Internal Jugular Phlebectasia: Diagnosis by Ultrasonography, Doppler and Contrast CT
Manash Kumar Bora1
1 Associate Professor, Department of Radiology, Aarupadai Veedu Medical College and Hospital, Pondicherry-605001, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Manash Kumar Bora, Associate Professor, Department of Radiology, Second Floor, Vishram Apatment, Door No.4, S.V. Patel Salai, Pondicherry, 605001, India.
Phone: 978730091
E-mail: drmanashbora@yahoo.com
Jugular phlebectasia is an isolated saccular or fusiform dilation of a vein without tortuosity. Its aetiology remains controversial. It is infradiagnosed, as it is generally asymptomatic. However, it has been increasingly recognized in recent years due to the better imaging techniques which are available. Phlebectasia of the Internal Jugular Vein (IJV) is a rare disease. It is mostly unilateral and it involves only the right side. It is usually a childhood disease which is diagnosed during the study of an intermittent neck mass. Its treatment is controversial. Presently, a conservative approach to unilateral or bilateral asymptomatic phlebectasia is recommended. Symptomatic phlebectasia requires surgery. The diagnosis is suggested by clinical features which can be confirmed by noninvasive radiology. This paper is reporting a case of unilateral right internal jugular phlebectasia in a 12 year old female patient who complained of an intermittent, right sided neck swelling, where we used UltraSonoGraphy(USG) with Doppler and Contrast enhanced CT(CECT) to evaluate the lesion.
Phlebectasia, Internal jugular vein, Contrast enhanced CT, USG Doppler
INTRODUCTION
Phlebectasia is the abnormal sacculofusiform dilatation (without tortuosity) [1] of a vein, which may affect any vein [2]. Its aetiology remains unknown [3] and it is seen usually in the paediatric age group as a unilateral lower neck swelling, mostly on the right side [4]. The other differential diagnoses of the neck swellings which increase in size during a Valsalva manoeuvre are tumours or cysts of the upper mediastinum, external laryngeal diverticulae or laryngoceles [5].Our case report has highlighted the importance of understanding the nature of this lesion by using non invasive radiological diagnostic modalities (USG, Doppler and CECT), in order to avoid invasive investigations which can lead to catastrophic results.
CASE HISTORY
A 12 year old female child came with an intermittent right sided neck swelling which had been observed by her mother for the past six months. Her examination at rest was normal. However, with the Valsalva maneouver a soft, painless, compressible swelling which appeared in the right lower neck was seen, which was not attached to the deep structures [Table/Fig-1]. No murmurs or fremitus were detected.
Photograph showing prominent swelling in the right lower neck on valsalva manoeuvre

There was no history of trauma. The systemic examination and the laboratory tests were normal. The patient was referred for CECT of the neck and a provisional diagnosis of a laryngocoele was made.
We evaluated the case first with ultrasound and Doppler, followed by CECT.
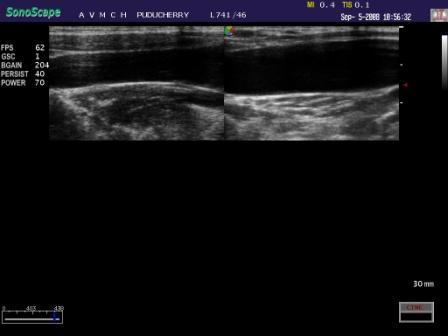
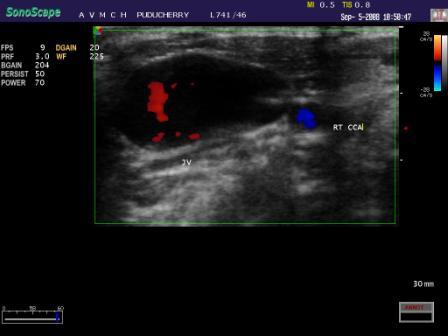
USG (Sonoscape-4400, 7.5 MHz linear probe) at rest, revealed a mildly dilated IJV as compared to that on the opposite side [Table/Fig-2]. On Valsalva manoeuvre, the right IJV was found to be increased in size to 3 cm x 5 cm [Table/Fig-3]. Colour Doppler revealed a complete luminal filling of the vein with intermittent aliasing, which suggested turbulence. Spectral tracing showed slow and flat wave forms which were typical of the venous flow.Compared to the opposite side, the phasic variation at rest was found to be amplified in the affected right side, which dampened with the Valsalva manoeuvre.
Gray Scale USG image showing mildly dilated right internal jugular vein (left image) compared to other side
USG with Doppler image showing enlargement of the right internal jugular vein on valsalva manoeuvre
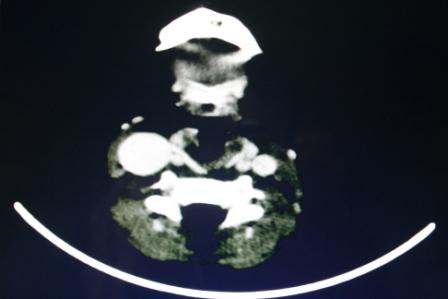
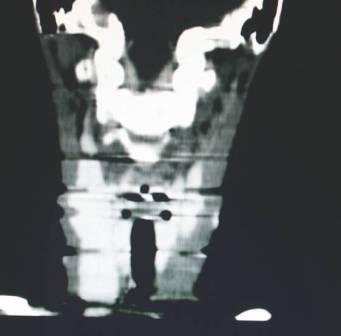
CECT while patient performing valsalva manoeuvre was done with (Toshiba Asteoin V1.71ER004 Spiral CT), with a slice thickness of 3mm, a collimation of 3mm, a pitch of 1.2 and Multi Planar Reconstructions (MPR). The axial images showed a dilated right IJV which measured 3 x 3 cm [Table/Fig-4]. MPR showed the large fusiform swelling to be the right IJV which had extended from the superior aspect of the right clavicle to the infrahyoid region, which measured 3 x 3 x 5 cm [Table/Fig-5 & 6]. Above and below, the vein was of normal calibre.
Contrast CT axial image showing enlarged right internal jugular vein
Multiplanar reconstructed Images –sagittal image showing enlarged right internal jugular vein
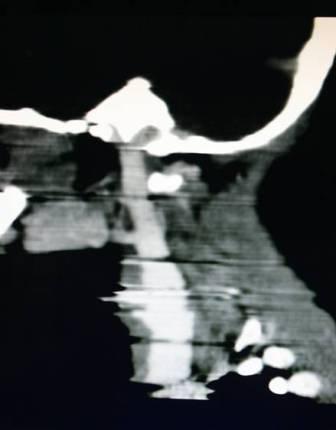
Multiplanar reconstructed Images –coronal image showing enlarged right internal jugular vein
As the patient did not have any complications, a conservative treatment was offered. The patient is now on regular follow up for the past one year.
DISCUSSION
Venous dilatation was first reported in 1928 [6] and phlebectasia was the term which was used by Gerwig [1] to describe an abnormal fusiform dilatation of a vein.
Synonyms include venous aneurysm, venous congenital cyst, venous ectasia or an essential venous dilatation. It can affect any vein [2]. Its aetiology remains unknown [3]. Histopathological studies have shown loss of the elastic layer and hypertrophy of the connective tissue, with focal intimal thickening [6]. It has been increasingly recognized in the recent years due to the better imaging facilities.
Phlebectasia has been reported in a wide age interval (ranging from 5 months to 68 years), being more frequent among paediatric patients, especially among those who are below 13 years of age [7].
Cervical swelling is a common diagnostic problem in paediatric patients. The differential diagnosis for the masses which appear on the Valsava manoeuvre includes laryngocele, external laryngeal diverticulae, pharyngocele, neumocele, a superior mediastinal cyst or a tumour [3, 5] and venolymphatic malformations, with laryngocele being the commonest [8]. Jugular phlebectasia is one such cause, with its incidence being higher on the right side [4]. Complications like a thrombus, a pulmonary embolism, a spontaneous rupture and thrombophlebitis may occur, with pulmonary embolism being the most serious one. Its non-invasive diagnosis can be achieved by using ultrasonography with Doppler, CECT,CT Angiography and MR Venography [9].
Ultrasonography with Doppler before, during and after the Valsalva manoeuvre is the preferred method for the diagnosis [10].
Duplex sonograms which show flat waves indicate that the swelling is of venous origin [11]. In our case, we got an intermittent turbulent flow on colour Doppler. The Doppler study also showed that the amplitude of the phasic variation was more prominent on the affected right side at rest, and that it decreased with the Valsalva maneouver.
Ultrasound is an accurate and a readily reproducible imaging technique in this condition, which defines its extent and its relationship with the other structures in the neck [12].
CECT has equal diagnostic capability for evaluating this lesion, as in our case. Its advantage is that the adjacent deeper structures of the neck can be better defined, which may not be readily accessible by a high frequency ultrasound probe. Previous reports have stated that CT and Biphasic CT angiography with MPR and maximum intensity projection are very sensitive and that they demonstrate the vascular anomaly clearly [9, 13].
Surgery is not recommended for this benign condition and a conservative follow up is required [14]. However, in symptomatic patients or in those with complications, resection of the dilated segment or covering with the muscular segment is recommended [15].
CONCLUSION
Very few cases of Internal jugular phlebectasia have been reported till date, due to the rarity of this condition and because they are mostly infradiagnosed. A clinical diagnosis can be achieved by having a strong suspicion about this intermittent neck mass. It should be evaluated with non invasive radiological modalities to avoid the possible catastrophic results which result from invasive techniques.
A conservative management is offered for this benign condition in asymptomatic patients. Surgery is reserved for the symptomatic cases or in the presence of complications.
[1]. WH Gerwig, Jr, Internal jugular phlebectasiaAnnals of Surgery 1952 135:130-33. [Google Scholar]
[2]. Gilbert MG, Greenberg LA, Brow WT, Fusiform venous aneurysm of the neck in children: a report of four casesJ Paediatr Surg 1972 7:108-11. [Google Scholar]
[3]. Hu X, Li J, Hu T, Jiang X, Aneurism of the internal jugular veinAm. J. Otolaringol. Head Neck Med. Surg 2005 26:172-74. [Google Scholar]
[4]. Paleri V, Gopalakrishman G, Jugular phlebectasia: theory of pathogenesis and review of literatureInt. J. Pediatr. Otorhinolaryngol 2001 57:155-59. [Google Scholar]
[5]. La Monte SJ, Walker EA, Moran WB, Internal jugular phlebectasia. A clinicoroentgeographic diagnosisArch Otolaryngol 1976 102:706-08. [Google Scholar]
[6]. Yokomori K, Kuba K, Kanamori Y, Takemura Internal jugular plebectasia in two sublings: manometric and histopathologicJ Pediatr Surg 1990 25:762-65. [Google Scholar]
[7]. Margarita Escudero Lirio, Isabel Delgado Pecellín, MacarenaTaguas Castaño, Maria Teresa Alonso Salas, Mercedes Loscertales Abril, Int J Pediatr Otorhinolaryngol 2008 3:03-09. [Google Scholar]
[8]. Harris RI, Congenital venous cyst of mediastinumAnn Surg 1928 88:953-56. [Google Scholar]
[9]. Desai SJ, Rajan S, Jain T, Anterior jugular vein aneurysm : Diagnosis by CT angiographyIndian J Radiol Imaging 2002 12:369-70. [Google Scholar]
[10]. Gribbin C, Raghavendra BN, Ginsburg HB, Ultrasound diagnosis of jugular venous ectasiaNew York State J Med 1989 89:532-33. [Google Scholar]
[11]. Lin MJ, Chou YH, Liu CM, Duplex Doppler ultrasound of internal jugular vein ectasia: A case report.Chung Huai I Hsulh Tsa Chih—ChinMed J 1990 46:190 [Google Scholar]
[12]. Stevens RK, Fried AK, Hood TR Jr, Ultrasonographic diagnosis of jugular venous aneurysmJ Clin Ultrasound 1982 10:85 [Google Scholar]
[13]. Som PM, Shugar JMA, Sacher M, Internal jugular vein phlebectasia and duplication: CT featuresJ Comput Assist Tomogr 1985 9:390 [Google Scholar]
[14]. Bowdler DA, Singh SD, Internal Juguler phlebectasiaInt J Pediatr Otorhinolaryngol 1986 12:165-71. [Google Scholar]
[15]. Ferreira Lidiane Maria de Brito Macedo, Haguette Erik Frota, Bilateral Internal Jugular PhlebectasiaInternational Archivesof Otorhinolaryngology 2007 11:21 [Google Scholar]