Introduction: An increase in the Left Ventricular Mass as a result of muscle hypertrophy, has emerged as a powerful pressure independent risk factor for the cardiovascular mortality and morbidity. It is associated with a risk of death that is 3 times greater than the risk which is associated with hypertension alone. For the development of Left Ventricular Hypertrophy (LVH), in addition to a chronic increase in the pressure and/or volume overload, an elevation in the plasma ACE activity, plasma aldosterone levels, and the angiotensin-II concentrations play a major role .In this study, the effect of Telmisartan, a selective angiotension-II receptor blocker, was compared with that of Atenolol, a selective β1 adrenergic receptor blocker, on the regression of LVH in the patients of essential hypertension.
Material and Method: Essential hypertensive patients with LVH were selected for this study, as per the inclusion and exclusion criteria. This study was carried out on two groups of hypertensive patients with LVH:
Group-1 : The patients who were taking telmisartan 80 mg OD.
Group-2 : The patients who were taking atenolol 50 mg OD.
The blood pressure was measured and echocardiography was done in both the groups, prior to the treatment and 6 months after the treatment in the Department of Cardiology, MKCG Medical College Hospital, Brahmapur, India. The data were analysed by using the Student’s ‘t’ test.
Results: In the cases of Left Ventricular Mass Index (LVMI), which is a better indicator of LVH, in the Atenolol group, the mean value changed from 143.93 ± 2.44 gm/m2 to 130.16 ± 2.88 gm/m2 (t=5.83,p<0.01 versus baseline).In the Telmisartan group, the mean value changed from 184.67 ± 7.14 gm/m2 to 133.41 ± 4.24 gm/m2 (t=12.12, p<0.001 versus baseline). On comparing Telmisartan with Atenolol, Telmisartan was found to produce a greater (27.49%) reduction than Atenolol (9.68%). In the Telmisartan group, 13 patients out of 26 patients achieved a target value of LVMI that was <134 gm/m2 in males and <110 gm/m2 in females (50%). In the Atenolol group, only 9 patients out of 22 patients achieved a target value (40.90%).
Conclusion: Thus, Telmisartan a selective AT1 antagonist, possesses pharmacological effects beyond a blood pressure reduction in which the blockade of the AT1 receptor may lead to attenuation of the growth promoting action of Ang II. From this study, it is clear that Telmisartan is superior to Atenolol in achieving a regression of LVH, which is a better indicator of the cardiovascular morbidity and mortality.
Left ventricular hypertrophy, Hypertension, Telmisartan
Introduction
In the modern era, due to the increase in the industrial activities and the materialistic attitude, human beings are exposed to mental stress and physical strain, due to which the disease of ‘hypertension’ has assumed global significance. Hypertension – an elevated arterial pressure, is one of the most important public health problems in the developed countries. It is common, asymptomatic, and readily detectable. Usually, it is easily treatable, but it may lead to lethal complications if it is left untreated.
In the long run, hypertension is associated with an increase in the incidence of:
Cardiac complications: coronary artery disease, left ventricular failure, LVH, dysrrhythmia and sudden cardiac death.
Cerebrovascular diseases.
Nephropathy
Retinopathy
Over the past few years, the concomitant increase in the left ventricular mass (30% of the unselected hypertensive adults and 90% adults with severe hypertensive) as a result of muscle hypertrophy, has emerged as a powerful pressure independent risk factor for the cardiovascular mortality and morbidity [1]. It is associated with a risk of death that is 3 times greater than the risk which is associated with hypertension alone [2]. Regression of left ventricular hypertrophy (LVH) may be associated with an improvement of prognosis [3].
Several studies have showed that cardiac hypertrophy is reversed disproportionately by various antihypertensive drugs [4].
However angiotensin converting enzyme inhibitors, β adrenergic blockers, Diuretics and calcium channel blockers were found to rapidly reduce left venfetricular mass [5].
For the development of LVH, in addition to a chronic increase in the pressure and/or volume overload, an elevation in the plasma ACE activity, plasma aldosterone levels, and the angiotensin – II (Ang – II) concentrations play a major role [6]. Reduction of the Angiotensin – II levels after the ACE inhibition, may be responsible for the beneficial effects of the ACE inhibitors beyond the blood pressure-lowering activity. Apart from the cleavage of Ang – I by ACE, an alternative pathway exists for the formation of Ang – II, which leads to the so called ‘ACE escape’. Because almost all the known actions of Ang – II are mediated via the AT1 receptor subtype, the recently introduced specific Ang – II AT1 receptor antagonists could also be useful drugs in terms of the LVH regression [7]. As the Angiotension Receptor Blockers (ARB) potentially provide a more complete blockade of angiotensin – II, they may have a superior target organ protection. Telmisartan is a relatively recently developed ARB with a long elimination half life (approximately 24 hour) that has shown to provide well tolerated 24 hour blood pressure control with once daily dosing [8]. Nowadays In India and throughout the world it is being used very frequently for treatment of hypertension, for prevention of stroke and heart failure. So its role in prevention of the target end organdamage is to be studied here.
In view of the existing background, this prospective, randomised, cross – sectional study was undertaken, with an aim to study the:
Effect of Telmisartan on the regression of LVH in essential hypertensive patients
Effect of Atenolol on the regression of LVH in essential hypertensive patients
Material and Methods
Study Population
The present study was done to compare the effect of Telmisartan a selective angiotension-II receptor blocker with Atenolol a selective β1 adrenergic receptor blocker, on regression of LVH in patients attending Cardiology, Department of MKCG Medical College Hospital, Brahmapur,India, during the period 2005 to 2007.
Study Period
For each patient the study was conducted for 6 months duration. Blood pressure and Echocardiography was measured in both groups prior to treatment and 6 months after the treatment in Department of Cardiology, MKCG Medical College Hospital, Brahmapur,India.
Selection of Patients
Essential hypertensive patients with LVH were selected for this study as per inclusion and exclusion criteria. After the written informed consent these patients were enrolled and allotted to a group using computer generated random numbers.
Inclusion Criteria:Patients with moderate to severe hypertension having LVH.
Exclusion Criteria:Patients with secondary hypertension.
Pregnancy induced hypertension.
Patients with known cardiovascular abnormalities like valvular heart disease, cardiomyopathies.
Ethical Clearance
Institutional Ethical Committee approval and written permission from the Superintendent, the concerned H.O.D.s of MKCG Medical College Hospital, Brahmapur were obtained, prior to actual study.
Method of Study
Study carried out in two groups of Hypertensive patients with LVH:
Group – 1: Patients taking telmisartan 80 mg OD.
Group – 2: Patients taking atenolol 50 mg OD.
Blood pressure and Echocardiography was measured in both groups prior to treatment and 6 months after the treatment in Department of Cardiology, MKCG Medical College Hospital, Brahmapur,India.
Echocardiography
Echocardiography was done in the Department of Cardiology, MKCG Medical College, Brahmapur. Because of its simplicity, reproducibility, relative low cost and lack of adverse effects, M-mode echocardiography was used in the measurement of LV diameter, as well as septal and posterior wall thickness. All tracings for LV dimensions were recorded at the level of the tips of the mitral valve. LV dimensions and wall thickness were measured by the leading edge technique as per the recommendation of American Society of Echocardiography at both end diastole (Beginning of QRS complex) and end systole (shortest LV dimension).
Measurement of ventricular wall thickness was made by the criteria developed by investigators of University of Pennsylvania (The Penn Convention) which excludes endocardial echoes. LV mass was then calculated by subtracting the internal volume (chamber) from the external volume (total) and then multiplying by the specific gravity of the myocardium (1.04).
The following calculations were made using the regression corrected cube formula [Table/Fig-1]:
Schematic representation of cubed formula determining LV mass
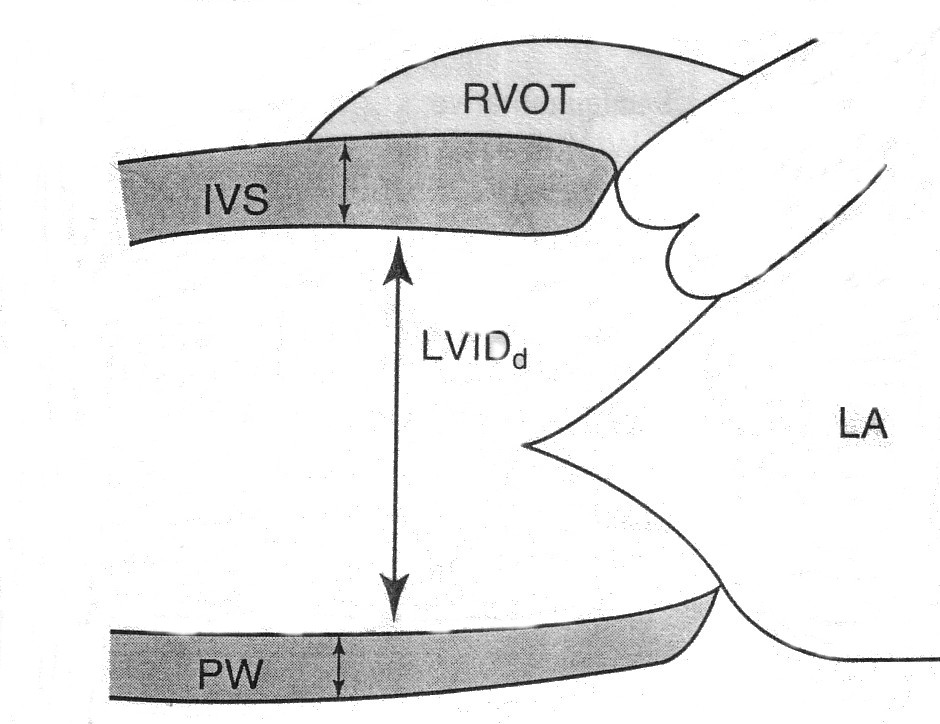
LV volume by cube formula.
Internal volume (chamber) LVV = (LVIDd)3
External volume (total) = (LVIDd+IVST+LVPWT)3
LVM (gm) = 1.04 (Ext. Vol. – Int. Vol.) – 13.6
= 1.04 [(LVIDd+IVST+LVPWT)3-LVIDd3]-13.6
LVV = Left ventricular volume.
LVM (gm) = Left ventricular mass in grams
LVIDd = Left ventricular internal dimension at end diastole
IVST= Interventricular septal thickness.
LVPWT= Left ventricular posterior wall thickness
LVMI (gm/m2) = LVM / B.S.A.
LVMI = Left ventricular mass index
B.S.A. = Body surface area
Study Protocol
The patient with LVMI > 134 gm/m2 for male and LVMI > 110gm/m2 for female were considered having LVH 39. They were included in the study and given either 80 mg of Telmisartan or 50mg of Atenolol. Since these patients are having end organ damage they required addition of hydrochlorothiazide 12.5mg in both groups. B.P measurement and Echo was done in both groups priors to start of treatment and six months after treatment.
Statistical Analysis
Data were analysed by using SPSS and Excel software by student’s t test (both paired and unpaired).
Results
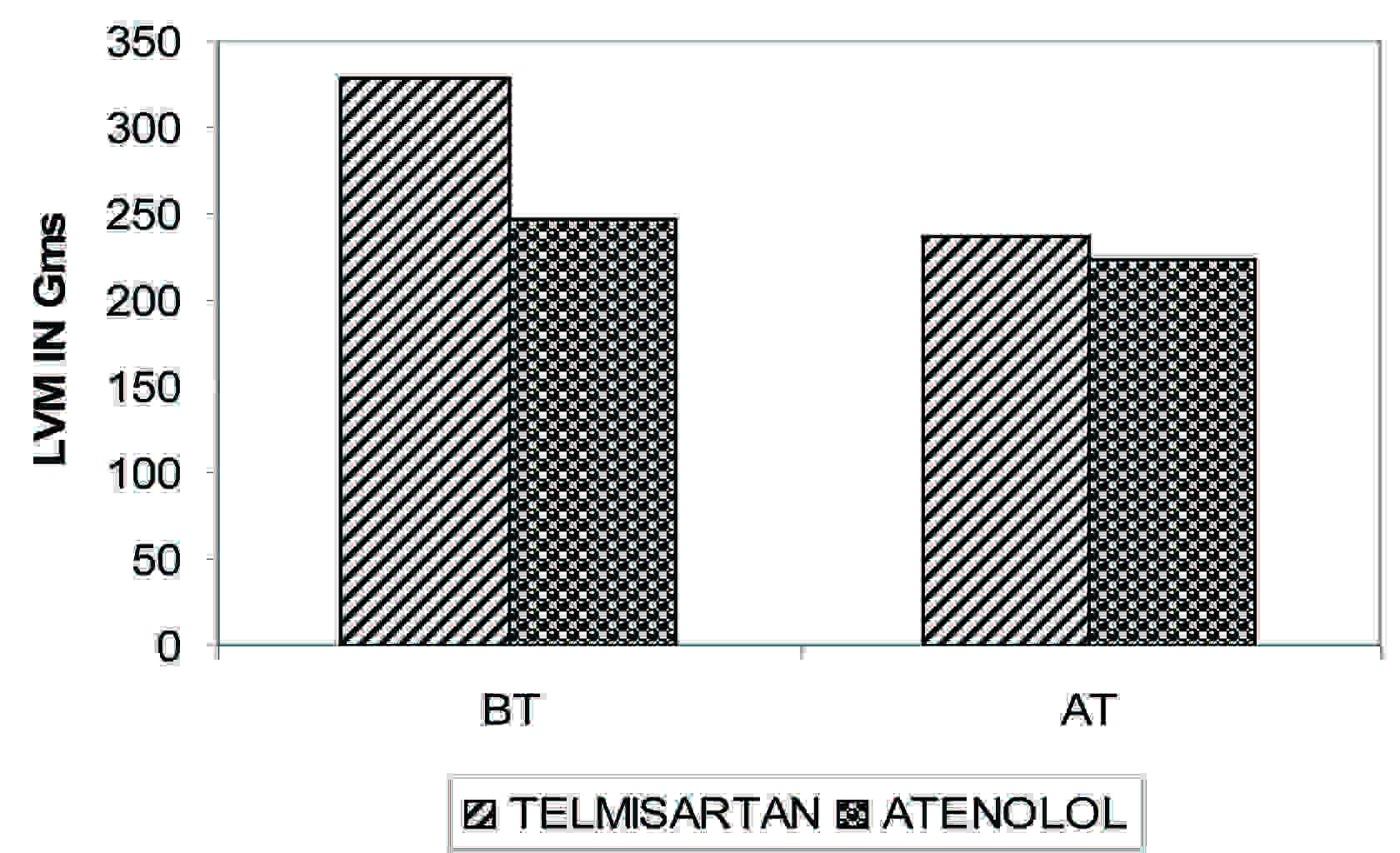
The LV mass by M mode echocardiography was measured before and six months after treatment. Different parameter like IVST, LVPWT, LVID, LVM and LVMI were measured. When Left ventricular mass (LVM) was compared , Both the groups were different before the treatment (p<0.001), But both exhibited equal effect (p>0.05) [Table/Fig-2]. So Telmisartan reduces LVM As it is done by Atenolol. Both drugs are effective but Telmisartan is more effective in reducing LVM (p<0.001 for Telmisartan in comparison to p < 0. 01 for Atenolol). The data are depicted in [Table/Fig-3] and [Table/Fig-4].
| Drugs | LVM ± SE | Paired t test |
|---|
| BT | AT | ‘t’ | ‘p’ |
|---|
| Telmisartan (n=26) | 328.89±13.13 | 237.16±7.67 | 11.28 | <0.001 |
| Atenolol (n=22) | 247.41±4.49 | 223.68±5.18 | 5.86 | <0.01 |
| Unpaired t test df=46 |
| ‘t’ | 5.51 | 1.39 | X |
| ‘p’ | <0.001 | >0.05 | X |
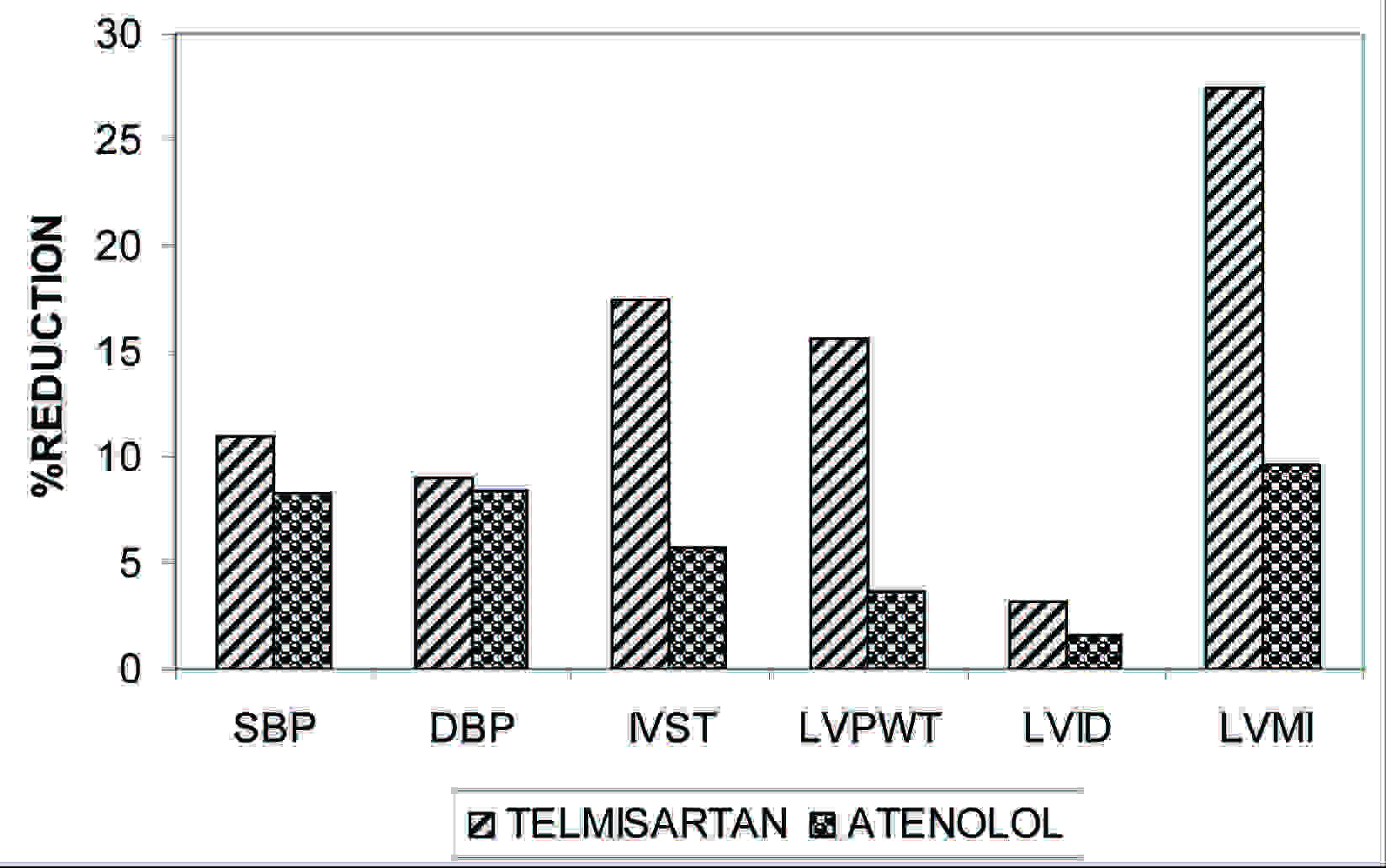
Effect of drugs on percent reduction of different parameters
| Drugs | SBP | DBP | IVST | LVPWT | LVID | LVMI |
|---|
| TELMISARTAN | 10.96 | 9.05 | 17.5 | 15.56 | 3.21 | 27.49 |
| ATENOLOL | 8.27 | 8.45 | 5.73 | 3.68 | 1.59 | 9.68 |
In case of LVMI which is a better indicator of LVH, in Atenolol group the mean value changed from 143.93 ± 2.44 gm/m2 to 130.16± 2.88 gm / m2 (t=5.83,p<0.01 versus baseline).In Telmisartan group the mean value changed from 184.67 ±7.14 gm / m2 to 133.41 ± 4.24 gm/m2 (t=12.12,p<0.001 versus baseline). In comparing Telmisartan with Atenolol, t=5.03, p<0.001(BT), t = 0.61, p>0.05(AT) [Table/Fig-5] and [Table/Fig-6]. Telmisartan produced greater (27.49%) reduction than Atenolol (9.68%) [Table/Fig-3].
| Drugs | LVMI ± SE | Paired t test |
|---|
| BT | AT | ‘t’ | ‘p’ |
|---|
| Telmisartan (n=26) | 184.67±7.14 | 133.41±4.24 | 12.12 | <0.001 |
| Atenolol (n=22) | 143.93±2.44 | 130.16±2.88 | 5.83 | <0.01 |
| Unpaired t test df=46 |
| ‘t’ | 5.03 | 0.61 | X |
| ‘p’ | <0.001 | >0.05 | X |
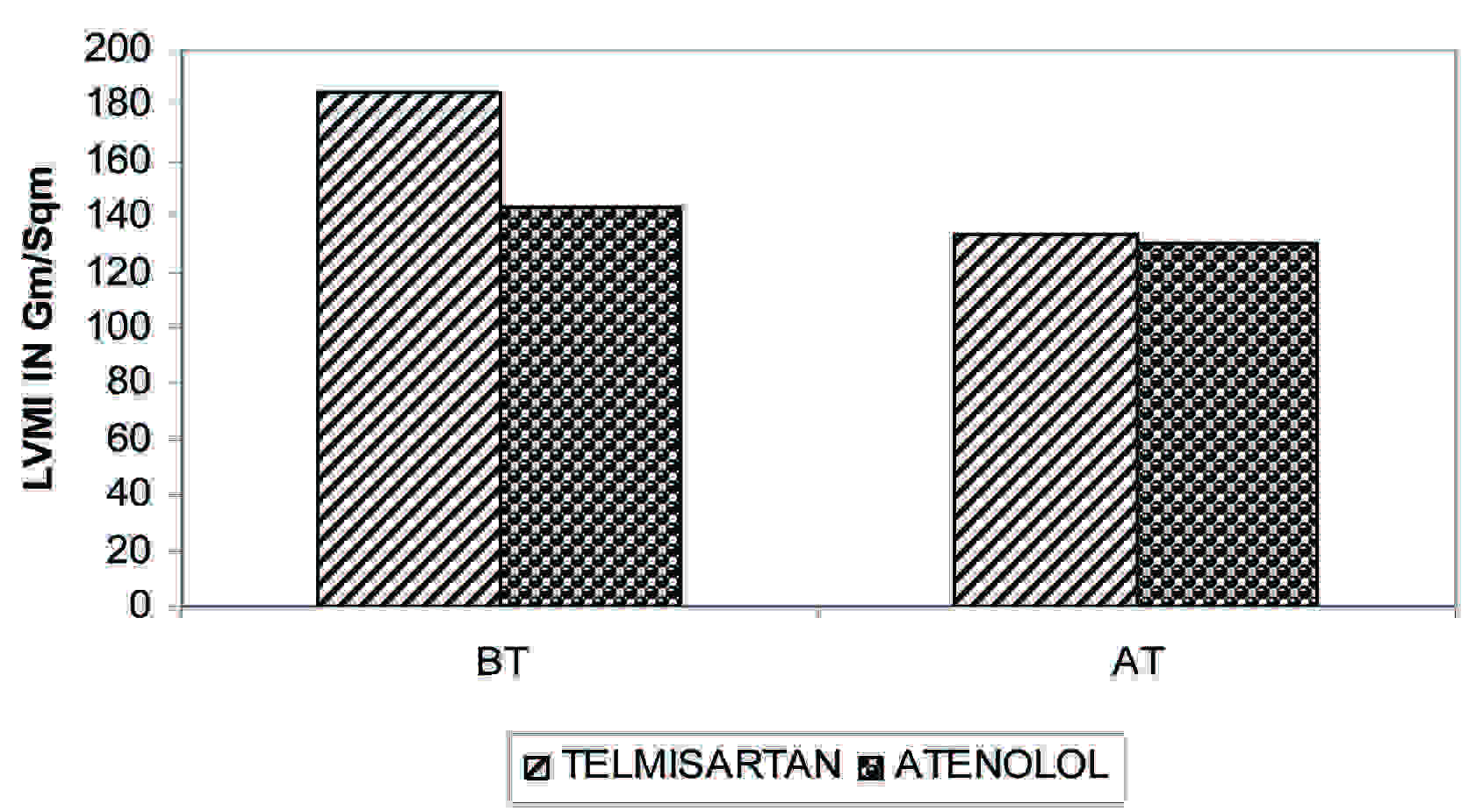
When Left ventricular mass index (LVMI) was compared was Both the groups were different before the treatment (p<0.001), But both exhibited equal effect (p>0.05). So Telmisartan reduces LVMI as it is reduced by Atenolol. Both drugs are effective but Telmisartan is more effective in reducing LVMI (p< 0.001). The data are depicted in [Table/Fig-5] and [Table/Fig-6].
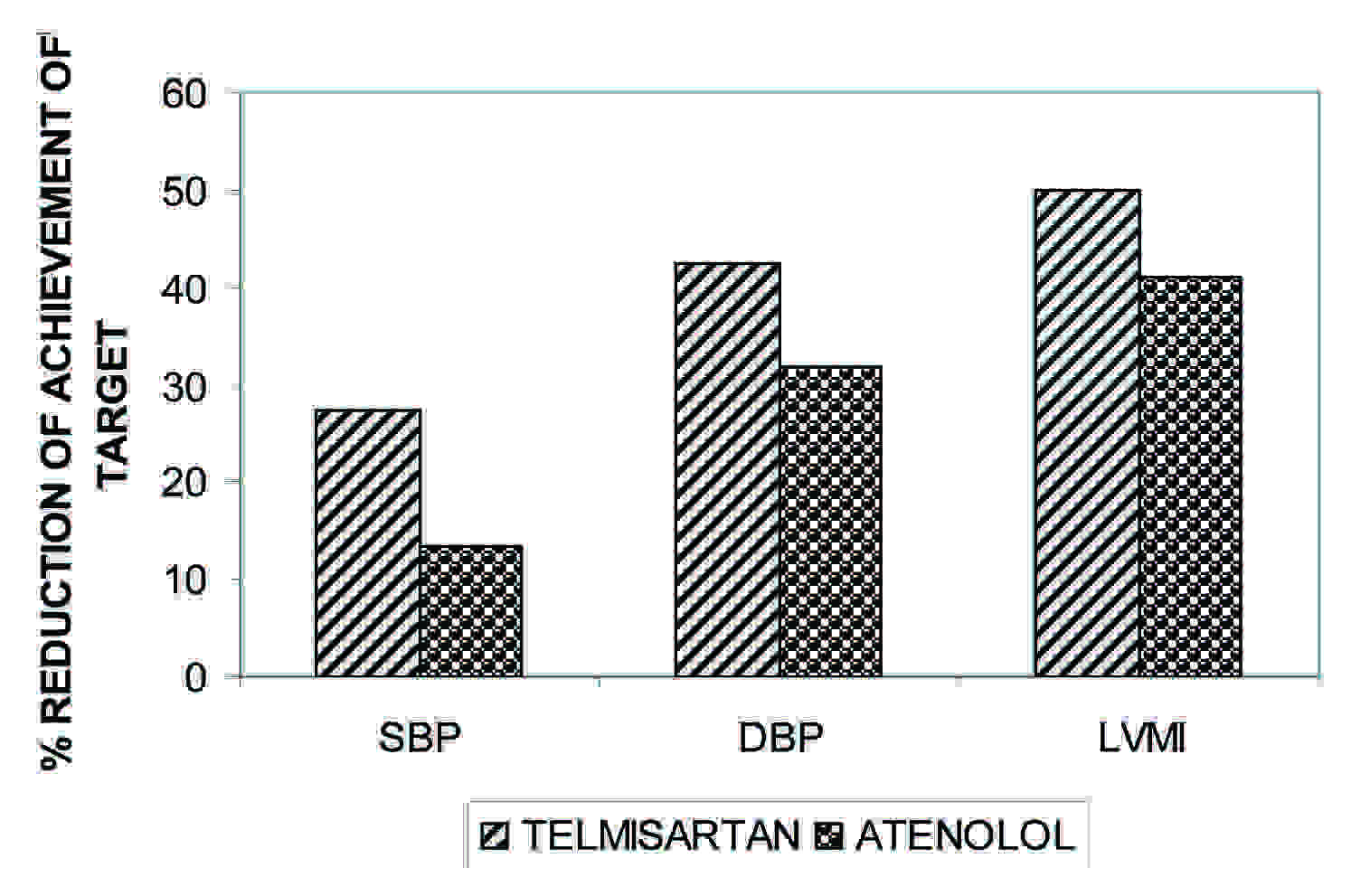
Telmisartan is having greater % reduction of all the parameters like SBP, DBP, IVST, LVPWT, LVID, LVMI in comparison with Atenolol. The data are depicted in [Table/Fig-7].
Effect of drugs on percent reduction of different parameters
Telmisartan is also having more % of patients achieving target BP (<140/90 mm of mercury) achievement in comparison to Atenolol. But Telmisartan is having greater % of patients achieving target level of LVMI (<134 gm/m2 for male and <110 gm/m2 for female). The data are depicted in [Table/Fig-8] and [Table/Fig-9].
Effect of drugs on different parameters
| PARAMETERS | TELMISARTAN (n=26) | ATENOLOL (n=22) |
|---|
| PTS NO | % | PTS NO | % |
|---|
| SBP (NORMALISED) | 6 | 27.27 | 4 | 13.38 |
| DBP (NORMALISED) | 11 | 42.30 | 7 | 31.81 |
| LVMI (NORMALISED) | 13 | 50 | 9 | 40.90 |
Effect of drugs on different parameters
Discussion
In comparing Telmisartan with Atenolol, Telmisartan produced greater (27.49%) reduction than Atenolol (9.68%). It can be compared with studies conducted by Dahlof B, Devereu RB (LIFE study), Devereu RB, Daholf B, Levy D et al., (The PRESERVED study) [9], studies conducted by OV Ivanova, OA Fomicheva et al., and Petra A, Thurmann MD, Peter Kennedy and ELITE trial [10].
The addition of HCTZ was required equally both in my treatment groups and a beneficial influence of this diuretic on LVMI cannot be ruled out. But according to the Liebson et al., [11], the major influence of a diuretic was confined predominantly to the LVID rather than the wall thickness parameters.
In the present study the mean LVMI before treatment was seen to higher than the other studies. This is probably because of delayed detection of hypertension as patients in our country are known to seek medical advice quiet late in the course of disease. It is also known that hypertension may sometimes remain asymptomatic for as long as 10 – 20 years leading to delayed detection and consequent progression of cardiovascular disease.
But in case of LVMI in Telmisartan group 13 patients of out of 26 patients achieved target value of <134 gm/m2 in male and <110 gm/m2 in female (50%). In Atenolol group only 9 patients out of 22 patients achieved a target value (40.90%) [Table/Fig-8]. Thus Telmisartan a selective AT1 antagonist possess pharmacological effect beyond blood pressure reduction in which blockade of AT1 receptor may lead to attenuation of growth promoting action of Ang II.
Conclusion
So from this study it is observed that both the drugs reduce left ventricular mass significantly. In comparing both the drugs percentage reduction of blood pressure is almost similar. But comparison regarding lowering of LVMI Telmisartan produced much greater reduction of LVMI than Atenolol. From this study it is amply clear that Telmisartan is superior to Atenolol in achieving regression of left ventricular hypertrophy which is a better indicator for cardiovascular morbidity and mortality than the lowering of blood pressure. Hence Telmisartan should always be the preferred drug in patients of essential hypertension with evidence of left ventricular hypertrophy
But in this study the sample size was very small [(Telmisartan (n=26), Atenolol (n=22)] as there is very difficult to find patients having LVH taking single drugs. Also the duration of the study is very less. So the effect of drugs on a large number of patients for a prolonged period has to be studied in future.
[1]. Messerli and Sorie, LVH and Cardiovascular mortality and morbidity, Drugs 44 (Suppl. 1) , 1992 [Google Scholar]
[2]. LVH in hypertensive persons, An H, Med ; Jan 1983 (Suppl. 18) [Google Scholar]
[3]. Muiesan ML, Salvetti M, Rizzoni D, Castellano M, Donato F, Agabiti Rosei E, Association of change in left ventricular mass with prognosis during long term antihypertensive therapyJ. Hypertens 1995 :1091-95. [Google Scholar]
[4]. Liebson PR, Granditis GA, Dianzumba S, Prineas RJ, Grimm RH, Neaton JD, Comparison of five antihypertensive monotherapies & placebo for change in left ventricular mass in patients receiving nutritional hygienic therapy in the treatment of Mild Hypertensive Study (TOMHS)Circulation 1995 91:698-706. [Google Scholar]
[5]. Reversal of left ventricular hypertrophy in essential hypertension. A meta-analysis of randomized double-blind studies. Schmieder RE, Martus P, Klingbeil AJAMA 1996 May 15 275(19):1507-13. [Google Scholar]
[6]. Sadoshima J, Izumbo S, Molecular characterization of angiotensin II induced hypertrophy of cardiac myocytes & hyperplasia of cardiac fibroblastsCirculation 1993 73:413-23. [Google Scholar]
[7]. Dahlof B, Effect of angiotensin II blockade on cardiac hypertrophy & remodeling: a reviewJ Hum Hypertens 1995 (Suppl. 5):37-44. [Google Scholar]
[8]. Smith DHG, Matzek KM, Dose response & safety of Telmisartan in patients with mild to moderate hypertensionJ clinical Pharmacol 2000 :1380-90. [Google Scholar]
[9]. Devereux RB, Dahlof B, Levy D, Pfeffer MA, Comparison of enalapril versus atenolol to decrease LVH in Systemic Hypertension (PRESERVE trial)Am J Cardiol 1996 78:61-65. [Google Scholar]
[10]. Pitt B, Segal R, Martinee FA, Randomised trial of Losartan versus Captopril in patients over 65 with heart failure (Evaluation of Losartan in the Elderly study, ELITE)Lancet 1997 349:747-52. [Google Scholar]
[11]. GOH Dinen JS, Rede JS, Massie BM, Effect of single drug therapy on reduction of LVM in mild to moderate Hypertension: comparison of six antihypertensive agentsCirculation 1997 95:2007-14. [Google Scholar]