hipodermal fibrosis | +/- | - | + Dermal |
| Thickened basement membrane (epidermal or follicular) | + | - | - |
Discussion
Alopecias can be broadly classified into the non-scarring or the non-cicatricial and the scarring or the cicatricial forms. Pathologically, a scar constitutes the end point of reparative fibrosis, with permanent destruction of the pre-existing tissue [7].
Scarring alopecias are further subdivided into the primary and the secondary types. In primary scarring alopecias, the hair follicle is the primary target of destruction, which is microscopically evident as a “preferential destruction of the follicular epithelium and/or its associated adventitial dermis, with relative sparing of the reticular dermis [2].” This group includes the following clinical entities: Chronic Cutaneous Lupus Erythematosus (CCLE), Lichen Planopilaris (LPP), Pseudopelade of Brocq (PB), Folliculitis Decalvans (FD) and Dissecting Cellulitis/Folliculitis (DF) [7]. In the present study, 24 cases of primary SA were diagnosed, of which 19 were lupus erythematosus, 3 were lichen planopilaris and on case was non specific SA. There was a single case of folliculitis decalvans.
The term ‘secondary scarring alopecia’ implies that a follicular destruction is not the primary pathologic event. Exogenous factors such as burns, and endogenous infiltrative and inflammatory diseases, such as sarcoidosis, pemphigus vulgaris and reticular dermal sclerosis, can result in secondary alopecias [7]. In the present study, secondary alopecia was seen in 8 cases, of which there were 4 cases of morphea and one each case of lupus vulgaris, congenital absence of skin, burn and sarcoidosis.
In 2001, a group of hair clinicians, pathologists and researchers, under the rubric of the North American Hair Research Society (NAHRS), issued a consensus opinion on the classification of primary cicatricial alopecias. The proposed classification sub – divided the primary scarring alopecias on the basis of the predominant type of inflammatory cell component, an approach that had already been published and was further refined by the workshop. In addition to the lymphocyte – and the neutrophil – associated subgroups, a mixed and a nonspecific group were differentiated and were newly defined [7]. In the present study, primary SA was classified, based on the inflammatory infiltrate, according to the North American Hair Research Society’s (NAHRS’) classification. Primary SA which showed a lymphocytic infiltration was seen in 23 cases, of which 19 were lupus erythematosus, 3 were lichen planopilaris and case was non – specific SA. A neutrophilic inflammatory infiltrate was seen in only one case i.e., folliculitis decalvans.
In the late phase of cicatricial alopecias, a histopathologic diagnosis is more difficult because the main criteria of classification, i.e., the type of inflammatory infiltrate, cannot always be evaluated. In these cases, additional criteria, such as the evaluation of the perifollicular elastic sheet and the fibrosis, can be useful [7].
The histopathological interpretation of the scalp biopsy specimens of the patients with alopecia, whether scarring or non – scarring, may represent a challenging task, especially in the absence of a good, definitive clinical history, adequate tissue sampling, and an appropriate grossing technique [2].
Lupus erythematosus and Lichen planopilaris were the most common causes of lymphocytic primary cicatricial alopecias in our study [Table/Fig-6].
Showing histopathological diagnosis of various scarring alopecias
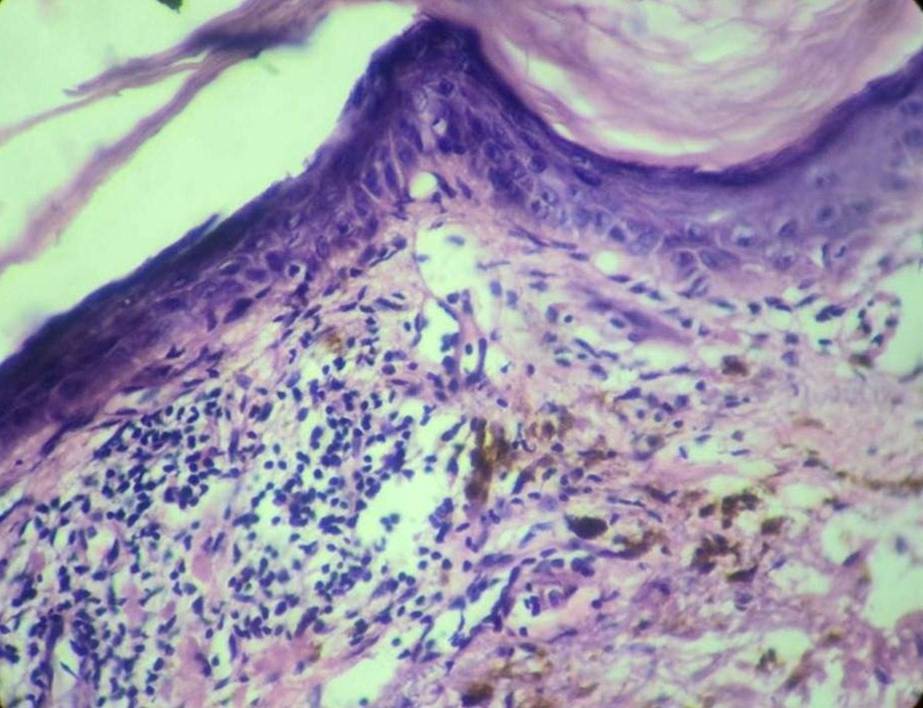
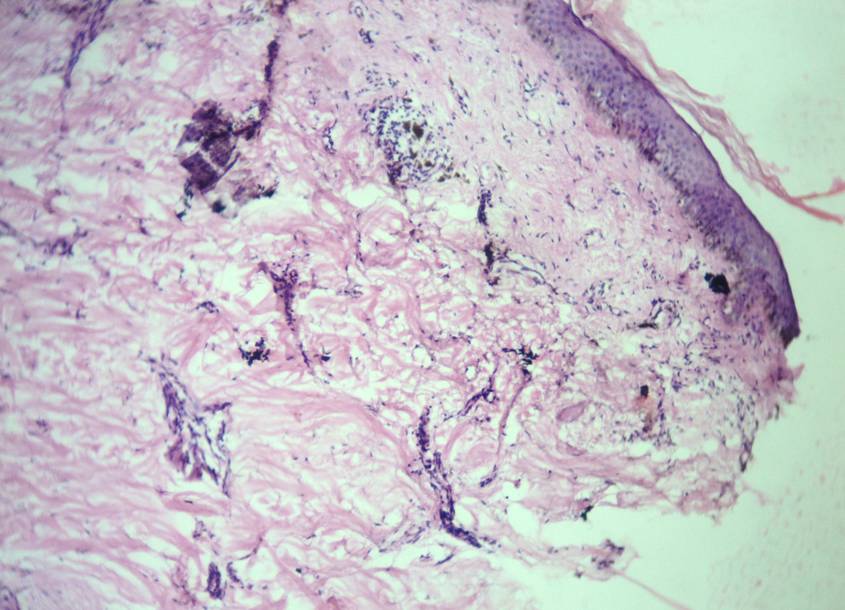
Photomicrograph showing atrophic epidermis with dense lymphocytic infiltrate and fibrosis of dermis (Lupus erythematosus)
Clinical photograph showing loss of hair (Lichen planopilaris)

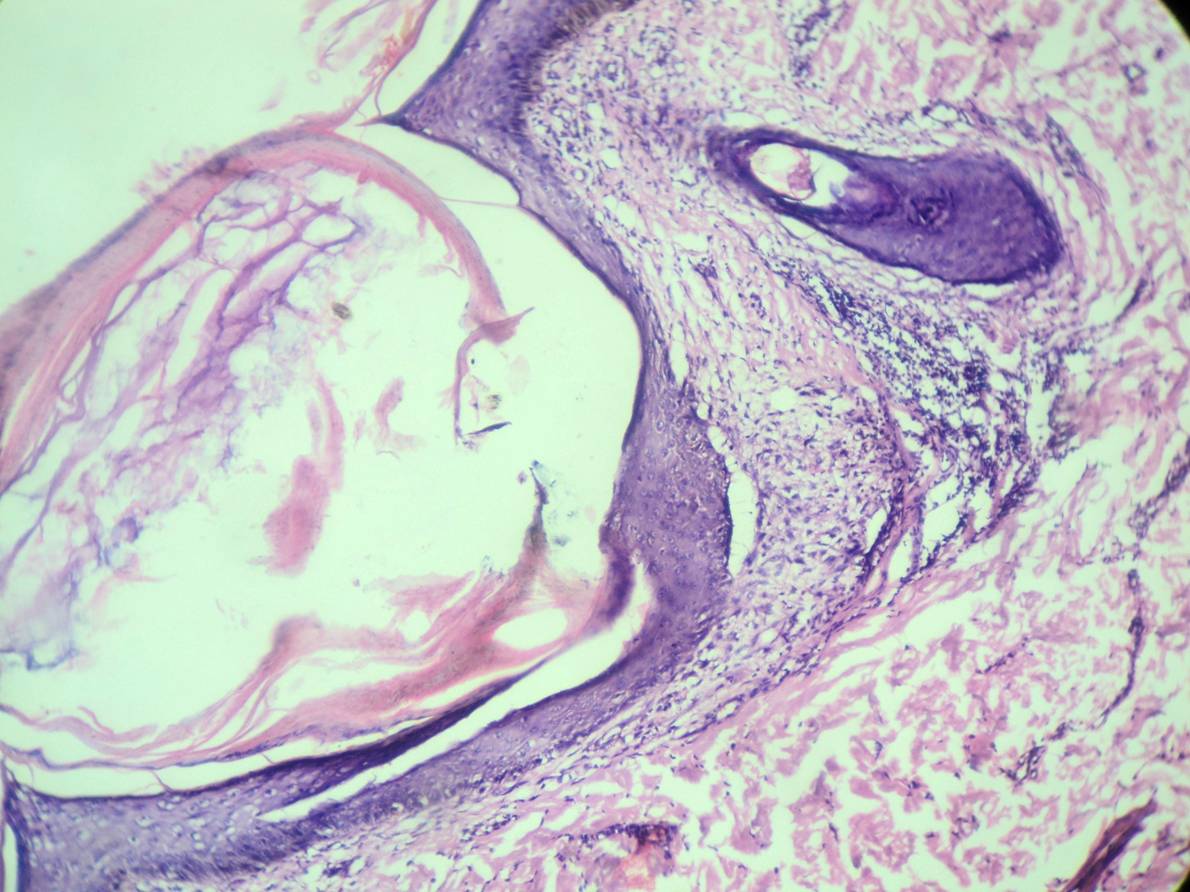
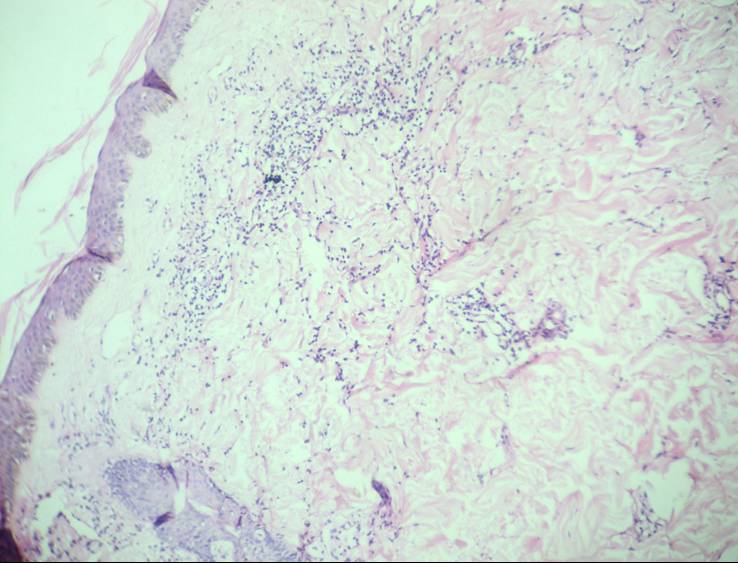
Photomicrograph showing follicular plugging with dense peri-follicular lymphocytic infiltrate and fibrosis of dermis (Lichen planopilaris).
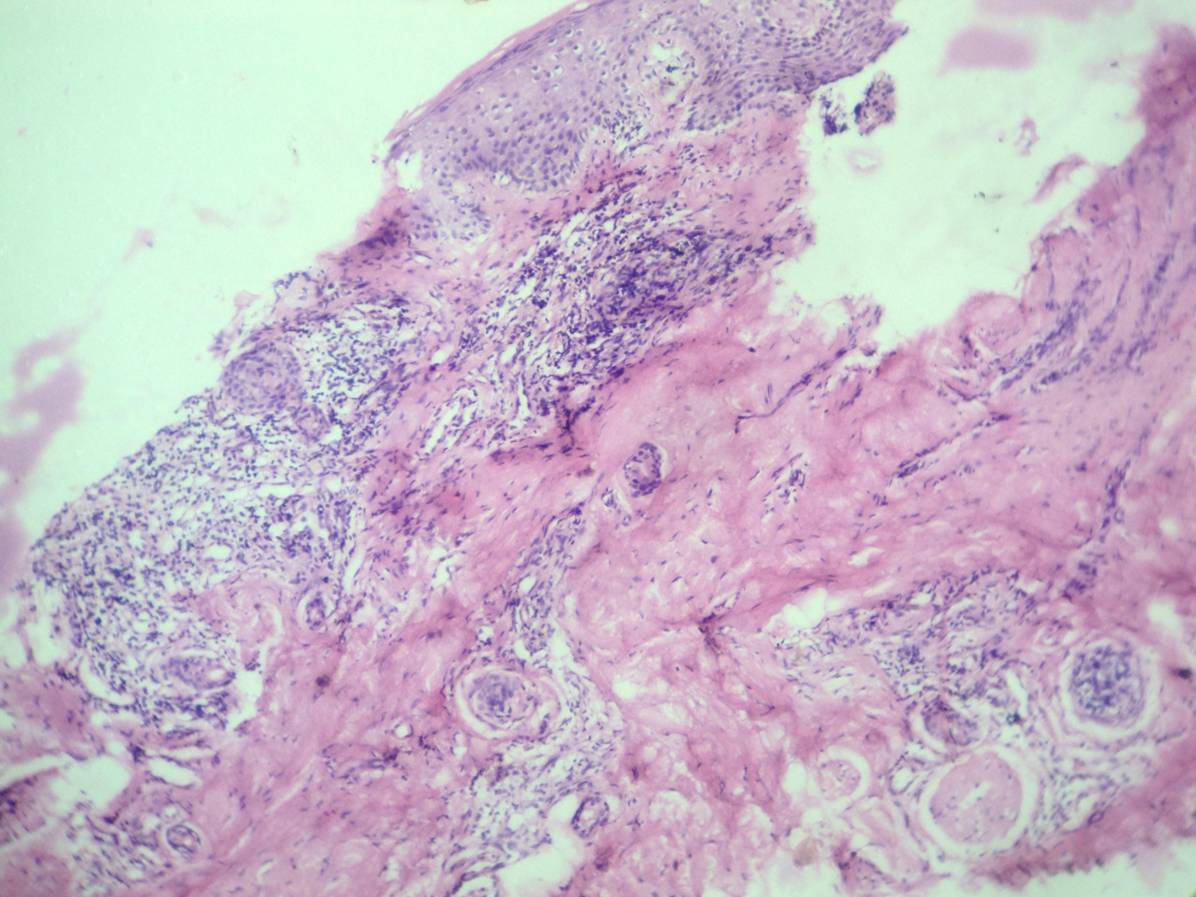
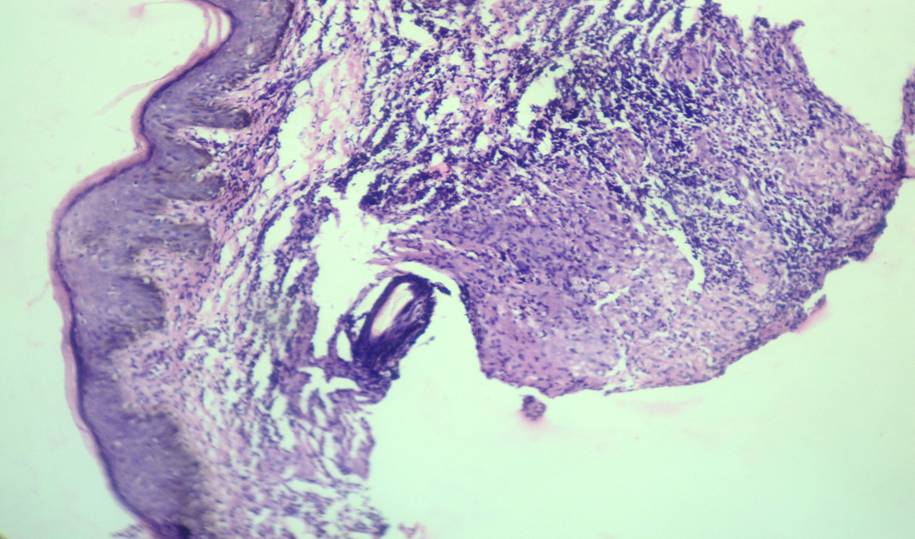
Photomicrograph showing dense peri-follicular neutrophilic infiltrate and fibrosis of dermis (Folliculitis decalvans – Low Power)
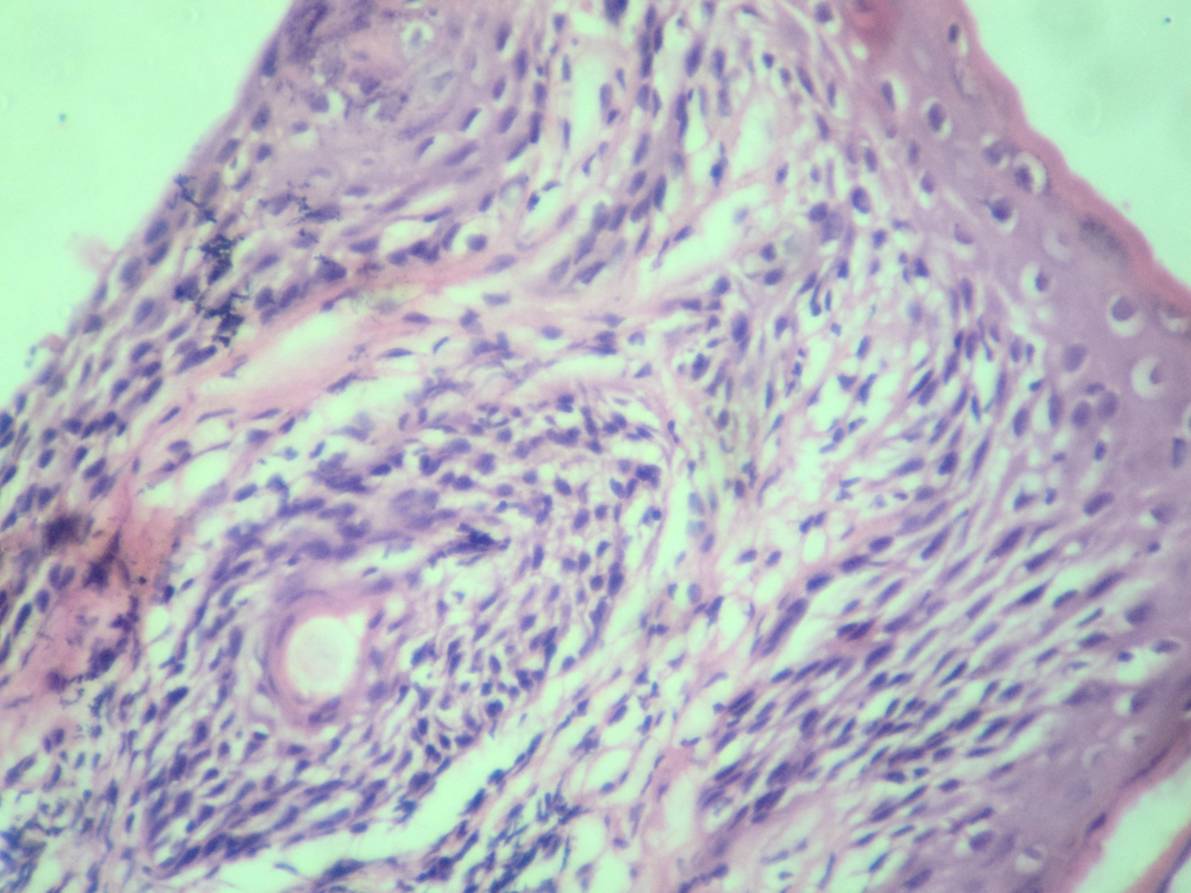
Photomicrograph showing dense peri-follicular neutrophilic infiltrate (Folliculitis decalvans – High Power)
Clinical photograph showing patchy loss of hair (Non specific SA)

Photomicrograph showing few follicles with sparse perifollicular lymphocytic infiltrate with dense fibrosis (Non specific SA)
Photomicrograph showing atrophic follicles with sparse peri-follicular lymphocytic infiltrate and dense fibrosis (Morphea)
Clinical photograph showing scarring alopecia (Lupus vulgaris)

Photomicrograph showing atrophic follicles with dense peri-follicular lymphocytic infiltrate, fibrosis with reticular dermis showing a granuloma (Lupus vulgaris)
Photomicrograph showing thinned out epidermis with atrophic follicles, sparse peri-follicular lymphocytic infiltrate & mild fibrosis (Congenital absence of skin)

The primary cicatricial alopecias are classified, based on the predominant type of inflammatory cells that attack the hair follicles: i.e., lymphocytes, neutrophils, or mixed inflammatory cells, because the treatment strategies are different for each subtype and for each patient.
The treatment of the lymphocytic group of cicatricial alopecias, which include lichen planopilaris, frontal fibrosing alopecia, central centrifugal alopecia, and pseudopelade (Brocq), involves the use of anti – inflammatory medications. The goal of the treatment is to decrease or eliminate the lymphocytic inflammatory cells that attack and destroy the hair follicles. The oral medications may include hydroxychloroquine, doxycycline, mycophenolate mofetil, cyclosporine, or pioglitazone. The topical medications may include corticosteroids, topical tacrolimus, topical pimecrolimus, or Derma-Smoothe/FS scalp oil. Triamcinolone acetonide (a corticosteroid) may be injected into the inflamed and the symptomatic areas of the scalp [9].
The treatment of the neutrophilic group of cicatricial alopecias (folliculitis decalvans and tufted folliculitis) is directed at eliminating the predominant microbes that are invariably involved in the inflammatory process. Oral antibiotics are the mainstay of the therapy. Topical antibiotics and anti-inflammatory medications may be used to supplement the oral antibiotics [9].
The treatment of the mixed group of cicatricial alopecias (dissecting cellulitis and folliculitis keloidalis) may include antimicrobials, anti-inflammatory medications and isotretinoin (the starting dose must be small). Infliximab may be helpful in the treatment of the resistant dissecting cellulites [9].
Hair transplantation can only be done in the patients who have normal healthy hair in the donor area. Scar revisions with/without a tissue expander and flap are the major surgical procedures for scarring alopecia, and there have been few reports on hair transplantation into the scar tissue. There is an apprehension of a lower survival rate of the donor hair for scarring alopecia, due to a poorer blood supply. However, hair transplantation can also show good results with the use of appropriate techniques and guidelines [10]. A combined use of hair auto grafting, followed by topical minoxidil 5%, appears to be an effective method in the treatment of irreversible alopecia [11].
The points which have to be noted when scarring alopecia is diagnosed.
The biopsy should be taken from the scalp areas which show signs of inflammation.
If it is taken from the atrophic scalp areas, it reveals only follicular or dermal fibrosis.
Transverse sections allow us to count and measure all the follicles in the specimen.
The key to a successful interpretation is the familiarity with the normality, both in terms of the follicular anatomy and the follicular size and number. A normal follicular unit from a normal scalp biopsy specimen shows 3-4 terminal follicles and one vellus follicle.
Conclusion
Adequate tissue sampling and appropriate laboratory processing, in combination with pertinent clinical information, provide the key to a histopathological diagnosis. The appropriate counselling and treatment can then be specifically directed.