Observation Units (OU) are dedicated areas where patients are treated or observed for a defined amount of time, to determine the need for admission [1,2]. These units offer treatment within defined areas for a longer period than the usual emergency department visits, but for a shorter period than for a full inpatient hospital admission [1–4]. The OU is an excellent option for relieving the high-volume stress in an overcrowded emergency department, which is a serious issue in the developing and the developed countries alike. Additionally, the OU could bring down the cost of the care by 50% as compared to the regular hospital admissions [1,5]. However, approximately 15-25% of the OU admissions result in unexpected hospitalisations [1,2,6]. The resultant additional transfer of care for both the patients and their families may decrease the efficiency of the patient care and the OU itself [1].
Till date, there are no reports on the OUs from the developing world. The clinical profiles of the paediatric patients who attend the OU and the presenting diagnoses which are responsible for the unexpected hospitalisations could be different for different geographical areas. This study aimed to explore the profile of the children who received a 23-hour OU care in the Indian setup and to determine the clinical diagnosis which was responsible for the unexpected hospitalisation in a 23-hour OU.
Methods
A prospective, observational study was done in the 6 bedded 23-hour OU of the Paediatric Emergency Department (PED) at the Government Medical College and Hospital, a tertiary care referral teaching hospital of northern India. This hospital caters to the low- medium socioeconomic class population. The data was collected from February-March 2011. Consecutive children who were aged upto 18 years and who presented to the PED were included. Informed consents were obtained from the parents/ guardians of all the children who were included in the study. Clearance was also obtained from the institutional ethics committee. The children who presented to the PED were triaged according to the WHO paediatric emergency triage and treatment algorithm [7] by the medical intern/s who was/were posted in the PED, which was crosschecked by a PED consultant. The children were excluded if they were directly admitted (i.e. if they were expected to stay in the hospital for > 24 hours); or directly discharged (i.e. if they visited the PED for trivial complaints which required outpatient visits). The rest were observed in the 23-hour OU based on the decisions which were taken by the senior resident or the PED consultant on call.
The children who were transferred to the 23-hour OU, were further followed up till 23 hours of stay in the hospital or till discharge, whichever was earlier. Our outcome measures were the proportion of the children who required unexpected hospitalisations and the presenting diagnoses which were responsible for unexpected hospitalisations in the 23-hour OU. The decision to discharge/admit was taken by the PED consultant. Descriptive statisticswere used for the primary outcomes. The clinical characteristics of the children who required unexpected hospitalisations were compared with those of those who were discharged from the 23-hour OU, by using the Student ‘t’ test and the Man-Whitney ‘U’ test. The data was analysed by using SPSS, version 17.0.
Results
Three hundred children (228 males and 72 females) presented to the PED over the period of the study duration. A majority (55%, n=165) of the children were triaged as non-urgent, 32% (n=97) as priority and 13% (n=38) as emergent. Among them, 173 (58%) were transferred to the 23-hour OU. The median age of the children who were shifted to the 23-hour OU was 24 months (IQR 11, 66 months). The male to female ratio was 3:1. Diarrhoea, bronchiolitis, seizures, thallasaemia, poisonings and pneumonia were responsible for three fourth of the patients who were observed in the 23-hour OU [Table/Fig-1].
Profile of children transferred to 23-hour OU
| Numbers | No. of children observed in 23-hour OU [N=173], (%) |
|---|
| Diarrhea | 34 (20) |
| Bronchiolitis | 27 (16) |
| Seizures | 26 (15) |
| Thallasemia | 24 (14) |
| Poisoning and animal bites | 9 (5) |
| Pneumonia | 8 (5) |
| Croup | 5 (3) |
| Bronchial Asthma | 5 (3) |
| Vague abdominal pain | 5 (3) |
| Others* | 30(17.3) |
* Others include: Viral hepatitis (n=2), high fever (n= 1), severe anemia (n= 1), urticaria (n= 1)
Of the 173 children who were transferred to the 23-hour OU, 16 (9%) required unexpected hospitalisations. The most common presenting diagnoses which were responsible for the unexpected hospitalisations were bronchiolitis and pneumonia (N=8, 50%, [Table/Fig-2]. The mean duration of the stay in the OU was 19 hours for the children who needed hospitalisation, as against 13 hours for those who were discharged (p=0.1). Out of the 157 children who were successfully discharged from the OU, none presented to our PED within the next 24 hours.
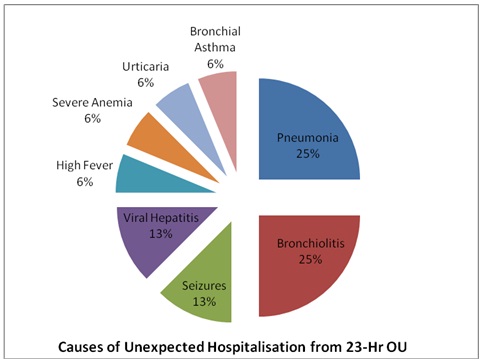
Causes of unexpected hospitalisation from 23 hours OU (N=16)
| Clinical diagnosis | No. of unexpected hospitalisations from 23-hour OU [N=16], (%) |
|---|
| Pneumonia | 4(25) |
| Bronchiolitis | 4(25) |
| Seizures | 2(13) |
| Viral Hepatitis | 2(13) |
| High Fever | 1(6) |
| Severe Anemia | 1(6) |
| Urticaria | 1(6) |
| Bronchial Asthma | 1(6) |
Thirty five children with pneumonia/ bronchiolitis were observed in the 23-hour OU [Table/Fig-1]. Of them, 8 required unexpected hospitalisations. The children with pneumonia/ bronchiolitis, who required unexpected hospitalisations (N=8),were compared with those who were discharged (N=27). On univariate analysis, it was found that there was no difference in the age at presentation 10.3 (3.8, 22.5) vs 8 (4, 24) months, p=0.9, the respiratory rate 51 (30,61) vs 44 (42, 58), the breaths per minute, p=0.6, the heart rate 129 (18) vs 134 (19), the beats per minute, p=0.5, the oxygen saturations [93 (3) vs 95 (3)%, p=0.5 and the duration of the symptoms 3 (1) vs 3 (1) days, p=0.9 between the two groups. The requirements of intravenous medications and intravenous fluids were also similar.
Discussion
In this prospective, observational study, 9% of the children who were observed in the 23 hours-OU required unexpected hospitalisations. Bronchiolitis and pneumonia were responsible for 50% of all the unexpected hospitalisations.
Although the concept of observation units has existed for the past two decades, studies which have been done on the paediatric age group, especially in the developing nations, is limited. The spectrum of the cases which presented to the OU in our study (diarrhoea, bronchiolitis, seizures, thallasemia, poisoning/ animal bites, and pneumonia) was similar to those in the previous published literature [1,2,8,9]. The frequency of the unexpected hospitalisations in our study was 9%. The frequency of the unexpected hospitalisations was 4% to 22% in the previous published studies [6,8,9].
In our study, respiratory ailments (pneumonia and bronchiolitis) were responsible for half of the unexpected admissions. In the previous reports too, the unexpected hospitalisation rates were high for the children with bronchiolitis and pneumonia [1,2,6]. Among the children with bronchiolitis and pneumonia who were observed in the 23 hours-OU in our study, no difference was found between the characteristics of the children who required unexpected hospitalisations versus those who were discharged [10].
There was a discharge rate of 91%, which is comparable to that in western studies [1,2,6,9].
Conclusions
The unexpected hospitalisations in the 23-hour OU in our study was 9%. Respiratory ailments (pneumonia and bronchiolitis) were responsible for half of the unexpected hospitalisations in the 23-hour OU.
What this study adds: The children with bronchiolitis and pneumonia were responsible for a majority of the unexpected hospitalisation rates in the 23-hour OU of a PED.
Limitations
However, there are certain limitations of the study. Firstly, this was a small study which was carried out bridging late winter through early spring season. This does not account for the patients in the summer and monsoon seasons. Secondly, we do not have a follow up of the children who were discharged from the 23-hour OU. It is possible that some patients who had been discharged successfully from our 23-hour OU had presented to another PED within a brief period.
Funding: None
* Others include: Viral hepatitis (n=2), high fever (n= 1), severe anemia (n= 1), urticaria (n= 1)