Fine needle aspiration (FNA), which is used in the setting of thyroid lesions, is widely considered to be a rapid, cost-effective, safe and a reliable tool of evaluation, especially in euthyroid patients with thyroid nodules. The application of thyroid FNA has been documented with the reduction of unnecessary thyroid surgeries in patients with benign thyroid nodules and it has resulted in a four fold increase in the resection of malignant nodules in comparison to that which was seen in the pre FNA era [1–3].
In the past; lack of ambiguity, standardization and the failure of the treating physician to interpret the cytological findings in many cases, had led to confusion and frustration in the sharing of clinically meaningful data between the physicians and even between inter and intra institutions, as the terminology tended to differ from one pathologist to the other and also between different laboratories [3, 4].
To achieve the standardization of the thyroid FNA reporting, the National Cancer Institute (NCI) hosted the ‘NCI Thyroid Fine Needle Aspiration State of the Science Conference’ which led to the formation of ‘The Bethesda System for Reporting Thyroid Cytopathology’ (TBSRTC) [5, 6].
The present study was undertaken by 2 experts in thyroid FNA, who in a double blinded fashion, examined and re-classified 80 random FNA cases according to the 6 levels of TBSRTC for an inter-observer review, to study and assess the new terminology for ease of reproducibility and to note the rate of disagreement overall or in any particular category.
MATERIAL AND METHODS
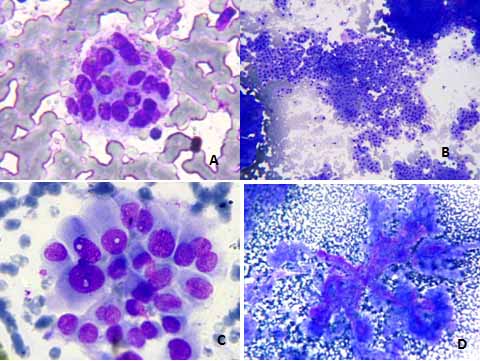
The present study was conducted in the Department of Pathology by 2 cytopathologists who had specialized in thyroid FNA, on 80 random past cases which were retrieved from the archives of the cytopathology unit, which had a non TBSRTC diagnosis but with histopathological correlations. Both the experts were using previous terminologies but they understood and were well versed with TBSRTC. The FNAs were reclassified in a double blinded fashion according to the 6 levels of TBSRTC which are: non diagnostic (ND); benign; atypia of undetermined significance/follicular lesion of undetermined significance (AUS/FLUS); follicular neoplasm/suspicious for a follicular neoplasm (FN/SFN), with those of the Hurthle cell type which were reported as follicular neoplasms, Hurthle cell type/suspicious for a follicular neoplasm, Hurthle cell type (FNHCT/SFNHCT); suspicious (SUS), and malignant [5, 7]. [Table/Fig-1A-D]
Cytolomorphological findings seen in various categories of The Bethesda System of Reporting Thyroid Cytopathology (TBSRTC) A: Category Atypia of undetermined significance/follicular lesion of undetermined significance (AUS/FLUS); [MGG 400 X] B: Category Follicular neoplasm, Hurthle cell type suspicious for a follicular neoplasm, Hurthle cell type (FNHCT/SFNHCT) [MGG 100 X] C: Category suspicious (SUS) [MGG 400 X] D: Category Malignant [MGG 100 X]
Both the experts were given the original relevant clinical and radiological details which were also retrieved from the archives. The findings were noted and they were tabulated in a systematic manner. Statistically, the degree of reproducibility was estimated in the form of percentage of agreement, disagreement and no consensus in re-classifying the thyroid lesions. Additionally, an effort was made to analyze whether any particular category had a greater degree of disagreement and to rationalize the probable reasons for that.
RESULTS
In the present study, the maximum number of cases was reclassified under the benign category (61.25% cases), followed by the FN/ SFN category and the AUS/FLUS category (11.25% and 10.00 % respectively) [Table/Fig-2]. An agreement was reached in 66 cases (82.5 %). The experts disagreed in 14 (17.5%) cases (where 1 expert did not agree with the other) [Table/Fig-3].
Reclassifying the thyroid lesions according to the categories described in the Bethesda System of Reporting Thyroid Cytology (TBSRTC)
| Category | | Percentage prevalence |
|---|
| ND | 01 | 01.25 |
| BENIGN | 49 | 61.25 |
| AUS/FLUS | 08 | 10.00 |
| FN/SFN | 09 | 11.25 |
| FNHCT/SFNHCT | 07 | 08.75 |
| SUS | 03 | 03.75 |
| MALIGNANT | 03 | 03.75 |
| TOTAL | 80 | |
ND-Non Diagnostic; AUS/FLUS-Atypia of Undetermined Significance/Follicular Lesion of Undetermined Significance; FN/SFN-Follicular Neoplasia/Suspicious of Follicular Neoplasia; FNHCT/SFNHCT-Follicular Neoplasia Hurthle Cell Type/Suspicious of Follicular Neoplasia Hurthle Cell Type; SUS-Suspicious of malignancy.
Comparison of reclassified lesions according to TBSRTC between experts as agreement versus disagreement (Expert 1-horizontal and Expert 2-Vertical)
| Category According to Experts | According to Expert 1 |
|---|
| ND | Benign | AUS/FLUS | FN/SFN | FNHCT/SFNHCT | SUS | Malignant | Total |
|---|
| According to Expert 2 | ND | 01 | | | | | | | 01 |
| Benign | | 46 | 03 | 02 | 02 | | | 53 |
| AUS/FLUS | | 01 | 04 | | | | | 05 |
| FN/SFN | | 01 | | 06 | | | | 07 |
| FNHCT/SFNHCT | | 01 | 01 | | 05 | | | 07 |
| SUS | | | | 01 | | 02 | | 03 |
| Malignant | | | | | | 01 | 03 | 04 |
| Total | 01 | 49 | 08 | 09 | 07 | 03 | 03 | 80 |
Cases which were discordant (Disagreement) are in bold.
ND-Non Diagnostic; AUS/FLUS-Atypia of Undetermined Significance/Follicular Lesion of Undetermined Significance; FN/SFN-Follicular Neoplasia/Suspicious of Follicular Neoplasia; FNHCT/SFNHCT-Follicular Neoplasia Hurthle Cell Type/Suspicious of Follicular Neoplasia Hurthle Cell Type; SUS-Suspicious of malignancy.
There was a complete agreement on a single ND case which was previously diagnosed as a colloid cyst [3]. Cases in the benign category which were discordant between both the experts were either put in the category AUS/FLUS, FN/SFN or FNHCT/ SFNHCT. All these discordant cases were previously diagnosed as hyperplastic nodular goitre, multi-nodular goitre or as adenomatous goitre by a non TBSRTC system [Table/Fig-3].
Of the 8 cases in the category AUS/FLUS; in 4 cases, there was disagreement (3 cases kept under benign category and 1 case kept under the category FNHCT/SFNHCT [Table/Fig-3]. In the category FN/SFN, 3 cases were discordant out of total 9 cases. The cases in which the disagreement took place were either kept under the benign category (2 cases) or 1 case which was kept under suspicious (SUS) category [Table/Fig-3].
Among the 7 cases which were finally kept in the category, FNHCT/SFNHCT; on 2 cases, consensuses were not reached between the experts and these 2 cases were categorized under the benign category by the discordant cytopathologist [Table/Fig-3]. In 2 cases out of 3 complete agreement was recorded with 1 case kept under malignant category by one of the experts. [Table/Fig-3]. There was a universal consensus in all the 3 cases of malignant lesions, with no disagreement between the 2 experts [Table/Fig-3]. In the end, there was a 93.87% agreement for the lesions in the benign category, for 50% cases in the AUS/FLUS category, for 66.66% cases in the FN/SFN and the SUS categories, for 71.42% cases in the FNHCT/ SFNHCT categories and for 100% cases in the ND and the malignant categories. Thus, the maximum disagreement was noted in the category, AUS/FLUS [Table/Fig-3].
DISCUSSION
The reporting of thyroid FNA suffers from usage of “personalized”, local, institutional and descriptive terminologies [6]. For example the diagnoses in the case of benign thyroid lesions in the present case series were given as colloid goitre, multi-nodular goitre, adenomatous hyperplasia, adenomatous goitre with hyperplastic nodules, hyperplastic nodular goitre and colloid cyst by various pathologists at different centres.
The TBSRTC system was the end result of a 2 day meet of over 150 cytopathologists, surgical pathologists, endocrinologists, radiologists and surgeons who had an avid interest in the field of thyroid disease, to put in place, a universal reporting system through which cytologists and physicians could understand each other and could help in predicting the prognosis by estimating the malignant potential of the individual category [5, 8, 9].
The TBSRTC system is presently being widely used in the United States and in several European countries, but it still has to go a long way in getting acceptability in many countries of Asia (including India) and Africa.
Prevalence wise, the maximum number of cases which were reclassified in the present study were in the benign category (61.25% cases), followed by the FN/ SFN category and the AUS/FLUS category (11.25% and 10.00 % respectively). This corroborates with the work which was done by other authors regarding the incidence of benign lesions (range-54-77.4%) considerably more than that of the malignant lesions. (Range-2-7%). The AUS/FLUS diagnosis shows a wide variability (range of 0.7-18%) by different researchers [9].
As in other studies, the categories under which the maximum degree of agreements noted were- non diagnostic, malignant and benign [6, 9].
Diagnostic disagreements were seen maximally in the AUS/FLUS and the FN/SFN categories. Exactly half of the cases in the AUS/FLUS category were discrepant, with the maximum number of these cases categorized as benign by one of the experts. In one of the case, the presence of few Hurthle cells prompted one of the experts to classify the lesion as FNHCT/SFNHCT. In the FN/SFN category, the 2 discrepant cases were categorized as benign by one of the experts, whereas 1 case was deemed as suspicious due to the presence of few cell clusters which had abnormal nuclei.
Various studies have highlighted this phenomenon as the presence of micro-follicular structures and their number may warrant a diagnostic variation from AUS/FLUS to FN/SFN. Studies have also stressed that this criteria is often not in agreement between the cytologists who review the same case, which leads to these discrepancies. Although these criteria are very well described, oft quoted, well illustrated and detailed in the print atlas and are a point which “stimulates” discussions in the department; the fact remains that it is strongly recommended that every cytopathologist needs specific training and the opportunity to compare the histological controls, whenever and wherever they are available, to distinguish between these 2 categories [6, 9–12].
This is important more so, as it was concluded in a very recent study, that the rates of the AUS/FLUS category should not exceed the recommended target of 7%, as the AUS rates and the malignant outcomes are inversely related: the higher a cytopathologists’s AUS rate, the lower is the rate of malignancy for that AUS cohort [13].
An interesting yet universally concluded fact in the cases of discrepancy between the AUS/FLUS rate versus the FN/SFN categories and the increased AUS rates, was that no correlation could be calculated between these and the cytopathologists’ experience or the thyroid FNA volume [11, 13].
In conclusion; though there was a great deal of agreement in the implementation of TBSTRC in the present study; disagreements were seen in the categories of AUS/FLUS and FN/SFN in the study which was conducted at our centre. This corroborated with the findings of the studies which were done elsewhere [13–15].
It was also concluded in our study, that the implementation of TBSTRC, which stands for a unique, international and a universal terminology for the reporting of the thyroid cytology; should be encouraged in our country, because its relative ease of reproducibility can make a “single voice” reality in the field of thyroid cytology, as many “voices and babbles (diagnosis)” sometimes confuse not only the treating physicians but also the cytologists who work at the same centre. This is possible by holding scientific seminars/CME/ workshops throughout the country by the scientific committees of the governing bodies of pathologists in India and by informing the affiliated pathologists and the societies about the TBSRTC system, its terminology and its guidelines.
An additional point which is in favour of the implementation of this system is that the classification is directly related to the risk of malignancy in each category [6, 16, 17], which in turn, prompts the recommended clinical management of that category, thus truly embodying the clinic-pathological correlation in its true spirit.
ND-Non Diagnostic; AUS/FLUS-Atypia of Undetermined Significance/Follicular Lesion of Undetermined Significance; FN/SFN-Follicular Neoplasia/Suspicious of Follicular Neoplasia; FNHCT/SFNHCT-Follicular Neoplasia Hurthle Cell Type/Suspicious of Follicular Neoplasia Hurthle Cell Type; SUS-Suspicious of malignancy.
Cases which were discordant (Disagreement) are in bold.ND-Non Diagnostic; AUS/FLUS-Atypia of Undetermined Significance/Follicular Lesion of Undetermined Significance; FN/SFN-Follicular Neoplasia/Suspicious of Follicular Neoplasia; FNHCT/SFNHCT-Follicular Neoplasia Hurthle Cell Type/Suspicious of Follicular Neoplasia Hurthle Cell Type; SUS-Suspicious of malignancy.