Meningioma is a common benign intracranial neoplasm. The incidence of an extracranial extension to other sites is rare. Due to the neglected intracranial component, the chances of an under diagnosis or a misdiagnosis of the extracranial component is there, which may adversely affect the management and therefore, the prognosis. Here, we are reporting a case of a 39 years old male patient with a preoperative probable diagnosis of a malignant bone tumour which involved the skull bone, which was made, based on the imaging studies , which was histopathologically found to be an invasive meningioma with an extensive extracranial skull vault involvement and was confirmed by immunohistochemistry. We have proposed a term, “carpet meningioma” for this extracranial invasive meningioma, because it had covered the skull vault like a carpet. The follow up studies after 1 year have revealed no evidence of a recurrence.
CASE REPORT
A 39 year old male patient was referred to our hospital for the complaint of recurrent headache since 20years and progressive disfigurement of face since 15years.He had no other significant complaints. On examination there was presence of approximately 13x10x6cm sized swelling over scalp extending from frontal to occipital region with firm consistency. A CT scan was done which was inconclusive with remote possibility of malignant transformation to oestosarcoma was given. Then MRI was ordered.
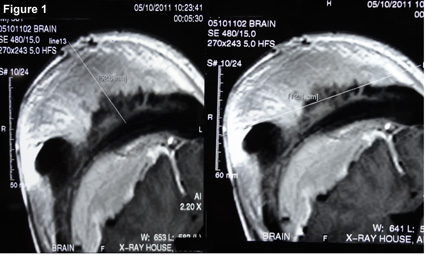
[Table/Fig-1] MRI of the brain with contrast: There was an evidence of a large soft tissue intensity lesion which involved the scalp on the right side, which had an approximate size of 10x10x6cm. The lesion was hypointense on the T1W images and it showed an intense enhancement on the post contrast study. The lesion involved all the layers of the scalp and it extended to involve the skull vault, with widening and marrow replacement in the diploic space. A large intracranial extension was seen in the form of an enhancing epidural component in the right frontoparietal region, with a maximum width of 3.4cm. The possibility of a malignant degeneration of some primary bony pathology was given.
MRI of the brain with contrast
Based on the clino-radiological findings, the surgical removal of the cranial vault was done.
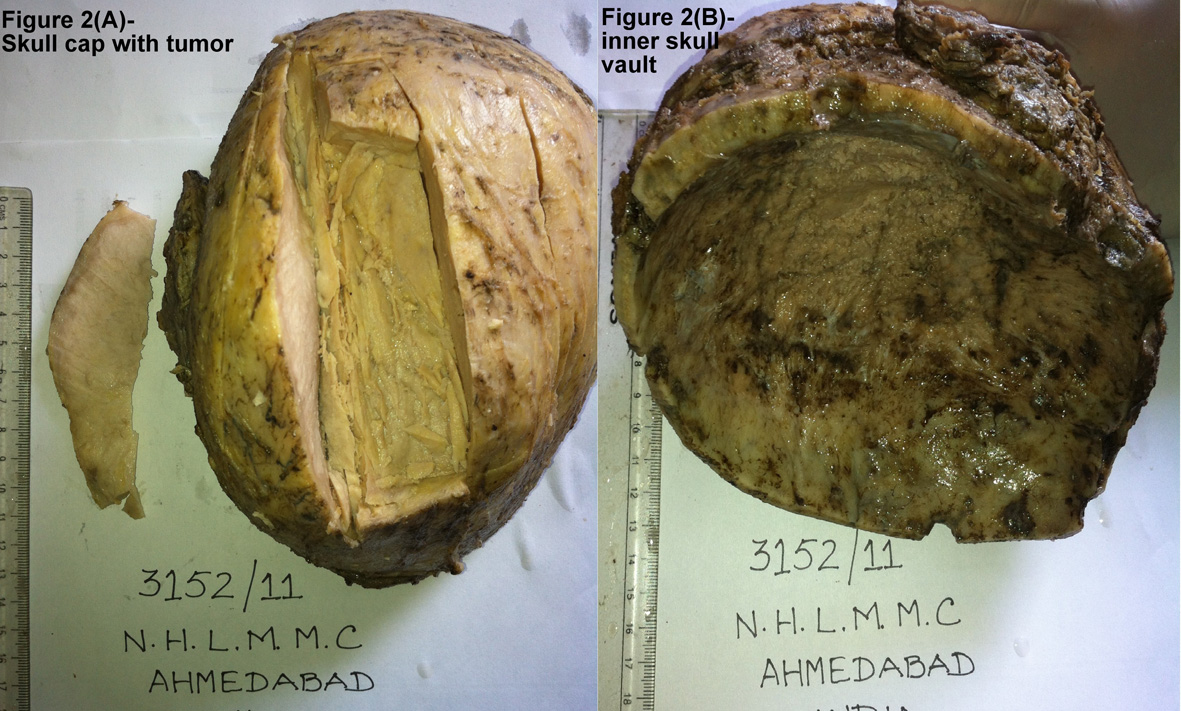
[Table/Fig-2] Gross appearance: (A) The skull cap with tumour- The specimen of the cranial vault with a part of the attached muscle measured 17x13x9 cm. The tumour which covered the skull cap measured 13x11x5.8 cm. The cut surface of the tumour was homogenous white. (B) The inner skull vault scrapping material measured 4x4cm in aggregates.
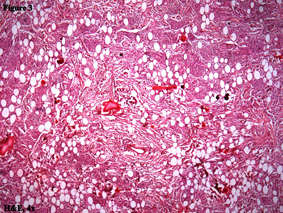
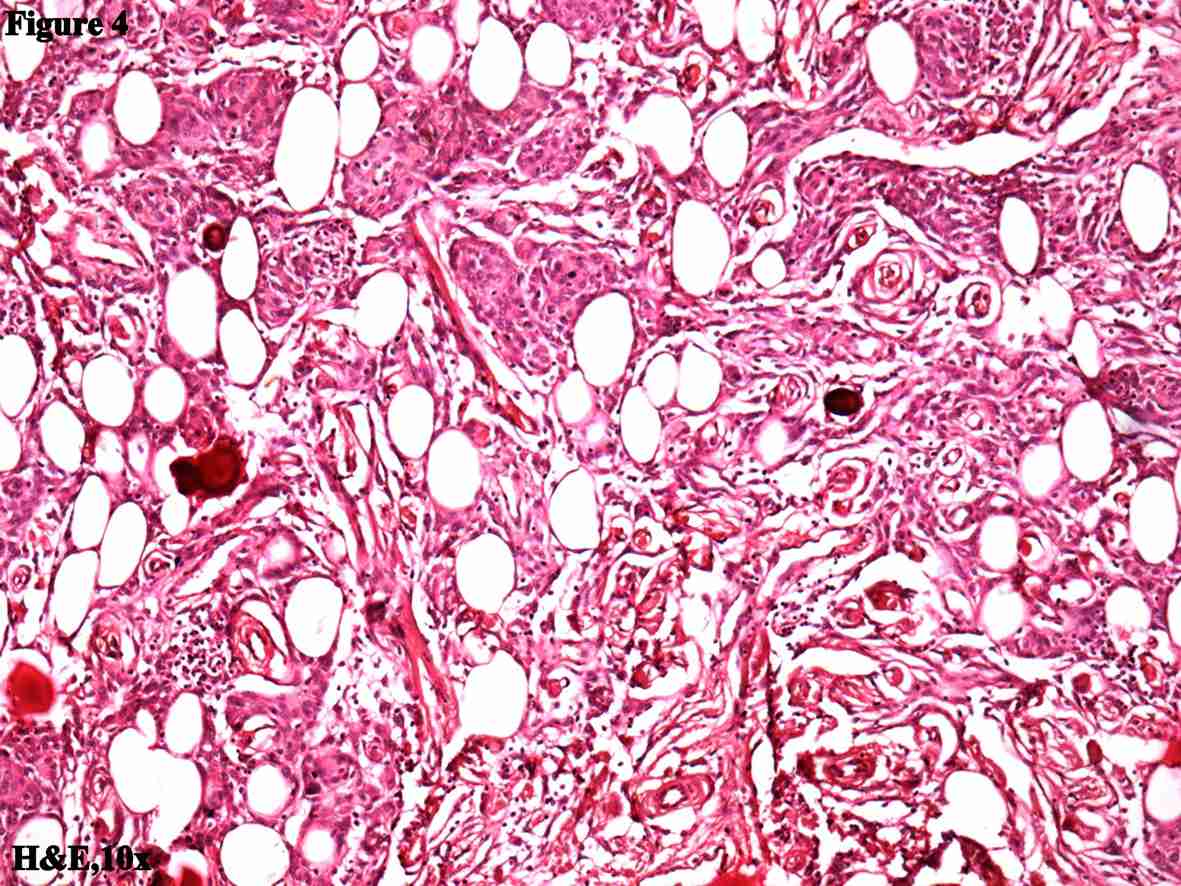
[Table/Fig-3, 4] (H andE stain- 4x, 10x): The tumour was composed of the fibroblastic, meningiotheliomatous and the transitional type patterns of meningiomas, with psammoma bodies and lipomatous changes. The tumour cells had infiltrated into the skull bone. There was no evidence of any mitotic figures or necrosis.
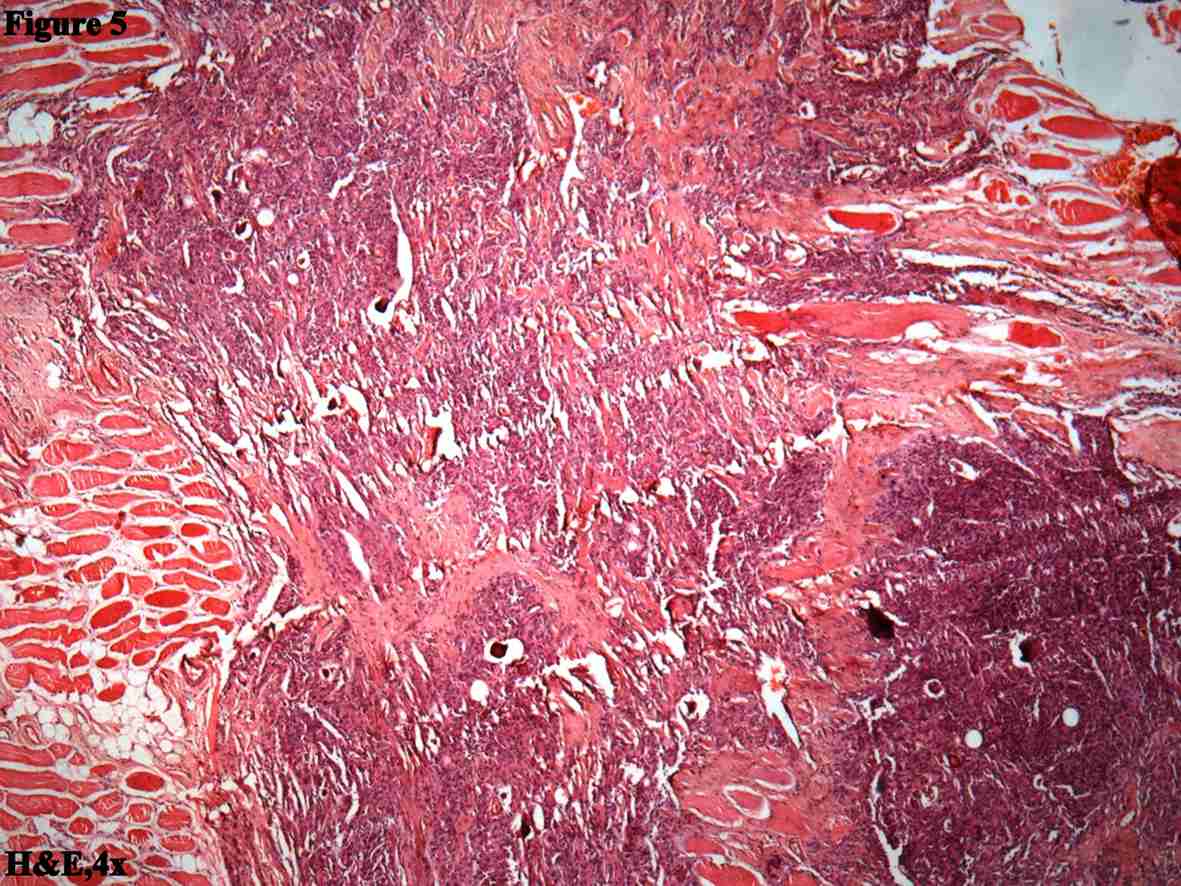
[Table/Fig-5] (H andE stain, 4x): The tumour cells had infiltrated into the skeletal muscles.
Though the histopapathological features were typical of a meningioma in our case, due to its unusual presentation, immunohistochemical studies were performed.
[Table/Fig-6] (IHC study)-The tumor cells showed strong cytoplasmic and membranous positivities for EMA and vimentin and a nuclear positivity for PR. The Ki-67(MIB-1, proliferation Index) positivity was 1-2%.
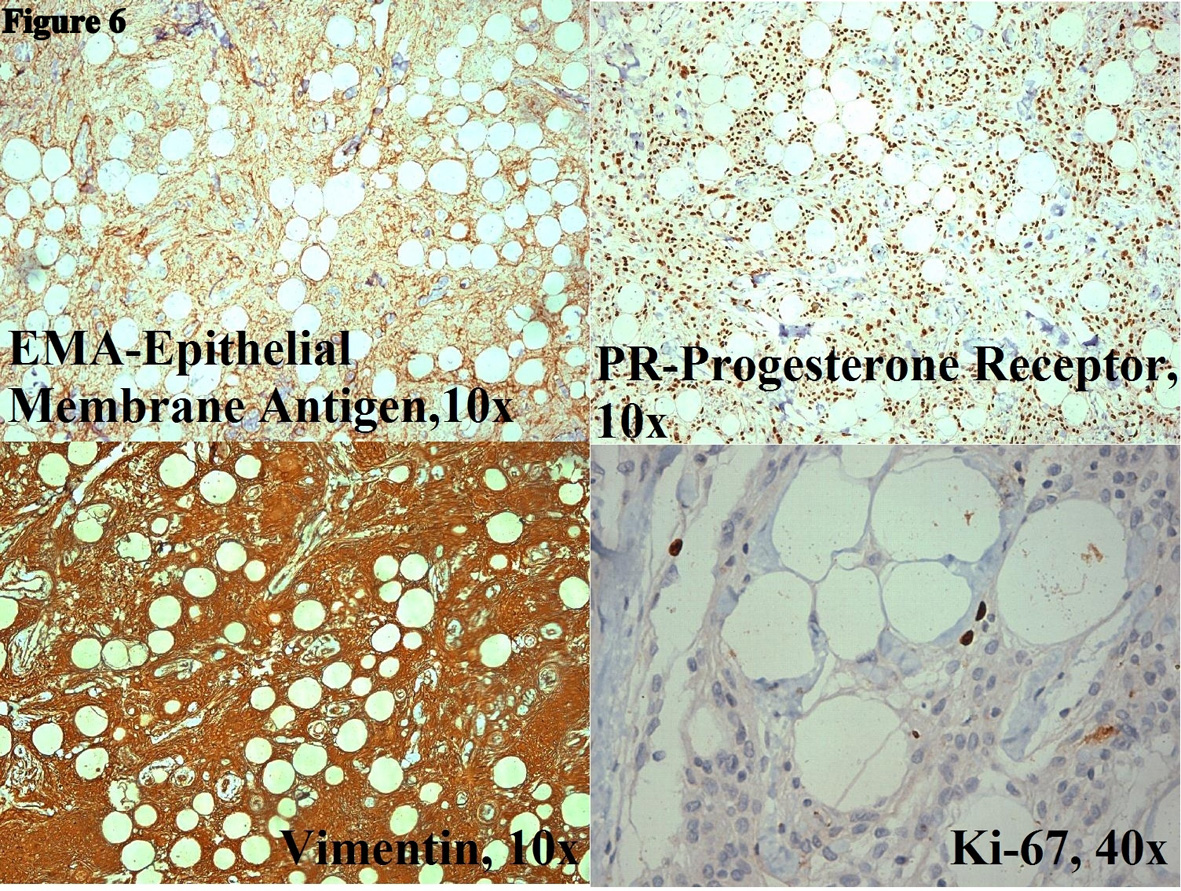
So, the diagnosis of an invasive meningioma with invasion of the muscle and the adipose tissue was given. A remark was written for an intracranial tumour sampling, to rule out a brain invasion, as well as for predicting the biological potential and the grading of the tumour.
A few days later, the surgical removal of the intracranial component was done, which revealed the same findings as have been mentioned above. Therefore, the final diagnosis of a meningioma of the WHO grade 1 was given. After 1year of follow up of the patient, there was no evidence of recurrence.
DISCUSSION
Meningioma is a common neoplasm of CNS. It commonly affects female during middle or later adult life and it comprises of approximately 24-30% of primary intracranial neoplasm [1].According to WHO (World Health Organization) / Mayo Clinic criteria [1], meningothelial tumors are classified in to three grades according to their biologic potential – Meningioma (WHO grade I), atypical meningioma (WHO grade II), and anaplastic meningioma (WHO grade III).
Primary intracranial meningioma usually arises in proximity to meninges, particularly in the parasagittal meninges, falx cerebri and sphenoid sphenoid ridges [2]. Origin [3–7] of arachnoid cells (meningothelial cells) is believed to be neural crest. They normally line the inner aspect of arachnoid membrane and fill the area of arachnoid villi that project into the lumens of dural veins and sinuses. The different mechanisms [3–6,8] are proposed for extracranial meningiomas occurrence:
Arachnoidal cells are present in the sheaths of nerves or vessels where they emerge through the skull foramina.
Displaced pacchionian bodies become detached, pinched off, or entrapped during embryologic development in an extracranial location.
A traumatic event or cerebral hypertension that displaces arachnoid location.
An origin from undifferentiated or multipotential mesenchymal cells.
Extracranial extension is rare. Shuangshoti [2] & Farr et al., [8] have reported prevalence of extracranial extension with primary intracranial meningioma to be 9% & 20% respectively. Orbit, outer table and scalp, paranasal sinuses and nasal cavity, parotid and parapharyngeal region are among the common sites for extracranial extension. Intracranial meningiomas with extracranial extension (secondary meningioma/invasive) have been reported in up to 20% of cases [5–7]. Extracranial spread of tumour can occur by various ways [2,7,9]. These are: Through foramina of skull, through the supraorbital fissure into the orbit, through the cribriform plate into the nasal cavities as well as nasopharynx, through floor of middle cranial fossa into paranasal sinuses and pterygoid region and through the suture line of the skull extracranial extension can occur.
Symptoms are usually non-specific and according to the anatomic site of involvement. Potential challenge in the diagnosis and treatment of invasive meningioma are present when they occur in region of head and neck, as presence in these sites often mimic other conditions in that region [8]. Therefore, high level of precision in diagnosing this extracranial – invasive meningioma is necessary. Depending upon the anatomic site of extracranial involvement, various differential diagnoses come into than can mimic like this entity clinically as well as radiologically. The main stay of diagnosis is by histopathological examination as well as by use of IHC studies.
IHC [10–13] has its diagnostic value in cases of anaplastic meningioma, variants mimics with other brain tumours like papillary, choroid , clear cell and meningioma with unusual location and presentation. EMA is the most commonly used marker in diagnosis of meningioma. It gives at least patchy positivity in most meningiomas. Most of the meningiomas express vimentin, an intermediate filament which has its own differential diagnostic value. Grade of the meningioma is inversely proportional to expression of PR, making its importance in diagnosis of borderline cases. Assessment of proliferative index with antibody MIB-1(Ki-67) is yet another important IHC marker, level of which correlates with the chances of recurrence. MIB-1 labeling indices more than 5% suggest a high likelihood of recurrence, so that it can be used as an additional tool to grade the borderline or atypical cases. Recently, mitosis-specific antibody against phosphohistone-H3 is found to be useful in meningioma grading. It has specific features of highlighting the mitotic figures which can help in searching mitotically active areas in the specimen and in differentiating mitoses from apoptotic nuclei. According to Saeed M Naguib et al., [12] claudin-1 is useful in differentiating fibrous meningiomas from morphologically similar other spindle cell tumors of the CNS like hemangiopericytoma, solitary fibrous tumors of meninges, and schwannoma.
According to one study [14], SPARC (also known as BM-40 and Osteonectin), is a potential diagnostic marker of invasive meningiomas and it can distinguish the histomorphologically benign non invasive from histomorphologically benign but invasive meningiomas, in absence of the infiltrative interface SPARC is a secreted, ECM (extra cellular matrix) - associated glycoprotein and is associated in modulation of cell adhesion, migration and angiogenesis. Its expression correlates with the invasive type.
Many benign and malignant tumors are included in clino-radiological differential diagnosis [3,6,7]. Extracranial meningioma can be misdiagnosed if the intracranial meningioma is missed. Paraganglioma, schwannoma and metastatic carcinoma come in differential diagnosis for primary ear and temporal bone meningioma. Aggresive psammomatoid ossifying fibroma for sinonasal tract lesion, dermatofibrosarcoma, melanoma, fibrosarcoma, leiomyosarcoma and synovial sarcoma for soft tissue and skin lesions mainly for grade II or III tumours as well as for non- meningothelial types of meningiomas. Specific histological feature, immunohistochemical markers and radiological findings of intracranial components are important in differentiating invasive meningioma from all these conditions.
The mainstay of treatment is total surgical removal [9,15] for most patients particularly at early stages. Prognosis of invasive meningioma is dependent on specific anatomic site, histological type, tumour grade, gender and age of patient. Overall prognosis is good [9,15,16]. The recurrence rate ranges from 7% to 84% depending upon the no. of years of follow up. It is similar to intracranial meningioma which have up to 20% recurrence rate [17,18].
In summary, our case is classical example of usual meningioma presents unusually by carpeting along with skull cap. So we proposed a term carpet meningioma for its presentation. Although it is grade I meningioma histologically, it still invades surrounding soft tissue and muscle. Therefore intrinsic aggressiveness must be present in these types of meningiomas. Moreover, these tumors are more often high grade despite no evidence of genetic abnormality as seen with atypical and anaplastic menigniomas. At this point, it is uncertain what causes invasiveness. As many benign and malignant tumors come in the differential diagnosis of this benign neoplasm, separation from other tumors is necessary as this entity has an excellent long term prognosis with only limited reported recurrence.
[1]. Perry A, Louis DN, Scheithauer BW, Budka H, von Deimling A, Meninigomas, In Louis DN, Ohgaki H, Wiestler OD, Cavenee WK (eds)WHO classification of tumors of the nervous system 2007 LyonIARC:164-72. [Google Scholar]
[2]. Perry A, Louis DN, Scheithauer BW, Budka H, von Deimling A, Meninigomas, In Louis DN, Ohgaki H, Wiestler OD, Cavenee WK (eds)WHO classification of tumors of the nervous system 2007 LyonIARC:164-72. [Google Scholar]
[3]. Shuangshoti S, Primary meningiomas outside the central nervous system. In Al-Mefty 0, edMeningiomas 1991 New YorkRaven Press:107-12. [Google Scholar]
[4]. Chang CY, Cheung SW, Jackler RK, Meningiomas presenting in the temporal bone: the pathways of spread from an intracranial site of originOtolaryngol Head Neck Surg 1998 119:658-64. [Google Scholar]
[5]. Farr HW, Gray GF, Vrana M, Panio M, Extracranial meningiomaJ Surg Oncol 1973 5:411-20. [Google Scholar]
[6]. Batsakis JG, Pathology consultation. Extracranial meningiomasAnn Otol Rhinol Laryngol 1984 93:282-83. [Google Scholar]
[7]. Friedman CD, Costantino PD, Teitelbaum B, Berktold RE, Sisson GA Sr, Primary extracranial meningiomas of the head and neck Laryngoscope 1990 100:41-48. [Google Scholar]
[8]. Thompson LD, Bouffard JP, Sandberg GD, Mena H, Primary ear and temporal bone meningiomas: a clinicopathologic study of 36 cases with a review of the literatureMod Pathol 2003 16:236-45. [Google Scholar]
[9]. Thompson LD, Gyure KA, Extracranial sinonasal tract meningiomas. a clinicopathologic study of 30 cases with a review of the literatureAm J Surg Pathol 2000 24:640-50. [Google Scholar]
[10]. Granich MS, Pilch BZ, Goodman ML, Meningiomas presenting in the paranasal sinuses and temporal boneHead Neck Surg 1983 5:319-28. [Google Scholar]
[11]. Theaker JM, Gatter KC, Esiri MM, Fleming KA, Epithelial membrane antigen and cytokeratin expression by meningiomas: an immunohistological studyJ Clin Pathol 1986 39:435-39. [Google Scholar]
[12]. Meis JM, Ordonez NG, Bruner JM, Meningiomas. An immunohistochemical study of 50 casesArch Pathol Lab Med 1986 110:934-37. [Google Scholar]
[13]. Naguib Saeed M, Shalaby Ahmad M Ragab, Differentiation of meningiomas from histologic mimics via the use of claudin-1 Pan ArabJ Neurosurg 2008 12(1):10-14. [Google Scholar]
[14]. Riemenschneider Markus J, Perry Arie, Reifenberger Guido, Histological classification and molecular genetics of meningiomasLancet Neurol 2006 5:1045-54. [Google Scholar]
[15]. Naguib Saeed M, Shalaby Ahmad M Ragab, Differentiation of meningiomas from histologic mimics via the use of claudin-1 Pan ArabJ Neurosurg 2008 12(1):10-14. [Google Scholar]
[16]. Rempel SA, Ge S, Gutiérrez JA, SPARC: A potential diagnostic marker of invasive meningiomasClinical Cancer Research 1999 5:237-41. [Google Scholar]
[17]. Mirimannoff RO, Dosoroetz DE, Linggood RM, Ojemann RG, Martuza RL, Meningioma: analysis of recurrence and progression following neurosurgical resectionJ Neurosurg 1985 62:18-24. [Google Scholar]
[18]. Stafford SL, Perry A, Suman VJ, Meyer FB, Scheithauer BW, Lohse CM, Primarily resected meningiomas: outcome and prognostic factors in 581 Mayo Clinic patients, 1978 through 1988Mayo Clin Proc 1998 73:936-42. [Google Scholar]